Professional Documents
Culture Documents
Dos 416 Week 2 Discussion
Uploaded by
api-210258673Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
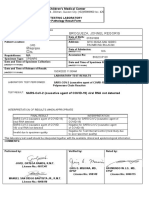
Dos 416 Week 2 Discussion
Uploaded by
api-210258673Copyright:
Available Formats
It is known beyond a shadow of a doubt that x-rays are harmful.
If sufficiently intense, x-rays can cause hematologic, gastrointestinal, and central nervous system disorders; local tissue damage; cytogenetic impairment (which are considered as an early effect of radiation). Late effects of radiation on humans would include leukemia, bone cancer, lung cancer, thyroid cancer, breast cancer, genetic damage and shortening of life span.1 However, the benefits resulting from applications of x-rays are enormous and often outweigh potential risks. It is the job of the radiation oncology multidisciplinary team to perform high- quality radiation therapy procedures with minimal radiation exposure to patients healthy tissues. This attitude results in the highest benefit with the lowest risk to patients and radiation workers, and its a foundation of the practice of ALARA as low as reasonably achievable.1 In 1994 the ALARA document became a part of title 10f the Code of Federal Regulations (10CFR35.20) which is binding on all institutions as a NRC regulation. Therefore, it must be practiced as a matter of mandate of federal code. Given the complexity of a radiotherapy practice, patients safety depends largely on human performance and training. Therefore, to ensure general public safety, educated and trained professionals are an essential prerequisite for quality and safety in radiotherapy. All of the following individuals have responsibility for public protection and safety by virtue of tasks involving decisions, operation or manipulation of sources or equipment used in radiotherapy: radiation oncologists; qualified experts in radiotherapy physics - medical physicists and dosimetrists; other health professionals operating radiotherapy equipment or handling radioactive sources (radiotherapy technologists); the Radiation Safety Officer; staff for maintenance of radiotherapy equipment; staff performing special tasks (type tests, long term stability checks, etc.) Moreover, the evidence is required of education and training relevant to their duties in relation to protection and safety. Responsibility for the practice of radiotherapy requires accreditation by the professional body (like Nuclear Regulatory Commission, International Council on Radiation Protection, and Committee on Biologic effects of Ionizing Radiation) or an educational institution2. The main task of all of these
institutions and trained professionals is to ensure public that their general safety is not a worry. According to an article published by the University of Maryland Cancer Center, radiation therapy is by far one of the safest and most effective forms of cancer treatment.3 As noted in the article, radiation therapy actually has an extremely low rate of errors, due to the many checks currently in place to ensure patient safety. An estimated 35 million treatments were administered last year on equipment made by Varian Medical Systems alone, with about 70 instances of mistakes that affected or nearly affected patient care. Most of the errors were associated with the lack of quality assurance processes. To eliminate that problems, and consequently to ensure patient safety, most of cancer centers follow a comprehensive set of safety rules. These include: 1) machine-related QA checks, including a daily check of the beam output and monthly physics checks of all equipment; 2) secondary calculations to verify the accuracy of the radiation dose calculated by our treatment planning systems; 3) a review of all treatment plans by medical physicists; 4) quality assurance checks of Intensity Modulated Radiation Therapy (IMRT) plans prior to treatment; 5) review by the therapist staff to verify agreement between the radiation dose in the treatment plan and the treatment console; and 6) verification of the physician's written directive, the prescribed dose and the patient's identity. Even though in the past few years several cases of cancer patients over-exposure were recorded across the United States, general public has no reason to worry. The field of Radiation Oncology is strictly governed by many professional institutions (which ensure radiation safety practices) and employs educated and trained in radiation safety personnel. Moreover, comprehensive set of safety rules are rigorously utilized, to verify accuracy of the radiation dose.
References: 1) Joseph, Nicolas Jr., Phalem Jeffrey. CE Essentials, LLC. Cardinal Principles of Radiation Protection. 2006. Available at: http://www.ceessentials.net/article3.html. Accessed at: October 1, 2011. 2) International Atomic Energy Agency. Applying Radiation Safety Standards in Radiotherapy. 2006. available at:
http://www-pub.iaea.org/MTCD/publications/PDF/Pub1205_web.pdf. Accessed at: October 1, 2011. 3) University of Maryland Greenebaum Cancer Center. Radiation Therapy and Patient Safety. 2011. Available at: http://www.umgcc.org/news/rt_safety.htm. Accessed at: October 1, 2011.
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Diversity 2Document3 pagesDiversity 2api-210258673No ratings yet
- Dos 514 Practice Problems 2Document8 pagesDos 514 Practice Problems 2api-210258673No ratings yet
- Flow ChartDocument2 pagesFlow Chartapi-210258673No ratings yet
- Resarch UpdatedDocument48 pagesResarch Updatedapi-210258673No ratings yet
- Transmission Factor CalculationDocument9 pagesTransmission Factor Calculationapi-2102586730% (1)
- March Case StudyDocument7 pagesMarch Case Studyapi-210258673No ratings yet
- February Case StudyDocument6 pagesFebruary Case Studyapi-210258673No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Lecture - 7 - Work - Capacity, - Stress - and - Fatigue (Autosaved)Document51 pagesLecture - 7 - Work - Capacity, - Stress - and - Fatigue (Autosaved)Aizat RomainoNo ratings yet
- Conducting A Nurse Consultation: ClinicalDocument6 pagesConducting A Nurse Consultation: ClinicalAlif Akbar HasyimiNo ratings yet
- List of Anesthetic, Analgesic and Tranquilizer Drugs Veterinary)Document25 pagesList of Anesthetic, Analgesic and Tranquilizer Drugs Veterinary)drbadman77100% (2)
- Pfizer Vaccine Explainer Version 2Document9 pagesPfizer Vaccine Explainer Version 2nqosa neidscqNo ratings yet
- Rent AgreementDocument4 pagesRent Agreementkhushbu chitreNo ratings yet
- Lesson 3 - The Circulatory and Respiratory SystemsDocument26 pagesLesson 3 - The Circulatory and Respiratory SystemsEmieleah Lorenzo PauigNo ratings yet
- Blood PressureDocument25 pagesBlood PressureSilvia FrtNo ratings yet
- QCLI DictionaryDocument129 pagesQCLI DictionarysenorvicenteNo ratings yet
- Chronic PeriodontitisDocument3 pagesChronic Periodontitisapi-537687828No ratings yet
- Subacute Bacterial Endocarditis and Antimicrobial ProphylaxisDocument42 pagesSubacute Bacterial Endocarditis and Antimicrobial Prophylaxisalex-pham-2258No ratings yet
- Mia SmsDocument8 pagesMia SmsGlasiNo ratings yet
- Peripheral NeuropathyDocument30 pagesPeripheral NeuropathyLyn LynNo ratings yet
- Serious Adverse Events of Special Interest Following mRNA COVID-19 Vaccination in Randomized Trials in AdultsDocument9 pagesSerious Adverse Events of Special Interest Following mRNA COVID-19 Vaccination in Randomized Trials in AdultsLilianneNo ratings yet
- 30613167: Management of Osteitis Pubis in Athletes Rehabilitation and Return To Training - A Review of The Most Recent Literature PDFDocument10 pages30613167: Management of Osteitis Pubis in Athletes Rehabilitation and Return To Training - A Review of The Most Recent Literature PDFRicovially DavyaNo ratings yet
- Case Study 7 - Antepartum BleedingDocument2 pagesCase Study 7 - Antepartum BleedingRahul Tharwani100% (1)
- Piperacillin TazobactamDocument2 pagesPiperacillin TazobactamAnonymous43% (7)
- Nguyen 2021Document8 pagesNguyen 2021Yaseen MohamnadNo ratings yet
- Fundamentals of NursingDocument44 pagesFundamentals of Nursingtheglobalnursing100% (2)
- Cardiopatias Congenitas FINALDocument17 pagesCardiopatias Congenitas FINALA.V.M.No ratings yet
- Levine Theory ApplicationDocument38 pagesLevine Theory ApplicationSimon JosanNo ratings yet
- Manual of Clinical Microbiology 10th Edition MurrayDocument3 pagesManual of Clinical Microbiology 10th Edition MurrayMohsen Haleem15% (20)
- Broqueza, Jonnel Regoris: Philippine Children's Medical CenterDocument1 pageBroqueza, Jonnel Regoris: Philippine Children's Medical CenterRica RegorisNo ratings yet
- Errors 2Document5 pagesErrors 2Anggun rahmi PutriNo ratings yet
- 4D CT With Respiratory GatingDocument2 pages4D CT With Respiratory GatingLaura Karina Sanchez ColinNo ratings yet
- Position PaperDocument8 pagesPosition Paperapi-316749075No ratings yet
- Integrative Final DraftDocument16 pagesIntegrative Final Draftapi-532928007No ratings yet
- Are Patients Admitted To Emergency Departments With Regular Supraventricular Tachycardia (SVT) Treated AppropriatelyDocument3 pagesAre Patients Admitted To Emergency Departments With Regular Supraventricular Tachycardia (SVT) Treated AppropriatelyGading AuroraNo ratings yet
- Report PDFDocument2 pagesReport PDFAnonymous 6x3CyeNo ratings yet
- Receta Medica InglesDocument2 pagesReceta Medica InglesHannia RomeroNo ratings yet
- Perfusion Concept MapDocument1 pagePerfusion Concept Mapapi-639782898No ratings yet