Professional Documents
Culture Documents
MI Chest Pain Assessment
Uploaded by
Dharline Abbygale Garvida AgullanaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MI Chest Pain Assessment
Uploaded by
Dharline Abbygale Garvida AgullanaCopyright:
Available Formats
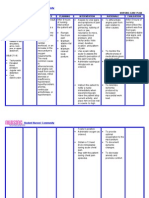
Myocardial Infarction ASSESSMENT DIAGNOSIS Subjective: The client reports of chest pain radiating to the left arm and
neck and back. Objective: Restlessness Facial grimacing Fatigue Peripheral cyanosis Weak pulse Cold and clammy skin Palpitations Shortness of breath Elevated temperature Pain scale of 8/10 Acute (Chest) Pain r/t myocardial ischemia resulting from coronary artery occlusion with loss/restriction of blood flow to an area of the myocardium and necrosis of the myocardium.
PLANNING STG: Within 1 hour of nursing interventions, the client will have improved comfort in chest, as evidenced by: States a decrease in the rating of the chest pain. Is able to rest, displays reduced tension, and sleeps comfortably. Requires decrease analgesia or nitroglycerin. LTG: The client will have an improved feeling of control as evidenced by verbalizing a sense of control over present situation and future outcomes within 2 days of nursing interventions.
INTERVENTION INDEPENDENT: 1. assess characteristics of chest pain, including location, duration, quality, intensity, presence of radiation, precipitating and alleviating factors, and as associated symptoms, have client rate pain on a scale of 1-10 and document findings in nurses notes. 2. obtain history of previous cardiac pain and familial history of cardiac problems.
RATIONALE
EVALUATION STG: Within 1 hour of nursing intervention, the client had improved comfort in chest, as evidenced by: States a decrease in the rating of the chest pain. Is able to rest, displays reduced tension, and sleeps comfortably. Requires decrease analgesia or nitroglycerin. Goal was met. LTG: The client had an improved feeling of control as evidenced by verbalizing a sense of control over present situation and future outcomes within 2 days of nursing intervention. Goal was met.
1. pain is indication of MI. assisting the client in quantifying pain may differentiate pre-existing and current pain patterns as well as identify complications.
2. this provides information that may help to differentiate current pain from previous problems and complications. 3. respirations may be increased as a result of pain and associate anxiety. 4. to reduce oxygen consumption and demand, to reduce competing stimuli and reduces anxiety. 5.pain control is a priority, as it indicates ischemia.
3. assess respirations, BP and heart rate with each episodes of chest pain. 4. maintain bedrest during pain, with position of comfort, maintain relaxing environment to promote calmness. 5. prepare for the administration of medications, and monitor response to drug therapy. Notify physician if pain does not abate.
6.istruct patient in nitroglycerin SL administration after hospitalization. Instruct patient in activity alterations and limitations. 7. instruct patient/family in medication effects, side-effects, contraindications and symptoms to report. DEPENDENT: 1. obtain a 12-lead ECG on admission, then each time chest pain recurs for evidence of further infarction as prescribed. 2. administer analgesics as ordered, such as morphine sulfate, meferidine of Dilaudid N. 3. administer betablockers as ordered.
6. to decrease myocardial oxygen demand and workload on the heart.
7. to promote knowledge and compliance with therapeutic regimen and to alleviate fear of unknown. 1. serial ECG and stat ECGs record changes that can give evidence of further cardiac damage and location of MI. 2. Morphine is the drug of choice to control MI pain, but other analgesics may be used to reduce pain and reduce the workload on the heart. 3. to block sympathetic stimulation, reduce heart rate and lowers myocardial demand. 4. to increase coronary blood flow and collateral circulation which can decrease pain due to ischemia.
4. administer calciumchannel blockers as ordered.
ASSESSMENT Subjective: The client reports of increased work of breathing associated with feelings of weakness and tiredness. Objective: Increased heart rate Increased blood pressure Dyspnea with exertion Pallor Fatigue and weakness Decreased oxygen saturation Ischemic ECG changes
DIAGNOSIS Activity Intolerance r/t cardiac dysfunction, changes in oxygen supply and consumption as evidenced by shortness of breath.
PLANNING STG: Within 3 days of nursing interventions, the client will be able to tolerate activity without excessive dyspnea and will be able to utilize breathing techniques and energy conservation techniques effectively. LTG: Within 5 days of nursing interventions, the client will be able to increase and achieve desired activity level, progressively, with no intolerance symptoms noted, such as respiratory compromise.
INTERVENTION INDEPENDENT: 1. monitor heart rate, rhythm, respirations and blood pressure for abnormalities. Notify physician of significant changes in VS. 2. Identify causative factors leading to intolerance of activity. 3. encourage patient to assist with planning activities, with rest periods as necessary. 4. instruct patient in energy conservation techniques. 5. assist with active or passive ROM exercises at least QID. 6. turn patient at least every 2 hours, and prn. 7. instruct patient in isometric and breathing exercises. 8. provide patient/family with exercise regimen, with written instructions. DEPENDENT: 1.Assisst patient with ambulation, as ordered, with progressive increases as patients tolerance
RATIONALE 1.changes in VS assist with monitoring physiologic responses to increase in activity.
EVALUATION STG: Within 3 days of nursing interventions, the client tolerated activity without excessive dyspnea and had been able to utilize breathing techniques and energy conservation techniques effectively. Goal was met. LTG: Within 5 days of nursing interventions, the client increased and achieved desired activity level, progressively, with no intolerance symptoms noted, such as respiratory compromise. Goal was met.
2. Alleviation of factors that are known to create intolerance can assist with development of an activity level program. 3. to help give the patient a feeling of self-worth and well-being. 4. to decrease energy expenditure and fatigue. 5.to maintain joint mobility and muscle tone. 6.to improve respiratory function and prevent skin breakdown. 7. to improve breathing and to increase activity level. 8. to promote self-worth and involves patient and his family with self-care. 1. to gradually increase the body to compensate for the increase in overload.
permits.
ASSESSMENT
DIAGNOSIS
PLANNING
INTERVENTION
RATIONALE
EVALUATION
Subjective: The client verbalizes questions regarding problems and misconceptions about his condition. Objective: Lack of improvement of previous regimen Inadequate follow-up on instructions given. Anxiety Lack of understan-ding.
Deficient Knowledge r/t new diagnosis and lack of understanding of medical condition.
STG: The client will be able to verbalize and demonstrate understanding of information given regarding condition, medications, and treatment regimen within 3 days of nursing interventions. LTG: The client will able to correctly perform all tasks prior to discharge.
INDEPENDENT: 1. monitor patients readiness to learn and determine best methods to use for teaching. 2. provide time for individual interaction with patient. 3. instruct patient on procedures that may be performed. Instruct patient on medications, dose, effects, side effects, contraindications, and signs/symptoms to report to physician. 4. instruct in dietary needs and restrictions, such as limiting sodium or increasing potassium. 5. provide printed materials when possible for patient/family to reviews. 6. have patient demonstrate all skills that will be necessary for postdischarge. 7. instruct exercises to be performed, and to avoid overtaxing activities. DEPENDENT: 1. refer patient to cardiac rehabilitation as ordered .
1. to promote optimal learning environment when patient show willingness to learn. 2. to establish trust. 3. to provide information to manage medication regimen and to ensure compliance.
STG: The client verbalized and demonstrated understanding of information given regarding condition, medications, and treatment regimen within 3 days of nursing interventions. Goal was met. LTG: The client had been able to correctly perform all tasks prior to discharge. Goal was met.
4. client may need to increase dietary potassium if placed on diuretics; sodium should be limited because of the potential for fluid retention. 5. to provide reference for the patient and family to refer. 6. to frovide information that patient has gained a full understanding of instruction. 7. these are helpful in improving cardiac function. 1. to provide further improvement and rehabilitation postdischarge.
You might also like
- Nursing Care Plan For Myocardial Infarction NCPDocument8 pagesNursing Care Plan For Myocardial Infarction NCPderic87% (15)
- NCP GrandcaseDocument5 pagesNCP GrandcaseSaima BataloNo ratings yet
- Nursing Assessment and Interventions for Acute Chest PainDocument3 pagesNursing Assessment and Interventions for Acute Chest PainAjay SupanNo ratings yet
- Managing Arteriosclerosis with Nursing CareDocument6 pagesManaging Arteriosclerosis with Nursing CareANCHAL SHARMANo ratings yet
- CP Intestinal Obstruction Nursing Care PlanDocument7 pagesCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaNo ratings yet
- NCP AnginaDocument3 pagesNCP AnginaShie LA100% (1)
- Nursing Care PlanDocument13 pagesNursing Care PlanCris Solis33% (3)
- Nursing Care Plan for Peptic UlcerDocument3 pagesNursing Care Plan for Peptic UlcerJefferson Baluyot PalmaNo ratings yet
- NCP For Mi PainDocument2 pagesNCP For Mi PainKahMallariNo ratings yet
- Nursing Care Plan For Diabetes Mellitus Diabetic KetoacidosisDocument17 pagesNursing Care Plan For Diabetes Mellitus Diabetic KetoacidosisJordz Placi100% (1)
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial InfarctionjamieboyRN88% (8)
- Nursing Care Plan for Mrs. Kanchan Rajput with Subarachnoid HemorrhageDocument21 pagesNursing Care Plan for Mrs. Kanchan Rajput with Subarachnoid HemorrhageDr-Sanjay SinghaniaNo ratings yet
- Care Plan Unstable AnginaDocument4 pagesCare Plan Unstable Anginaالغزال الذهبي50% (6)
- NCP DMDocument6 pagesNCP DMstara123No ratings yet
- Nursing Care PlanDocument14 pagesNursing Care PlanVin Landicho100% (1)
- FractureDocument1 pageFractureReechie TeasoonNo ratings yet
- Nursing Care PlanDocument15 pagesNursing Care PlanZhel Geron MercadoNo ratings yet
- Central Nervous System Nursing Care PlanDocument11 pagesCentral Nervous System Nursing Care PlanUday Kumar100% (1)
- Nursing Care Plan - Pericarditis PatientDocument2 pagesNursing Care Plan - Pericarditis Patientsandie_best78% (9)
- Coronary Artery Disease Care PlanDocument2 pagesCoronary Artery Disease Care PlanDanelle Harrison, RN100% (2)
- Nursing Care Plan For HypoglycemiaDocument3 pagesNursing Care Plan For HypoglycemiaPuteri AzmanNo ratings yet
- Emphysema: Presented By: Mis. M.K.Kaku Nursing TutorDocument10 pagesEmphysema: Presented By: Mis. M.K.Kaku Nursing TutorKaku ManishaNo ratings yet
- Nursing Care Plan (NCP) For A Patient With Angina PectorisDocument3 pagesNursing Care Plan (NCP) For A Patient With Angina PectorisKian Herrera100% (1)
- Scientific Explanation of Expected Outcomes and InterventionsDocument4 pagesScientific Explanation of Expected Outcomes and InterventionsGensen Cu RoxasNo ratings yet
- Medical Diagnosis: Bronchial Asthma Impaired Gas ExchangeDocument2 pagesMedical Diagnosis: Bronchial Asthma Impaired Gas ExchangeAndrea Chua BuadoNo ratings yet
- Anxiety NCPDocument2 pagesAnxiety NCPAnaleah MalayaoNo ratings yet
- NCP Heart BlockDocument3 pagesNCP Heart BlockEköw Santiago Javier33% (3)
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee BaluyotNo ratings yet
- NCP Ineffective Breathing PatternDocument4 pagesNCP Ineffective Breathing PatternSeika SouiNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanJoshua Pascasio100% (1)
- Cva NCP AnxietyDocument1 pageCva NCP AnxietyQueenElsaDeVeraNo ratings yet
- NCP PTBDocument2 pagesNCP PTBKath TalubanNo ratings yet
- NCP For MGDocument1 pageNCP For MGSandra MedinaNo ratings yet
- Acute Coronary Syndrome NCP 03Document6 pagesAcute Coronary Syndrome NCP 03AgronaSlaughterNo ratings yet
- NURSING CARE PLAN For Myocardial InfarctionDocument16 pagesNURSING CARE PLAN For Myocardial InfarctionFreisanChenMandumotan100% (1)
- Hypertension Nursing Care PlanDocument3 pagesHypertension Nursing Care PlanAsylla PajijiNo ratings yet
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- Instillation of Eye DropsDocument4 pagesInstillation of Eye DropsratnafadliNo ratings yet
- Disturbed Visual Sensory Perception Related: Nursing Care PlanDocument3 pagesDisturbed Visual Sensory Perception Related: Nursing Care PlanMae Therese B. MAGNONo ratings yet
- NCP HyperthermiaDocument1 pageNCP HyperthermiaPastor James PacadaljenNo ratings yet
- NCP LaminectomyDocument4 pagesNCP LaminectomyMark Zedrix MediarioNo ratings yet
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Nursing Care PlansDocument21 pages"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Nursing Care PlansCarl Elexer Cuyugan Ano100% (1)
- NCP - AnxietyDocument1 pageNCP - AnxietyNovie Carla100% (1)
- Assessing and Managing Risk of AspirationDocument6 pagesAssessing and Managing Risk of AspirationaianrNo ratings yet
- Asthma Care PlanDocument3 pagesAsthma Care PlanSam ParkNo ratings yet
- Body Weakness NCPDocument1 pageBody Weakness NCPtwicetrashNo ratings yet
- Nursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermDocument4 pagesNursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermErika Danalle ArceoNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanKath RubioNo ratings yet
- As Needed.: Environmental Stimuli 6Document4 pagesAs Needed.: Environmental Stimuli 6Nicole GumolonNo ratings yet
- NURSING CARE PLAN For Myocardial InfarctionDocument13 pagesNURSING CARE PLAN For Myocardial Infarctionbanyenye2593% (14)
- Lesson Plan ContentDocument6 pagesLesson Plan ContentSrijana Gurung100% (2)
- NCP For CHF 3 Activity IntoleranceDocument2 pagesNCP For CHF 3 Activity IntoleranceAngelyn ArdinesNo ratings yet
- NCP MiDocument8 pagesNCP MiPitaca Madiam Annabehl PaulNo ratings yet
- NCP FinalDocument18 pagesNCP FinalJessica Medina100% (1)
- NCPDocument7 pagesNCPBeverLyNo ratings yet
- Nursing Care Plan for a Diabetic Patient with Dehydration and FatigueDocument9 pagesNursing Care Plan for a Diabetic Patient with Dehydration and FatigueDanica Salinas100% (1)
- IUFDDocument13 pagesIUFDChristopher Lontoc0% (1)
- NCPDocument17 pagesNCPShayne Jessemae AlmarioNo ratings yet
- NCPDocument8 pagesNCPJose Benit DelacruzNo ratings yet
- Assessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationDocument10 pagesAssessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationApol Pen67% (3)
- Oncologic NursingDocument16 pagesOncologic NursingDharline Abbygale Garvida AgullanaNo ratings yet
- Grandparent 2Document20 pagesGrandparent 2Dharline Abbygale Garvida AgullanaNo ratings yet
- Without Advance Notice To The BorrowerDocument2 pagesWithout Advance Notice To The BorrowerDharline Abbygale Garvida AgullanaNo ratings yet
- Business Proposal Ilocos NorteDocument4 pagesBusiness Proposal Ilocos NorteDharline Abbygale Garvida AgullanaNo ratings yet
- Nursing PharmacologyDocument22 pagesNursing PharmacologyDharren Rojan Garvida Agullana100% (2)
- CHN&CDDocument7 pagesCHN&CDDharline Abbygale Garvida AgullanaNo ratings yet
- Mitosis ActivityDocument2 pagesMitosis ActivityDharline Abbygale Garvida AgullanaNo ratings yet
- CHN&CDDocument7 pagesCHN&CDDharline Abbygale Garvida AgullanaNo ratings yet
- Auditing Theory Key Concepts ExplainedDocument12 pagesAuditing Theory Key Concepts ExplainedKevin Ryan EscobarNo ratings yet
- SMEs Guide to IFRS for SMEsDocument130 pagesSMEs Guide to IFRS for SMEsDharren Rojan Garvida AgullanaNo ratings yet
- MedSurg Notes - Nurse's Clinical Pocket Guide (FA Davis, 2007)Document242 pagesMedSurg Notes - Nurse's Clinical Pocket Guide (FA Davis, 2007)Keron Hou97% (62)
- Chemistry TriviasDocument1 pageChemistry TriviasDharline Abbygale Garvida AgullanaNo ratings yet
- Mitosis ActivityDocument2 pagesMitosis ActivityDharline Abbygale Garvida AgullanaNo ratings yet
- December2012nletips Funda 121005040112 Phpapp02 PDFDocument6 pagesDecember2012nletips Funda 121005040112 Phpapp02 PDFJessamine Rochelle Reyes EsbertoNo ratings yet
- Pemphigus VulgarisDocument1 pagePemphigus VulgarisDharline Abbygale Garvida AgullanaNo ratings yet
- GrandparentDocument4 pagesGrandparentDharline Abbygale Garvida AgullanaNo ratings yet
- KorsakoffDocument4 pagesKorsakoffDharline Abbygale Garvida AgullanaNo ratings yet
- Planning and Organizing LecturesDocument3 pagesPlanning and Organizing LecturesDharline Abbygale Garvida AgullanaNo ratings yet
- Chemistry JokesDocument3 pagesChemistry JokesDharline Abbygale Garvida AgullanaNo ratings yet
- HypertensionDocument7 pagesHypertensionDharren Rojan Garvida AgullanaNo ratings yet
- NCPDocument3 pagesNCPDharline Abbygale Garvida Agullana100% (2)
- Tallest ManDocument1 pageTallest ManDharline Abbygale Garvida AgullanaNo ratings yet
- CancerDocument4 pagesCancerDharline Abbygale Garvida AgullanaNo ratings yet
- Industry BackgroundDocument1 pageIndustry BackgroundDharline Abbygale Garvida AgullanaNo ratings yet
- Meat Processing Industry in Ilocos Norte AnalysisDocument36 pagesMeat Processing Industry in Ilocos Norte AnalysisDharline Abbygale Garvida Agullana100% (1)
- Predisposing/ Non-Modifialbe Precipitating/ Modifiable: HepaticDocument2 pagesPredisposing/ Non-Modifialbe Precipitating/ Modifiable: HepaticDharline Abbygale Garvida AgullanaNo ratings yet
- Head Nursing Evaluation ToolDocument2 pagesHead Nursing Evaluation ToolDharline Abbygale Garvida Agullana100% (5)
- ScoliosisDocument4 pagesScoliosisDharline Abbygale Garvida AgullanaNo ratings yet
- Bone DiseasesDocument9 pagesBone DiseasesDharline Abbygale Garvida AgullanaNo ratings yet
- 10 DOH Approved Herbal Medicine: Prepared By: Washington, Luis D. Student Nurse BSN 2H-DDocument11 pages10 DOH Approved Herbal Medicine: Prepared By: Washington, Luis D. Student Nurse BSN 2H-DLuis WashingtonNo ratings yet
- Dengue AccomplishmentDocument4 pagesDengue AccomplishmentKylie GolindangNo ratings yet
- Bulimia NervosaDocument17 pagesBulimia NervosaJheanAlphonsineT.Means100% (1)
- Ebr MacalolotDocument4 pagesEbr Macalolotquen.chuaNo ratings yet
- Nursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationDocument10 pagesNursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationmalindaNo ratings yet
- 2006 Human and Developmental Toxicology - D. Bellinger (Informa, 2006) WW PDFDocument555 pages2006 Human and Developmental Toxicology - D. Bellinger (Informa, 2006) WW PDFGiovana BarbosaNo ratings yet
- Third Quarter Summative Test No. 4 EnglishDocument3 pagesThird Quarter Summative Test No. 4 EnglishJoanaNo ratings yet
- 2828100368063500002Document4 pages2828100368063500002sangama a0% (1)
- Articles of BERRIDGE, Edward WDocument11 pagesArticles of BERRIDGE, Edward WMuhammad Ata Ul MustafaNo ratings yet
- Protein and Amino Acid MetabolismDocument52 pagesProtein and Amino Acid MetabolismRisky OpponentNo ratings yet
- Preparation of Nurses To Disaster ManagementDocument10 pagesPreparation of Nurses To Disaster Managementai nisa hasnasariNo ratings yet
- Census August 8 - August 9, 2020Document6 pagesCensus August 8 - August 9, 2020Patrick JohnNo ratings yet
- PRAGYAN Vol 07 Issue 01Document92 pagesPRAGYAN Vol 07 Issue 01PRAGYAN,Tinsukia CollegeNo ratings yet
- First Division (G.R. No. 217036, August 20, 2018)Document12 pagesFirst Division (G.R. No. 217036, August 20, 2018)Emir MendozaNo ratings yet
- Fundamentals of Nursing10-19Document19 pagesFundamentals of Nursing10-19escolarNo ratings yet
- Article Dietschi VeenersDocument18 pagesArticle Dietschi VeenersRoberto PucNo ratings yet
- Cardiovascular Embryology StagesDocument109 pagesCardiovascular Embryology StagesBir Singh100% (1)
- MacroMinerals: Calcium, Phosphorus, Potassium, Sodium, Chloride, and MagnesiumDocument9 pagesMacroMinerals: Calcium, Phosphorus, Potassium, Sodium, Chloride, and MagnesiumDerek AtienzaNo ratings yet
- Laboratory Tests for Hemostasis EvaluationDocument5 pagesLaboratory Tests for Hemostasis EvaluationCMLNo ratings yet
- Slides 6 - ObturationDocument22 pagesSlides 6 - Obturationبراءة أحمد السلاماتNo ratings yet
- Inclusiveness: Prepared By: Dinke A. 2021Document131 pagesInclusiveness: Prepared By: Dinke A. 2021maria tafaNo ratings yet
- Nursing Care of Clients Undergoing Eye SurgeryDocument1 pageNursing Care of Clients Undergoing Eye SurgerySewyel GarburiNo ratings yet
- CucumberDocument25 pagesCucumberDa Nie LNo ratings yet
- Understand Glaucoma: Causes, Diagnosis and TreatmentDocument57 pagesUnderstand Glaucoma: Causes, Diagnosis and TreatmentDarshan SinghNo ratings yet
- Hand When You Need Them MostDocument9 pagesHand When You Need Them MostJim SchotterNo ratings yet
- Physiology Practice Questions: Parasympathetic Nervous System CharacteristicsDocument4 pagesPhysiology Practice Questions: Parasympathetic Nervous System CharacteristicsGregg ShanksNo ratings yet
- ICMIDocument4 pagesICMIKim MingyuNo ratings yet
- Shift work effects on doctors' healthDocument4 pagesShift work effects on doctors' healthHalilGutajNo ratings yet
- The Vanuatu Cooking Project ProposalDocument6 pagesThe Vanuatu Cooking Project ProposalBunga Melur MewangiNo ratings yet
- Dangers of Excess Sugar ConsumptionDocument2 pagesDangers of Excess Sugar ConsumptionAIDEN COLLUMSDEANNo ratings yet
- You Can't Joke About That: Why Everything Is Funny, Nothing Is Sacred, and We're All in This TogetherFrom EverandYou Can't Joke About That: Why Everything Is Funny, Nothing Is Sacred, and We're All in This TogetherNo ratings yet
- The Smartest Book in the World: A Lexicon of Literacy, A Rancorous Reportage, A Concise Curriculum of CoolFrom EverandThe Smartest Book in the World: A Lexicon of Literacy, A Rancorous Reportage, A Concise Curriculum of CoolRating: 4 out of 5 stars4/5 (14)
- The Importance of Being Earnest: Classic Tales EditionFrom EverandThe Importance of Being Earnest: Classic Tales EditionRating: 4.5 out of 5 stars4.5/5 (42)
- Welcome to the United States of Anxiety: Observations from a Reforming NeuroticFrom EverandWelcome to the United States of Anxiety: Observations from a Reforming NeuroticRating: 3.5 out of 5 stars3.5/5 (10)
- The House at Pooh Corner - Winnie-the-Pooh Book #4 - UnabridgedFrom EverandThe House at Pooh Corner - Winnie-the-Pooh Book #4 - UnabridgedRating: 4.5 out of 5 stars4.5/5 (5)
- The Inimitable Jeeves [Classic Tales Edition]From EverandThe Inimitable Jeeves [Classic Tales Edition]Rating: 5 out of 5 stars5/5 (3)
- The Asshole Survival Guide: How to Deal with People Who Treat You Like DirtFrom EverandThe Asshole Survival Guide: How to Deal with People Who Treat You Like DirtRating: 4 out of 5 stars4/5 (60)
- Lessons from Tara: Life Advice from the World's Most Brilliant DogFrom EverandLessons from Tara: Life Advice from the World's Most Brilliant DogRating: 4.5 out of 5 stars4.5/5 (42)
- Other People's Dirt: A Housecleaner's Curious AdventuresFrom EverandOther People's Dirt: A Housecleaner's Curious AdventuresRating: 3.5 out of 5 stars3.5/5 (104)
- The Comedians in Cars Getting Coffee BookFrom EverandThe Comedians in Cars Getting Coffee BookRating: 4.5 out of 5 stars4.5/5 (8)
- Sexual Bloopers: An Outrageous, Uncensored Collection of People's Most Embarrassing X-Rated FumblesFrom EverandSexual Bloopers: An Outrageous, Uncensored Collection of People's Most Embarrassing X-Rated FumblesRating: 3.5 out of 5 stars3.5/5 (7)
- Humorous American Short Stories: Selections from Mark Twain, O. Henry, James Thurber, Kurt Vonnegut, Jr. and moreFrom EverandHumorous American Short Stories: Selections from Mark Twain, O. Henry, James Thurber, Kurt Vonnegut, Jr. and moreNo ratings yet
- Si-cology 1: Tales and Wisdom from Duck Dynasty's Favorite UncleFrom EverandSi-cology 1: Tales and Wisdom from Duck Dynasty's Favorite UncleRating: 4.5 out of 5 stars4.5/5 (16)
- The Best Joke Book (Period): Hundreds of the Funniest, Silliest, Most Ridiculous Jokes EverFrom EverandThe Best Joke Book (Period): Hundreds of the Funniest, Silliest, Most Ridiculous Jokes EverRating: 3.5 out of 5 stars3.5/5 (4)

























































































































![The Inimitable Jeeves [Classic Tales Edition]](https://imgv2-1-f.scribdassets.com/img/audiobook_square_badge/711420909/198x198/ba98be6b93/1712018618?v=1)