Professional Documents
Culture Documents
Choosing Between Cobalt-60 and Linear Accelerator Units
Uploaded by
Santanu SamantaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Choosing Between Cobalt-60 and Linear Accelerator Units
Uploaded by
Santanu SamantaCopyright:
Available Formats
50 Years of Cancer Control in India
CHOICE OF A TELETHERAPY UNIT: COBALT 60 UNIT vs LINEAR ACCELERATOR
K. S. Reddy
Cancer has been present throughout human history. Egyptian and Incan mummies show evidence of the disease. Accurate information regarding the disease and different modalities of treatment have been developed only during the last century. In the later half of twentieth century, it was well recognized that cancer has been the leading cause of death and it affects approximately one in two men and one in three women during their life times. In fact, the global cancer incidence is predicted to double between now and the year 2020 at which time there will be over 200,00,000 new cases diagnosed each year. Majority of these will be in the developing countries. Of these, 12,000,000 deaths will result. WHO estimates that if these trends continue, cancer will be the leading cause of death everywhere except in sub Saharan Africa and most victims will be in the 50-60 year age group. Treatment strategies for cancers have evolved mainly during the last 50 years. Radiotherapy is one of the major modalities of cancer treatment and every alternate cancer patient will require radiation during the course of treatment. It is also well recognized that over 40% of the course of cancer result directly from the use of radiotherapy. By 2020, 70% of the global need for radiotherapy will be in the currently defined developing world.
History
First application of x-rays for therapeutic purpose was made on Jan.29, 1896 in Chigago by Grubbe for treatment of breast carcinoma. The first case of cure of malignant tumour by radiotherapy alone was reported on a patient with a histologically confirmed squamous cell carcinoma of the nose. In 1899 she received 150 radiations over 9 months, was cured and was alive and well 30 years later. Curative results for some head and neck cancers were reported from Curie
79
79
50 Years of Cancer Control in India Institute in Paris (Coutard 1932). In mid 1930s, radiotherapy was beginning to be used as an adjuvant to radical mastectomy.
Cobalt 60 Unit:
In 1951, Cobalt 60 teletherapy was first put to clinical use in London, Ontario. It was adopted with tremendous enthusiasm in the treatment of malignant disease. A typical teletherapy 60 CO source is a cylinder of diameter 2 cm., height 5 cm., and is positioned in the Cobalt Unit with the circular end facing the patient. The fact that the radiation source is not a point source complicates the beam geometry and gives rise to what is known as the geometric penumbra and the transmission penumbra. These penumbras create a region of dose variation at the field edges. Cobalt-60 Gamma radiation typically has energy of about 1.2 MV, D-max being 0.5 cm. and a percentage depth of 55% at 10 cm. Cobalt units with low energy of gamma rays are ideal for treatment of head and neck cancers. This would cover 25% of cancers seen in a large cancer treatment center. Majority of others will be cervical cancers and others like cancers of oesophagus, lung, prostate, etc. where the separation or thickness of parts to be treated will be greater that 20 cm. Even though Cobalt units can be used for above clinical situations they do not give the ideal depth dose and require complicated plans to deliver the effective tumor dose. Dr. Herman Suit of Harvard Medical School wrote in an editorial that Cobalt units should be modernized with state of the art ancillary devices and then they could be fully acceptable for the treatment of head and neck cancers, cancer of breast and some soft tissue sarcomas of extremities. However Cobalt-60 units over the last several decades have remained static in design and there has been very little change in ancillaries and accessories. The major problem with these units is the decaying source, reduced output resulting in increased treatment times which in turn will effectively reduce the patient output. The source needs to be replaced every 5-7 years and is becoming more and more expensive and is also hard to get. Disposal of spent source is another major problem and this will be compounded if as per estimates our country should have at least 1000 teletherapy units, (1 unit per million if not 2 per million population) 80
50 Years of Cancer Control in India we will need at least 200 sources to be replaced every year and a similar number to be sent for waste disposal.
Linear accelerator:
In the first few decades after discovery of x-rays only low energy xrays were available and they were used predominantly for palliative treatment. From the technology of World War II radars came the ability to produce high energy microwaves. This field advanced with the development of high energy microwave tubes known as Klystronsor Magnetrons which are still at the heart of todays' modern Linear Accelerators. The First medical Linear Accelerator was created and used in England in 1953 followed by USA (at Standford University (Gintzon 1984)5. Basically the Linear accelerator (Linac) is a device that uses high frequency electromagnetic waves to accelerate charged particles such as electrons to high energies through a Linear tube. The high energy electron itself can be used for treating superficial tumors or it can be made to strike a target to produce x-rays for treating deep seated tumours. Linear accelerators have made rapid progress in technology, design, ancillaries and utility. In the '60s & '70s Cobalt Unit have largely been replaced by Linear Accelerators in most of the radiation oncology departments in the developed countries. Low, medium and high energy Linacs are now available which can generate not only x-rays but also electrons for treatment. Newer technologies like multi leaf collimators (MLC) fittedto Linac, intensity modulated Radiotherapy Plans (IMRT) have helped to improve accuracy in executing treatment. While the high energy Linacs (with x-ray and variably energy electron generating potential) are expensive, Low energy Linacs (4-6 MV) compare favourably with traditional cobalt units in terms of cost as well as uptime. The characteristics of the Linac beam and out put are superior to Cobalt-60 gamma ray beam.
Comparison
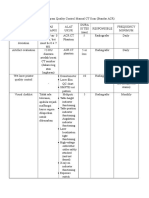
Several arguments have been put forward both for and against Cobalt Units as well as Linear accelerators. These arguments relate to physics, clinical advantages and more importantly, the cost consideration. The following table summarises the data that is available. 81 81
50 Years of Cancer Control in India
Feature Dose rate Low Energy 600 MU/Min Cobalt Accelerator Reducing dose starts at 200r/min Remarks 60Unit In Cobalt units dose will reduce because of decay, and depends on source activity. whereas with Linear Accelerator one has the guarantee of constant dose rate Penumbra effect is higher in cobalt machines Source cost for 12,000 curie source is very much on the increasing trend. Current cost for 12,000 curie source is around Rs. 35, 00,000. since the higher curie sources are not available with BARC one has to import the source along with the machine and at the time of change of source one has to send the decayed source back to the manufacturer, which is very expensive. Linear accelerator with 6 MV, photon, we are able to get D-max 1.5 cm. This is very useful for deep seated tumours. Skin sparting is better with Linac (6 mv). Difficult to treat deep seated tumors in Thorax, abdomen or pelvis. In cobalt one cannot treat field size less than 5x5cm.
Energy Source DIA Source change
<2mm None
20mm Every 7 years 30-35 lakhs
D- max
1.5 cm
Only 0.5cm
Perchantage 67% Depth dose at 10cm Colimator trasmission Minimum field size Radiation leakage through the head Penumbra Not exceed o.5% 0.5x0.5 cm Nil
55%
More than 3% 5 x 5 cm Less than 0.2%
Less than 5 mm
More than 1 cm
With 2 cm. Cobalt source the Penumbra effect is very high.
82
50 Years of Cancer Control in India
Feature Precision Low Energy Dose delivered to any arc is reproducible within 3% or 1MU which ever is greater Possible Cobalt Accelerator Remarks 60Unit In Linear accelerator one c an have reproducibility of Dosimetry system and the dose delivered is continuously monitored and recorded
Motorized wedges Variable dose rate
Not possible
80 to 600 MU/min
Not variable
Dose rate if fixed, decreases with decay of source Increases accuracy in dose delivery
Multileaf Possible collimators, stereotactic attachments Asymmetric collimator jaws Yes, standard features
Not possible
No
Electronics are cheaper Independenty collimator jaws are very useful for precise and accurate cancer treatment The costly maintenance is compensated as source cost is not required for Linacs Allows to view actual tumour while treatment Provides wider application usage
Parts Parts costlier replacement Portal vision Yes, possible attachment (Optinal) Steroetatic Yes, can be applications used with additional tools Civil Marginally requirement costly for the compared to installatin of cobalt unit telepherapy Unit Patient support system Superior
No
No
Inferior, low accuracy
83
83
50 Years of Cancer Control in India
Feature Low Energy Cobalt Accelerator Not possible Remarks 60Unit Beam matching is a very good feature available in Linear accelerator. This will help institutions to buy the 2nd machine with the same beam characteristics of the existing units. Thereby patients can be shifted between different Linear accelerator. More flexibility. WHO recommends built in guarantee/performance clauses for 5-10 years after procurement BAARC does not permit disposal for imported source. In the event the source is imported along with the cobalt machine the decayed source has to be transported back to the manufacturers, which is very expensive. Rs. 1.90 crores (cost of cobalt source) Since the number of Cobalt units sold worldwide is on a decreasing trend during the last 10 years, the cost of cobalt units is increasing due to high manufacturing cost with less number of units being sold every year.(not mre than 50 units worldwide per year). Whereas Linear accelerators are sold at least 500 units per year worldwide. 1 lakh/year In ten year span accelerators are slightly expensive.
Beam Possible matching with second unit
Uptime
95%
95%
Source disposal
Nil
Major problem with cobalt units, and source cost is increasing every year. It is also becoming increasingly difficult to obtain a source Rs. 2.5-3 crores
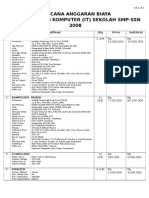
Cost of the machine
AMC with labour Spare parts cost for 10 years operation INR20,00,000
2 lakhs/year
INR 10,00,000
84
50 Years of Cancer Control in India
Feature Low Energy Cobalt Accelerator INR 35,00,000 Remarks 60Unit The source to be replaced at least once every sever years In ten years period we need to spend more money towards maintenance and source replacement. The running cost of linear accelerator over 10 years is less when compared to a cobalt unit. Also Linear accelerator has definite clinical advantages over Cobalt.
Source Nil replacement cost Running AMC charges cost of the .for 10 years machine for = Rs. 20 lakhs, 10 years cost of spare including parts for 10 yrs labour, spare = Rs. 20 lakhs, parts and total maintecobalt source nance cost of low energy accelerator = 40 lakhs.
AMC charges for 10 years = Rs. 10 lakhs. Cost of spare parts for 10 yrs = Rs. 10 lakhs. Cost of source replacement = Rs. 35 lakhs. Total maintenance cost for Cobaltmachine = 55 lakhs.
At the present time the treatment machine to population ratio ranges from 12 machines per million in US to fewer than 0.3 machines per million in china. In India we have around 290 telepherapy machines spread over 62 cities/towns for a billion population. Around 35 of them are Linear Accelerators and the rest are Cobalt Units. Currently around 30 countries have no access to radiotherapy at all. In 1993 the cancer division of WHO conducted it's first consultation on Radiotherapy and repeated it's consultation to refine the recommendations concerning radiotherapy at London in March 1999. This meeting summarized a statement regarding the results of the second consultation in the UICC News Archives.6 The assumptions were that radiotherapy remained an important and cost effective modality in treatment of cancer. The WHO supported the growth of programmers in which the sales of megavoltage equipment, planning systems and simulators is linked to training, education staffing and the use of treatment protocols. They further recommended that service contracts together with peformance guarantees be built into the programmes and these contracts should run from 5 to 10 years. They also considered the question of cobalt 85 85
50 Years of Cancer Control in India 60 vs. Linear Accelerator and considered the need for Linac technology in the developing world. The group recognized that linac technology is associated with advantages over cobalt teletherapy, especially as regard collimation, conformal therapy and the ability to perform intensity modulation. The working group concluded that if capital costs and service were essentially equal, then linac technology would be considered superior to cobalt technology for modern day curative radiotherapy. Contrary to the popular belief that radiotherapy is expensive, it is salient to note that the cost of one military jet fighter represents the entire costs for radiation therapy for most countries. In fact, together with surgery, radiotherapy currently remains the most cost-effective way of curing cancer.
Conculsion:
Cobalt 60 units provide relatively high energy gamma rays for radiotherapy which are ideally suited for treatment of head and neck cancers and other superficially located tumours like breast cancers and soft tissue sarcomas of extremities. They are not adequate for treatment of deep seated tumours and have the added disadvantage of decreasing output with decay of source and the need for source replacement within 5-7 years. Disposal of decayed source is another major concern. The beam characteristics when compared to 6mv Linacs are inferior and fewer ancillaries are available for cobalt machines as compared to Linacs. High energy Linacs in addition to giving two or three x-ray energies can also generate variable energy electron beam for treatment. While such high energy Linacs are expense, 6 MV Linacs compare favourably in terms of cost with the Cobalt 60 units. Even though the initial cost appears to be high, over a ten year period maintenance costs are less as it does not require change of source. It is stressed that service contracts with performance guarantees for 5-10 years have to be built into the contracts while procuring the equipment. To summarize Linear accelerators have several advantages: 1. Very high energy beams can be created with a machine that is not very bulky or cumbersome to use. 86
50 Years of Cancer Control in India 2. The edges of the beams are much more sharply defined than those of a cobalt machine, allowing additional precision in dose delivery. 3. Electron beams can be created (with high energy linacs) that is of particular value in treating superficial lesions. 4. The dose rate per minute is variable and can be turned up very high allowing the patient to be located at substantial distance from the machine in order to create large fields necessary for total skin or total body irradiation while still maintaining adequate dose rate. With cobalt, the rate is determined by the amount of cobalt source in the machine and cannot be regulated. References: 1. Del Regato JA. Gosta Forsell, Int. J. Radiation Oncol Bioi Physics, 1977; 2: 783-70 2. Coutard H Roentgen Therapy of epitheliomas of tosillar region, hypopharynx and larynx from 1920 to 1926. Am J Roentgenology, 1932;3228: 313-31 3. Van DykJ, Battista, J.J. Cobalt-60: an old modality, a renewed challenge, Current Oncology, 1996; 3: 8k-17. 4. Suit H. What is the optimum choicL (Editorial). Int, J. Radiation Oncol Bil Physics, 1986; 12: 1711-1712. 5. GintzonEL, Nunan Cs. Historyof Microwave elector Linear accelerators for Radiotherapy. Int. J Radiation Oncol Biol Phys, 1984; 11:205-216. 6. Aref A, Chodounsky Z, Elzawawy a, Manatrakul N, Ngoma T, Orton C, Porter At, Sikora K, Eric Van't Hooft. Summary Statement of the WHO Second Radiotherapy Consultation March 5-6, 1000, London, UK, UICC News archieves, April-June 1999. 7. Lichter AL, Lampe I. Radiation therapy. In abeloff MD Ed: Clinical Oncology, Ba
87
87
You might also like
- Cobalt-60 and Linacs - Competing TechnologiesDocument6 pagesCobalt-60 and Linacs - Competing TechnologiesTomás Alexander Alvis MenachoNo ratings yet
- Healingenvironments RadiotherapyDocument99 pagesHealingenvironments Radiotherapyden yogaNo ratings yet
- Bhabhatron: An Indigenous Telecobalt Machine For Cancer TreatmentDocument8 pagesBhabhatron: An Indigenous Telecobalt Machine For Cancer TreatmentK. JayarajanNo ratings yet
- Improving Selection to the Foundation Programme: An Overview of New Selection MethodsDocument29 pagesImproving Selection to the Foundation Programme: An Overview of New Selection MethodsStanley LiewNo ratings yet
- Halcyon Brochure RAD10443B 092417Document14 pagesHalcyon Brochure RAD10443B 092417Anonymous 0TOLgQWuHvNo ratings yet
- AxisTV v.8.0 Technical ManualDocument110 pagesAxisTV v.8.0 Technical ManualDrew Allen Dennis50% (2)
- Rab Alat Medis Dan Penunjang Medis Kea Medistra 2020Document17 pagesRab Alat Medis Dan Penunjang Medis Kea Medistra 2020Sultan CikupaNo ratings yet
- All Set RSUD - TarakanDocument14 pagesAll Set RSUD - TarakanAnggi SitompulNo ratings yet
- Current Status of Radiotherapy in FARO CountryDocument24 pagesCurrent Status of Radiotherapy in FARO CountrySamuel Kelvin RuslimNo ratings yet
- Ezdocs Document Management System Product BrochureDocument6 pagesEzdocs Document Management System Product BrochureZameer AhmedNo ratings yet
- RAB Internet AllDocument2 pagesRAB Internet Allzay_cobainNo ratings yet
- Varian Medical Systems JPM PresentationDocument34 pagesVarian Medical Systems JPM PresentationmedtechyNo ratings yet
- History of Radiotherapy & Infrastructure in IndiaDocument106 pagesHistory of Radiotherapy & Infrastructure in IndiaRakesh JadhavNo ratings yet
- Katalog HVAC Polytron 2017 LocalDocument28 pagesKatalog HVAC Polytron 2017 LocalYoga PramudyaNo ratings yet
- CT Scan 64 SliceDocument4 pagesCT Scan 64 SliceMeTha PoEnyaNo ratings yet
- Radlink PET and Cardiac Imaging Centre - PhilipsDocument1 pageRadlink PET and Cardiac Imaging Centre - PhilipsRadlinkSingaporeNo ratings yet
- Rab CCTV (PT)Document2 pagesRab CCTV (PT)Haf izhNo ratings yet
- Lab Equipment Inventory 2015-2019Document5 pagesLab Equipment Inventory 2015-2019RusmindartiNo ratings yet
- Hospital Expenditure Report by DoctorDocument32 pagesHospital Expenditure Report by Doctorgalih wicaksonoNo ratings yet
- Sale Sheet Mistral 1007140 Print File ROWDocument2 pagesSale Sheet Mistral 1007140 Print File ROWravisagarNo ratings yet
- Tabel QC CT ScanDocument6 pagesTabel QC CT ScanbayuNo ratings yet
- Simulasi Koding&Tarif Bedah Umum Rs Type D (Inacbg)Document1 pageSimulasi Koding&Tarif Bedah Umum Rs Type D (Inacbg)Achmad Dzulfikar AziziNo ratings yet
- Paramount Bed Indonesia E-Catalogue Price ListDocument3 pagesParamount Bed Indonesia E-Catalogue Price Listginayulistiana50% (2)
- Quick CountDocument36 pagesQuick CountSLAMET PAMUJINo ratings yet
- Design OperasiDocument4 pagesDesign OperasitedyNo ratings yet
- RAB VMS Variable Message SignDocument4 pagesRAB VMS Variable Message Signdede yulmarinoNo ratings yet
- Jurnal CT ScanDocument9 pagesJurnal CT ScanPungki Putra TamaraNo ratings yet
- Tata Cara Menyusun Study Kelayakan Pendirian Rumah SakitDocument75 pagesTata Cara Menyusun Study Kelayakan Pendirian Rumah SakitisnugraikaNo ratings yet
- FORM QC MRI AcceptTesting 0604Document4 pagesFORM QC MRI AcceptTesting 0604Yuda FhunkshyangNo ratings yet
- Perhitungan Beban Kerja IPS MedisDocument55 pagesPerhitungan Beban Kerja IPS Medisainul istiadzahNo ratings yet
- Techno FixDocument36 pagesTechno Fixbinta100% (1)
- MMWP 2008C DatasheetDocument12 pagesMMWP 2008C DatasheetSergeyKuznetsovNo ratings yet
- E-Cube Line Up CatalogDocument16 pagesE-Cube Line Up CatalogJose QuiscaNo ratings yet
- Daftar Harga Instrumente Zepf PDFDocument193 pagesDaftar Harga Instrumente Zepf PDFAnonymous GF9qEM2EnjNo ratings yet
- Makalah Bahasa InggrisDocument8 pagesMakalah Bahasa InggrisNorhikmahNo ratings yet
- Katalog - Lenovo JakartaDocument20 pagesKatalog - Lenovo JakartaFahmiNo ratings yet
- Spesifikasi CT Scan Somatom Perspective 128 SliceDocument2 pagesSpesifikasi CT Scan Somatom Perspective 128 SliceVro JackNo ratings yet
- Form Ceklist Harian Alat RadiologiDocument3 pagesForm Ceklist Harian Alat Radiologilenggo geniNo ratings yet
- An Experiment With Arduino Uno and TFT Nextion For Internet of ThingsDocument6 pagesAn Experiment With Arduino Uno and TFT Nextion For Internet of Thingsaeri sujatmikoNo ratings yet
- EMResource - NEDOCS Definitions and Tracking LogDocument2 pagesEMResource - NEDOCS Definitions and Tracking LogkingdonNo ratings yet
- Ai Pengujian Lead ApronDocument8 pagesAi Pengujian Lead Apronwildan sanjayaNo ratings yet
- Daftar Alat-Alat Yang Ada Diruangan Instalasi Gawat Darurat RS Bina Kasih Pekanbaru Lemari High AlertDocument5 pagesDaftar Alat-Alat Yang Ada Diruangan Instalasi Gawat Darurat RS Bina Kasih Pekanbaru Lemari High AlertRiwiyoko YrsNo ratings yet
- AAPM 34 - MRI Acceptance TestDocument16 pagesAAPM 34 - MRI Acceptance TestmahbodsedNo ratings yet
- Excimer Laser Basics: Original Author: Professor Theo Seiler Universitätsaugenklinik Dresden Dresden, GermanyDocument28 pagesExcimer Laser Basics: Original Author: Professor Theo Seiler Universitätsaugenklinik Dresden Dresden, GermanynafsikavNo ratings yet
- BQ STP 5 KubikDocument2 pagesBQ STP 5 Kubikbim akadeNo ratings yet
- Jarit CV Catalog NS1888 04 08 PDFDocument285 pagesJarit CV Catalog NS1888 04 08 PDFFabian Andres GiraldoNo ratings yet
- Dual Source CT Imaging PDFDocument275 pagesDual Source CT Imaging PDFAnisa SetiawatiNo ratings yet
- Umj 1x Adilsiswan 854 1 Jurnala LDocument18 pagesUmj 1x Adilsiswan 854 1 Jurnala LRudi AndikaNo ratings yet
- Rab Alkes Dak Rsud Muaradua 2023Document4 pagesRab Alkes Dak Rsud Muaradua 2023Kontol LodonNo ratings yet
- Rab Lab ComDocument2 pagesRab Lab ComMusliminIminNo ratings yet
- Terumo E-Catalog Prices June 2017Document4 pagesTerumo E-Catalog Prices June 2017rahayuNo ratings yet
- Handbook of Sutures and KnotsDocument50 pagesHandbook of Sutures and KnotsOgunfowora Olumide TaiwoNo ratings yet
- Rev5 RAB CCTV GMB1Document1 pageRev5 RAB CCTV GMB1CV. PEMUDA MERDEKANo ratings yet
- Agfa CR 10 XDocument4 pagesAgfa CR 10 XSandyKarittokNo ratings yet
- Choice of A Teletherapy Unit: Cobalt 60 Unit Vs Linear AcceleratorDocument9 pagesChoice of A Teletherapy Unit: Cobalt 60 Unit Vs Linear AcceleratorMd. Ashikur RahmanNo ratings yet
- BARC Develops Cobalt-60 Teletherapy Machine For Cancer TreatmentDocument6 pagesBARC Develops Cobalt-60 Teletherapy Machine For Cancer TreatmentK. JayarajanNo ratings yet
- Orthovoltage Vs MegavoltageDocument7 pagesOrthovoltage Vs MegavoltageEmmanuel Cuevas MisNo ratings yet
- (RADIO 250) LEC 10 Radiation OncologyDocument3 pages(RADIO 250) LEC 10 Radiation OncologyWilliam PinzonNo ratings yet
- X-Ray-Sterilization SystemDocument12 pagesX-Ray-Sterilization Systemamin adimiNo ratings yet
- Rectangular Collimation: No Longer A Matter of Choice!Document10 pagesRectangular Collimation: No Longer A Matter of Choice!comphomeNo ratings yet
- CA CX Biological MarkersDocument38 pagesCA CX Biological MarkersSantanu SamantaNo ratings yet
- JCO 2012 Lee 268 73Document6 pagesJCO 2012 Lee 268 73Santanu SamantaNo ratings yet
- NHL CaseDocument29 pagesNHL CaseSantanu SamantaNo ratings yet
- 08 Pneumonia Review ofDocument4 pages08 Pneumonia Review ofMonika Margareta Maria ElviraNo ratings yet
- Counseling Notification 2013Document5 pagesCounseling Notification 2013Santanu SamantaNo ratings yet
- INRT guidelines for early Hodgkin lymphomaDocument8 pagesINRT guidelines for early Hodgkin lymphomaSantanu SamantaNo ratings yet
- The Oncologist 2007 Erlotinib LungDocument12 pagesThe Oncologist 2007 Erlotinib LungSantanu SamantaNo ratings yet
- Radiobiology I: Direct and Indirect Radiation EffectsDocument36 pagesRadiobiology I: Direct and Indirect Radiation EffectsSantanu SamantaNo ratings yet
- 730 855 Hu Head NeckDocument44 pages730 855 Hu Head NeckSantanu SamantaNo ratings yet
- Units and Measurements: Radiation Physics Paper IDocument33 pagesUnits and Measurements: Radiation Physics Paper ISantanu SamantaNo ratings yet
- EPID RPT - 75Document26 pagesEPID RPT - 75Santanu SamantaNo ratings yet
- IMRT Basics: R. Alfredo C. Siochi, Ph.D. Juan Carlos Celi, PH.DDocument3 pagesIMRT Basics: R. Alfredo C. Siochi, Ph.D. Juan Carlos Celi, PH.DSantanu SamantaNo ratings yet
- Yakima Co (WA) Protocols 2010Document117 pagesYakima Co (WA) Protocols 2010Anthony James-Hartwell100% (1)
- Quezon City - Ang Tahanan NG Quezon City3Document11 pagesQuezon City - Ang Tahanan NG Quezon City3Jalimay CabadingNo ratings yet
- Interpersonal PsychotherapyDocument21 pagesInterpersonal PsychotherapyDr. Jayesh PatidarNo ratings yet
- Body Condition Scoring As A Tool For Dairy Herd Management PDFDocument5 pagesBody Condition Scoring As A Tool For Dairy Herd Management PDFfrankyNo ratings yet
- National Tuberculosis Program OverviewDocument21 pagesNational Tuberculosis Program OverviewJames RiedNo ratings yet
- Dcpip Food TestDocument14 pagesDcpip Food TestSyahir YaakopNo ratings yet
- HAAD Exam For Nurses Questions 2018Document46 pagesHAAD Exam For Nurses Questions 2018Asif Newaz100% (6)
- Peptic UlcerDocument4 pagesPeptic UlcerEris Abdul AzizNo ratings yet
- Treatment Planning Heterogeneity Vs Homogeneity Lung ProjectDocument13 pagesTreatment Planning Heterogeneity Vs Homogeneity Lung Projectapi-299138743No ratings yet
- Peplau's Interpersonal Relations Theory Power PointDocument10 pagesPeplau's Interpersonal Relations Theory Power PointCharisse Nicole DiazNo ratings yet
- FAQ Updated Must Read For Apple Therapy-9Document23 pagesFAQ Updated Must Read For Apple Therapy-9dpparkheNo ratings yet
- Artikel SAINMED Nian Afrian Nuari, M.kepDocument11 pagesArtikel SAINMED Nian Afrian Nuari, M.kepZueNo ratings yet
- Biomedical Waste ManagementDocument14 pagesBiomedical Waste ManagementdivyeshkpatelNo ratings yet
- 1 - O - Anuruddha KumaraDocument8 pages1 - O - Anuruddha Kumaraumapati 1505No ratings yet
- Cervical Dystonia Supplement - Summer 08Document8 pagesCervical Dystonia Supplement - Summer 08Kelly PhillipsNo ratings yet
- AtlsDocument32 pagesAtlsMahesh RajwalNo ratings yet
- Legal Medicine Review PDFDocument10 pagesLegal Medicine Review PDFGhie TangonanNo ratings yet
- General Principles of Pharmacology: Dr. GoverdhanDocument42 pagesGeneral Principles of Pharmacology: Dr. GoverdhanGoverdhan PeddireddyNo ratings yet
- Lap Ok RSGM Ronal HudaDocument23 pagesLap Ok RSGM Ronal HudaDwi SastrawanNo ratings yet
- 21841Document397 pages21841Sudheer JayaramNo ratings yet
- Karen Horney's Psychoanalytic Theory of NeurosisDocument26 pagesKaren Horney's Psychoanalytic Theory of NeurosisRafael SalamatNo ratings yet
- What's The Childbearing Age?: Woman's Reproductive Years Are Between Ages andDocument4 pagesWhat's The Childbearing Age?: Woman's Reproductive Years Are Between Ages andJeffrey MagadaNo ratings yet
- HerpesDocument9 pagesHerpesTilak ReddyNo ratings yet
- Mental Health CH 2Document6 pagesMental Health CH 2Gina GiammalvoNo ratings yet
- STEM Immersion Reflections in Physical Therapy, Nursing, and Medical TechnologyDocument4 pagesSTEM Immersion Reflections in Physical Therapy, Nursing, and Medical TechnologyLeonard Cyren LigutomNo ratings yet
- Abnormal-Uterine-Bleeding Case StudyDocument57 pagesAbnormal-Uterine-Bleeding Case StudyOneForAll :100% (1)
- Care of New BornDocument25 pagesCare of New BornNirupama KsNo ratings yet
- Organizaational ChangeDocument94 pagesOrganizaational ChangeAravind Kumar KotamsettyNo ratings yet
- Development Economics II Summary: Health, Calories, and ProductivityDocument9 pagesDevelopment Economics II Summary: Health, Calories, and Productivityshabrina larasatiNo ratings yet
- Psychology Presentation Chapter 10 - Life Span DevelopmentDocument15 pagesPsychology Presentation Chapter 10 - Life Span DevelopmentEduardo VillanuevaNo ratings yet