Professional Documents
Culture Documents
Ineffective Airway Clearance
Uploaded by
Benly Grace Rebuyon MosquedaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ineffective Airway Clearance
Uploaded by
Benly Grace Rebuyon MosquedaCopyright:
Available Formats
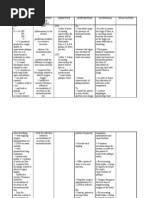
Diagnosis # 2
Need
Desired Outcome Within 8 hrs of nursing interventions:
Nursing Interventions
Rationale
Evaluation Statement
Ineffective Airway Clearance r/t retained secretions as manifested by dyspnea Subjective: dili ko ka ginhawa Objective: rales are evident upon auscultation dyspnea scale of 8 from scale of 0-10 V/S: BP = 140/90mmHg RR = 29 cpm CR = 52 bpm P= 56 bpm Background Knowledge The diastolic dysfunction (backward effects) of LFH results from the
P H Y S I O L O G I C
Patient will demonstrate improved ventilation airway patency Patient will expectorate secretions
Independent Evaluate change in level of mentation. Note cyanosis and change in skin color, including mucous membranes and nail beds Assess energy level and activity tolerance.
Accumulation of fluids/airway compromise can impair oxygenation of vital organs and tissues.
To determine choice of interventions and provides basis for comparison and evaluation of therapy. Reduces oxygen consumption/ demands and promotes maximal lung inflation
Goal partially met. Client verbalized, makaubo-ubo na ko pero gamay pa lang ang akoang mapagawas. Pero masulti nako na nag-improve jud siya.
Maintain chair/bedrest with head of bed elevated 20-30 degrees, semi-fowlers position. Support arms with pillows Encourage frequent position changes
Helps prevent atelectasis and
volume overload of the left ventricle or in some cases the left atrium. Because the left heart cannot discharge its normal ejection fraction, increased enddiastolic volume causes blood to accumulate in the left atrium, into the four pulmonary veins, and the pulmonary capillary bed (PCB). As the volume of blood in the lungs increases, the pulmonary vessels enlarge. The pressure of blood in the PCB increases. When it reaches a certain critical point (about 25-28 mm Hg), fluid passes across the pulmonary capillary membrane into the interstitial spaces around the alveoli and finally into the alveoli. Actual
pneumonia Instruct patient In effective deep breathing and coughing exercises Promotes optimal chest expansion and drainage of secretions thus, facilitates oxygen delivery Use of a scale to evaluate dyspnea helps clarify degree of difficulty and changes in condition.
Assess for dyspnea.
Specific Report patency in the airway
Auscultate breath sounds, noting crackles, wheezes
Promote bedrest/limit activity and assist with self-care activites
Goal partially met Patient report Reveals presence of that dyspnea pulmonary was reduced . congestion/collection of Patient secretions, indicating verbalized that need for further the phlegm is intervention. still present but has reduced in Reducing oxygen amount due to consumption/ demand his persistent during periods of coughingt has respiratory compromise may reduce severity of symptoms. To reduce irritant effect on airways.
Keep environment allergen/pollutant free
alveolar pulmonary edema occurs when the rate of fluid transudation exceeds the ability of the plentiful lymphatic drainage to remove it from the interstitial spaces. Acute pulmonary edema (APE) results as the alveoli fill with fluid; this impairs gas exchange. Impaired gas exchange refers to excess or deficit in oxygenation and/or carbon dioxide elimination at the alveoli-capillary membrane (this may be an entity of its own but also may be an end result of other pathology with interrelatedness between airway clearance and/or breathing pattern problems.
Collaborative Administer supplemental oxygen as indicated Increases alveolar oxygen concentration, which may correct/ reduce tissue hypoxemia Reduces alveolar congestion, enhancing gas exchange. Increases oxygen delivery by dilating small airways and exerts mild diuretic effect to aid in reducing pulmonary congestion.
Administer medication as indicated: Diuretics, e.g., furosemide
Maintain adequate I&O but avoid fluid overload Encourage adequate rest and limit activities within client tolerance. Promote calm, restful environment.
For mobilization of secretions Helps limit oxygen needs/consumption.
Patient will Verbalize and demonstrate understanding of methods in
Goal met
maintaining patency of the airway
Demonstrate deep breathing exercises
Creates resistance against outflowing air to prevent collapse/narrowing of airways, thereby helping distribute air throughout the lungs and relieve/reduce shortness of breath.
Patient able to verbalize eagerness to participate in the treatment regimen as well as the methods in improving his airway.
Provide psychological support, listening to questions/ concerns. Review oxygenconserving techniques (e.g. sitting instead of standing to perform tasks, eating small meals:performing slower purposeful movements. Reinforce treatment rationale. Include significant others in teaching as appropriate.
This will aid in decreasing of anxiety and increase patients self-esteem. Knowledge of disease process and expectations can facilitate adherence to prescribed treatment regimen.
Patient will participate in treatment regimen
Patient may believe it is acceptable to alter postdischarge regimen when feeling well and symptom-free or when feeling below par,
Review safe use of medications, purpose and side effects requiring medical evaluation. Provide oral and written instructions.
which can increase the risk of exacerbation of symptoms. Understanding of regimen, medications and restrictions may augment cooperation Goal met with control of patient able to symptoms. understand Understanding of the purpose of therapeutic needs and the drugs importance of prompt given to him reporting of side effects and was can prevent occurrence encouraged to of drug-related take them as complications. Anxiety prescribed may block comprehension of input or details and patient/significant others may refer to written material at alter date to refresh memory.
You might also like
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananNo ratings yet
- Acute GastroenteritisDocument2 pagesAcute GastroenteritisErika CadawanNo ratings yet
- NCP BMDocument1 pageNCP BMSourabh MehraNo ratings yet
- ANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationDocument2 pagesANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationEdrianne Tui100% (2)
- Medication ThalassemiaDocument3 pagesMedication ThalassemiaDivya ToppoNo ratings yet
- Pleural EffusionDocument5 pagesPleural EffusionTerizla MobileNo ratings yet
- Nursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NDocument2 pagesNursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NnananaNo ratings yet
- AAAAA Altered-Body-Temp-NCPDocument2 pagesAAAAA Altered-Body-Temp-NCPMoi ValdozNo ratings yet
- Nursing Care Plan for Managing HyperthermiaDocument4 pagesNursing Care Plan for Managing Hyperthermiamimingdot33No ratings yet
- Risk For Ineffective Airway Clearance 1Document8 pagesRisk For Ineffective Airway Clearance 1kint manlangitNo ratings yet
- Gastrectomy NCP IBPDocument3 pagesGastrectomy NCP IBPKevin T. Katada100% (1)
- Nursing Care Plan for a Patient with Multiple Bruises and Difficulty BreathingDocument3 pagesNursing Care Plan for a Patient with Multiple Bruises and Difficulty BreathingLeogalvez BedanoNo ratings yet
- Ineffective Airway Clearance Nursing Care PlanDocument2 pagesIneffective Airway Clearance Nursing Care Planrois romaNo ratings yet
- Deficient Fluid Volume (Vanene)Document7 pagesDeficient Fluid Volume (Vanene)jajalerNo ratings yet
- NCP PSHDocument17 pagesNCP PSHMargareth OrtizNo ratings yet
- Ineffective Airway Clearance - PTBDocument2 pagesIneffective Airway Clearance - PTBIrish Eunice FelixNo ratings yet
- Assessing and Managing Ineffective Airway ClearanceDocument3 pagesAssessing and Managing Ineffective Airway ClearanceNelle Agni100% (1)
- Assessment Subjective: "Nahihirapan Ako Huminga" As VerbalizedDocument2 pagesAssessment Subjective: "Nahihirapan Ako Huminga" As Verbalizedmayla_jordan3666No ratings yet
- Fluid Volume Deficit BatuDocument2 pagesFluid Volume Deficit Batumecz26No ratings yet
- Nursing Care Plan: Cystic FibrosisDocument4 pagesNursing Care Plan: Cystic FibrosisYael EzraNo ratings yet
- Multiodular non toxic goiter nursing care planDocument1 pageMultiodular non toxic goiter nursing care plankzbreakerrNo ratings yet
- Nursing Care Plan For Ineffective Airway ClearanceDocument6 pagesNursing Care Plan For Ineffective Airway ClearanceCaroline ChaNo ratings yet
- Assessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesAssessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDanica Kate GalleonNo ratings yet
- NCP PTBDocument6 pagesNCP PTBJay Dela VegaNo ratings yet
- NCP For CTTDocument1 pageNCP For CTTJen Rhae LimNo ratings yet
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee BaluyotNo ratings yet
- Ineffective Breathing PatternDocument7 pagesIneffective Breathing PatternJanmae JivNo ratings yet
- NCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsDocument3 pagesNCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsSarah Ann Jamilla FaciolanNo ratings yet
- Nursing ManagementDocument16 pagesNursing ManagementNica Marie LumbaNo ratings yet
- 6 Pleural Effusion Nursing Care PlansDocument7 pages6 Pleural Effusion Nursing Care PlansShaina Fe RabaneraNo ratings yet
- NCP For Ineffective Airway ClearanceDocument3 pagesNCP For Ineffective Airway ClearanceJennelyn BayleNo ratings yet
- Seizure NCPDocument2 pagesSeizure NCPChristine Dela CruzNo ratings yet
- Assessing Nursing Diagnoses and Expected OutcomesDocument20 pagesAssessing Nursing Diagnoses and Expected OutcomesZamranosNo ratings yet
- Ineffective Breathing Pattern As Evidenced by Use of Accessory Muscles and Episodes of DyspneaDocument3 pagesIneffective Breathing Pattern As Evidenced by Use of Accessory Muscles and Episodes of DyspneaNiel MinatozakiNo ratings yet
- Risk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.Document2 pagesRisk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.eleinsamNo ratings yet
- Monitor and regulate body temperature for patient with hyperthermiaDocument2 pagesMonitor and regulate body temperature for patient with hyperthermiaDudong SasakiNo ratings yet
- Assessing and Treating Pneumonia Through Respiratory Monitoring and InterventionsDocument3 pagesAssessing and Treating Pneumonia Through Respiratory Monitoring and InterventionsDyanne BautistaNo ratings yet
- Assessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationDocument6 pagesAssessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationimnasNo ratings yet
- NCP - Acute Pain Related To EdemaDocument2 pagesNCP - Acute Pain Related To EdemaChenime Añana0% (1)
- PHASE 2 NCP (Injury, Risk For Bleeding)Document3 pagesPHASE 2 NCP (Injury, Risk For Bleeding)NE TdrNo ratings yet
- NCP HemothoraxDocument3 pagesNCP HemothoraxMichael John F. NatividadNo ratings yet
- NCP Acitivity IntoleranceDocument3 pagesNCP Acitivity IntolerancegizelleNo ratings yet
- Risk for Aspiration Nursing Care Plan During CholecystectomyDocument1 pageRisk for Aspiration Nursing Care Plan During CholecystectomyJess GoNo ratings yet
- Case Study Pleural EffusionDocument4 pagesCase Study Pleural EffusionKhristine Anne FabayNo ratings yet
- NCP Lack of KnowledgeDocument3 pagesNCP Lack of KnowledgeFaye BartianaNo ratings yet
- Drug StudyDocument4 pagesDrug StudyPam RomeroNo ratings yet
- NCP HyperthermiaDocument2 pagesNCP HyperthermiaMeljonesDaanNo ratings yet
- Diarrhea NCPDocument3 pagesDiarrhea NCPCharles Michael AzagraNo ratings yet
- Actual NCPDocument2 pagesActual NCPbaki0146No ratings yet
- NCP - ERDocument5 pagesNCP - ERAnnelore ArcayNo ratings yet
- NCP PTBDocument2 pagesNCP PTBMack Jhed AnarconNo ratings yet
- NCP CopdDocument4 pagesNCP CopdJoshua ValdrizNo ratings yet
- BPN NCPDocument6 pagesBPN NCPJoart EspinozaNo ratings yet
- Rufino, Leslie Kriztel S. BSN 3-2 Group 1Document6 pagesRufino, Leslie Kriztel S. BSN 3-2 Group 1Deinielle Magdangal RomeroNo ratings yet
- Impaired Gas ExchangeDocument4 pagesImpaired Gas ExchangeNuraini Hamzah100% (1)
- Managing COPD: Nursing Care for Breathing Issues, Nutrition, Infection RiskDocument2 pagesManaging COPD: Nursing Care for Breathing Issues, Nutrition, Infection RiskAl RizkyNo ratings yet
- Respiratory FailureDocument15 pagesRespiratory FailureKennedy Ng'andweNo ratings yet
- Pleural Effusion NCPsDocument7 pagesPleural Effusion NCPsJaja Nagallo100% (2)
- Nursing Care PlanDocument10 pagesNursing Care PlanElijah S GomezNo ratings yet
- Impaired Gas ExchangeDocument2 pagesImpaired Gas ExchangeHanya Bint PotawanNo ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway ClearanceBenly Grace Rebuyon MosquedaNo ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway ClearanceBenly Grace Rebuyon MosquedaNo ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway ClearanceBenly Grace Rebuyon MosquedaNo ratings yet
- Drug Study FinalDocument22 pagesDrug Study FinalBenly Grace Rebuyon MosquedaNo ratings yet
- Ferrous Sulfate Iron SupplementDocument3 pagesFerrous Sulfate Iron SupplementBenly Grace Rebuyon MosquedaNo ratings yet
- One China PolicyDocument1 pageOne China PolicyBenly Grace Rebuyon MosquedaNo ratings yet
- Viii NCPDocument6 pagesViii NCPAdrian MangahasNo ratings yet
- Kesesuaian StokDocument2 pagesKesesuaian StokResky OktavianiNo ratings yet
- Alywn Cosgrove Real World Fat Loss PDFDocument75 pagesAlywn Cosgrove Real World Fat Loss PDFJM Gym Manticao100% (1)
- Interpreting PDX Dot BlotsDocument2 pagesInterpreting PDX Dot BlotsSpy CameraNo ratings yet
- Slums: The History of A Global Injustice, by Alan MayneDocument4 pagesSlums: The History of A Global Injustice, by Alan MayneKarliane MassariNo ratings yet
- Comm 602 Assignment 1Document4 pagesComm 602 Assignment 1hamiltjw2No ratings yet
- Installation and Preoperative TestDocument27 pagesInstallation and Preoperative TestLeonardo BaiaoNo ratings yet
- IAT 1 Answer Key RHEDocument13 pagesIAT 1 Answer Key RHEAparna GanesenNo ratings yet
- Interpretation: L23 - FPSC Malviya Nagar1 A-88 Shivanand Marg, Malviyanagar JaipurDocument4 pagesInterpretation: L23 - FPSC Malviya Nagar1 A-88 Shivanand Marg, Malviyanagar Jaipurmahima goyalNo ratings yet
- Cultural Differences in Travel Risk PerceptionDocument20 pagesCultural Differences in Travel Risk PerceptionEsther Charlotte Williams100% (2)
- Hyperglycemic Hyperosmolar State - A Diabetic EmergencyDocument2 pagesHyperglycemic Hyperosmolar State - A Diabetic EmergencyNiken AninditaNo ratings yet
- Massive Transfusion ProtocolDocument5 pagesMassive Transfusion ProtocolArlette Araceli Barbosa IbarraNo ratings yet
- Physical characteristics and vocal qualities of major neurological movement disordersDocument1 pagePhysical characteristics and vocal qualities of major neurological movement disordersShruti KumarNo ratings yet
- SPECIAL WORKSHOP ANNOUNCEMENT-with Keshe NotesDocument4 pagesSPECIAL WORKSHOP ANNOUNCEMENT-with Keshe NotesAhmad AriesandyNo ratings yet
- Anatomy Trains 3rd Edition Emag 1Document62 pagesAnatomy Trains 3rd Edition Emag 1Dibyendu BanerjeeNo ratings yet
- Truvivity by NutriliteDocument10 pagesTruvivity by Nutriliteโยอันนา ยุนอา แคทเธอรีน เอี่ยมสุวรรณNo ratings yet
- Minitek Indore Profile 2Document9 pagesMinitek Indore Profile 2kunal agiwaleNo ratings yet
- Improving Workplace Safety Behavioral Based Safety: ThroughDocument32 pagesImproving Workplace Safety Behavioral Based Safety: ThroughYursNo ratings yet
- Individual Development FactorsDocument9 pagesIndividual Development Factorshanani_leeNo ratings yet
- Interpretation of Abnormal CTG Pattern - 2Document17 pagesInterpretation of Abnormal CTG Pattern - 2Jaspreet Kaur100% (1)
- BICOM Treatment of Chronic Fatigue and FibromyalgiaCFS ReportDocument15 pagesBICOM Treatment of Chronic Fatigue and FibromyalgiaCFS ReportAnahata Fraydon100% (1)
- Ward D - Freida McFaddenDocument239 pagesWard D - Freida McFaddenHassan ZayanNo ratings yet
- Nursing responsibilities for tramadol administrationDocument2 pagesNursing responsibilities for tramadol administrationThrinNo ratings yet
- NEWCROSS Site Survey - Rev1Document37 pagesNEWCROSS Site Survey - Rev1eke23No ratings yet
- Tai Chi Qigong TrainerDocument11 pagesTai Chi Qigong Trainerskycall28No ratings yet
- Career Path PDFFFFDocument2 pagesCareer Path PDFFFFapi-410567922No ratings yet
- Liver Disease: Overview of The LiverDocument6 pagesLiver Disease: Overview of The LiverMustafa AlmasoudiNo ratings yet
- Timetable Theory-August 2023Document22 pagesTimetable Theory-August 2023SueNo ratings yet
- Bowen Therapy Melbourne - Natural ApproachDocument17 pagesBowen Therapy Melbourne - Natural Approachnatural Approach100% (2)
- Providing Public Area ServicesDocument48 pagesProviding Public Area ServicesFONCY BUYANNo ratings yet