Professional Documents
Culture Documents
Journal of Immunological Methods: Research Paper
Uploaded by
davdavdavdavdavdavdaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal of Immunological Methods: Research Paper
Uploaded by
davdavdavdavdavdavdaCopyright:
Available Formats
Journal of Immunological Methods 338 (2008) 5862
Contents lists available at ScienceDirect
Journal of Immunological Methods
j o u r n a l h o m e p a g e : w w w. e l s ev i e r. c o m / l o c a t e / j i m
Research paper
Determination of blood leukocyte concentration with constant volume acquisition on a ow cytometer is comparable to individualized single platform testing with beads as internal reference standard
Susan Hansen, Ronald Dahl, Hans Jrgen Hoffmann
Department of Respiratory Diseases, Aarhus University and Hospital, Building 2b, Nrrebrogade 44, DK 8000 Aarhus C, Denmark
a r t i c l e
i n f o
a b s t r a c t
Flow cytometers have a constant ow rate. This enables ow cytometers to measure leukocyte concentrations in a determined volume by acquiring data at a xed rate over a xed time and is called constant volume acquisition (CVA). The volume aspirated by a FACS Calibur ow cytometer in 4 min at a high rate has a median of 163 l (IQR 156170) with TruCount tubes. Leukocyte concentrations of 26 healthy volunteers were measured twice on up to four occasions with a BrkerTrk chamber, by single platform technology (SPT) with TruCount tubes and on the same data set using CVA. Total leukocyte concentrations determined by CVA correlated better with measurements in a BrkerTrk (BT) chamber than with SPT. Concentrations determined with CVA were 1.86% higher than with BT whereas SPT data were 5.35% higher than BT (p b 0.001), and 3.36% higher than CVA (p b 0.001). At leukocyte concentrations b 6 million/ml SPTcorrelated better with BT than CVA. The SPT measurement may be more variable because it depends on measurement of the number of beads aliquoted, the number of beads and leukocytes aspirated, where both BT counting and CVA measurements only depend on the number of leukocytes counted. CVA with PanLeukoGating can be established using microscopy as a reference, and is comparable to BT chamber and SPT determination. Leukocyte concentrations can be measured with CVA on ow cytometers in research and clinical settings. 2008 Elsevier B.V. All rights reserved.
Article history: Received 27 April 2008 Received in revised form 4 July 2008 Accepted 10 July 2008 Available online 3 August 2008 Keywords: Flow cytometry Single platform testing CD45 PanLeukoGating
1. Introduction Blood leukocyte concentrations are an essential complement to the fractional changes of leukocyte subsets. The best known blood leukocyte parameter is the CD4 concentration during infection with the human immunodeciency virus (HIV) that becomes critical when it decreases below 200 cells/ l (Yarchoan et al., 1991). We have recently investigated the frequency of regulatory T cells (Hoffmann et al., 2007) and changes in basophil granulocyte, regulatory T cell (T reg) and plasmacytoid (pDC) and myeloid dendritic cell subsets during
Abbreviations: BT chamber, BrkerTrk chamber; CVA, constant volume acquisition; SPT, single platform testing. Corresponding author. Department of Respiratory Diseases, Aarhus University and Hospital, Building 2b, Nrrebrogade 44, DK 8000 Aarhus C, Denmark. Tel.: +45 89492107; fax: +45 89492110. E-mail address: hans.jurgen.hoffmann@ki.au.dk (H.J. Hoffmann). 0022-1759/$ see front matter 2008 Elsevier B.V. All rights reserved. doi:10.1016/j.jim.2008.07.010
allergen provocation (Hoffmann et al., 2006), and used a two platform method to determine absolute leukocyte changes. Single platform determination of leukocyte concentration has been developed and is still being rened for monitoring of HIV status (Schnizlein-Bick et al., 2000; Martini et al., 2007). Typically, beads are added to the blood sample before staining, and a lyse-no-wash method is employed (Nicholson et al., 1997). However, even though only one tube is employed, three measurements are made to calculate leukocyte concentration by this method; measurements are based on determination of numbers of leukocytes, aliquoted beads and acquired beads. Each measurement comes with some error, which is compounded as the terms are multiplied together. The present generation of ow cytometers has stable ow and constant volume (Bergeron et al., 2003). The PanLeukoGating procedure using CD45 (Glencross et al., 2002) has been developed to calibrate ow cytometers to analyse leukocytes in a constant volume dened by a constant acquisition time (Storie et al., 2003; Walker et al., 2006).
S. Hansen et al. / Journal of Immunological Methods 338 (2008) 5862
59
We adapted this method to our project, investigating ux of leukocyte subsets due to the allergen injection in specic immunotherapy (Bousquet et al., 1987), and compared leukocyte concentrations determined by SPT measurement with constant time acquisition and measurement in a BrkerTrk chamber as our predicate method. 2. Materials and methods
brightly uorescent polystyrene beads were used to determine the absolute concentrations of leukocytes, by using the formula: Total cell concentration = (number of cell events counted pr tube number of beads counted pr tube) / (total number of beads in tube sample volume pr tube). According to manufacturer's suggestions, bead doublets were included in the bead gate. 2.5. Statistics
2.1. Participants The Ethics Committee of Aarhus County approved the project. Adult patients (n = 20) to be treated with venom injection for wasp allergy by a standardized protocol (Bousquet et al., 1987) and controls not treated with allergy vaccination (n = 6) were recruited. Two patients withdrew because of lack of interest. Cells were counted in 4 ml heparinised blood before SCIT and 30 min after the last venom injection at the 1st, 4th, 7th visits and at maintenance dose. In controls, cells were counted at similar intervals. For each of 18 patients and 6 controls, two blood samples were analysed at each visit. Each participant visited the clinic up to four times, at intervals of 47 weeks. Patients were seen on 44 days from January to October 2007. 2.2. Microscopy Blood leukocyte concentrations were determined by microscopic counting, using a BrkerTrk counting chamber (0.0025 mm2, 0.5 l). 475 l dilution uid was mixed with 25 l heparinised blood and approximately 2 glass pearls were added. The dilution factor was 1/20. The blood leukocyte concentration can be calculated as number of leukocytes counted 0.04 cells/ml. 2.3. Flow cytometry Total leukocytes and T cells were measured with TruCount tubes (Catalogue Nr 340334) according to manufacturer's instructions. Heparinised blood (50 l) was labelled within 1 h of venipuncture with titrated amounts of antibodies. To identify leukocytes CD45 PerCP (10 l, Catalogue Nr 345809) was used in a tube designed to identify and determine the concentration of leukocytes (CD45+), plasmacytoid dendritic cells (CD45+Lin1CD123+HLA DR+) and basophil granulocytes (CD45+Lin1CD123+HLA DR) using Lin1 FITC, CD123 PE and HLA DR APC (Hoffmann et al., 2006). FACS Lysing Solution (450 l) was added to the TruCount tubes for 15 min, and the cells were counted with a FACS Calibur for 4 min at a high ow rate acquisition using Cell Quest Software. High ow rate analysis gives the lowest intra-assay CVs for cell counts (Storie et al., 2003). Compensation controls were generated each day with Comp beads (Catalogue nr 51-90-9001291) and all antibodies. All reagents and equipment for ow cytometry were from Becton-Dickinson, San Jose, CA, USA. 2.4. Data analysis Data were compensated with compensation beads prepared on each day, and analysed in batch with FlowJo version 8.2 (Fig. 1). TruCount tubes containing a known number of
Fig. 1. Representative gating procedure for determining bead and leukocyte numbers. Fresh heparinised blood was labelled with titrated amounts of CD45 PerCP in a TruCount tube, and was incubated and lysed with BD lysis reagent. The sample was acquired with a FACS Calibur ow cytometer at high speed set to trigger on PerCP for 4 min.
Counting uncertainty was assumed to equal the square root of the number of counted events. Statistical signicance of difference between results was assessed using a paired ttest if data was normally distributed, or a Wilcoxon Signed Rank test. p b 0.05 was considered statistically signicant. Association between leukocytes measured with microscope and ow cytometer analysed with the Pearson's Correlation Coefcient (SPSS 11.0.0, 2001). Missing data was excluded from the analyses. 3. Results 3.1. Calculation of constant volume acquisition (CVA) volume The mean rate of bead acquisition was 63.34 3.15 beads/s (CV = 4.97%) and the median volume aspirated in analysis of leukocytes was 163 l (IQR 156170 l). The aspirated volume contained 14.8 l blood. 3.2. Reproducibility of determinations by microscope, SPT and CVA The reproducibility of repeated BT counting (n = 7) and SPT enumerations (n = 2, four repeats acquired consecutively on the same day) was determined on blood of independent
60
S. Hansen et al. / Journal of Immunological Methods 338 (2008) 5862
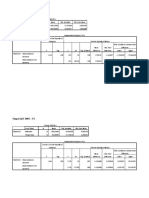
Table 1 Comparison of statistical strength of the measurements Method Microscopy TruCount, bead number CVA and SPT, cell number Material Donor 1 Donor 2 Beads Donor 3 Repeats 7 7 4 4 Number of events 290 129 14,160 89,712 SD 16 3 454 5669 CV (%) 5.52 2.33 3.21 6.32 100/n 5.87 8.80 0.84 0.33 Leukocyte concentration 11,611 5142 6239
Vastly different numbers of events were counted when counting cells by microscopy, and TruCount beads and cells in the ow cytometer. The effect of this difference on precision is illustrated here; the counting method and material counted are listed, and the number of repeats, and the mean number of events counted with each method are given. The CV is calculated from the observed variation, and the theoretical CV is calculated as 100/n. The leukocyte number determined is also given, as this may inuence the actual number of events evaluated.
persons (Table 1). The observed precision was comparable for all measurements, but was less than expected from statistical theory. 3.3. Validation of SPT and CVA algorithms against microscopy CVA and SPT were compared to BT by linear regression; CVA = BT 0.9527 + 349,455 cells/ l ( R 2 = 0.6868, n = 147, p b 0.001) and SPT= BT 0.7864+ 1,092,629 cells/l (R2 =0.7895, n = 147, p b 0.001) (Fig. 2a). In a BlandAltman analysis (Fig. 2b, c and d) the spread of the data was similar for CVA and SPT compared to BT counting (Fig. 2b and d). The mean difference of leukocyte concentrations determined by the CVA and SPT methods and BT counting were 1.86% (IQR 6.779.85%, ns) and 5.35% (IQR 2.4214.04%, p b 0.001), respectively. The difference between CVA and SPT determinations was signicant (3.36%, IQR 1.37%9.03%; p b 0.001). The median difference from the predicate BT counting method to SPT was signicantly larger than to CVA at high leukocyte concentrations, but was less at low leukocyte concentrations (Fig. 2e). The binned net differences between the predicate BT counting method and CVA or SPT were symmetrical around the line of equality (Fig. 2f). 4. Discussion In ow cytometric analysis, cell concentrations are often given as percentage change without regard to the absolute cell concentrations. For economic reasons, absolute leukocyte concentrations have primarily been the domain of clinical immunology and infections disease, as a decrease of absolute CD4 T cell concentrations to below 200 cells/l is a critical threshold in the progression of HIV infection (Yarchoan et al., 1991). Here we show that CVA can be applied in a research setting to determine changes in blood leukocyte concentrations to give results comparable to both BT counting and SPT. In a clinical experiment changes in basophil granulocytes and pDC were investigated during specic immunotherapy by venom injection of persons allergic to wasp sting (Hansen, Dahl and Hoffmann, in preparation). Total leukocyte concentrations were determined as quality control tool by BT counting, SPT and CVA. 4.1. Calculation of constant volume acquisition (CVA) volume The ow rate of ow cytometers is constant enough to allow aspiration of a xed volume in a predetermined time (Bergeron et al., 2003; Storie et al., 2003). The CV of the rate determined here, 4.97%, was comparable to that reported by
previously for a Calibur; b 6% (Bergeron et al., 2003). To utilize CVA one may adopt an approach similar to the one described here where a ow cytometric method is standardized against an accepted predicate method, avoiding the complexity of adjusting for viscosity (Storie et al., 2003; Walker et al., 2006). The ow rate of the cytometer(s) should be checked regularly (N four times on one day to establish a mean event number collected with CV, then weekly followed by monthly, and after each service of the instrument) with leukocytes of known concentration (as has been suggested by Walker et al., 2006) or with a lot of beads reserved for this purpose. The method requires identication of CD45+ leukocytes for PanLeukoGating (Glencross et al., 2002) for comparison to leukocyte concentration determined by BT counting. The volume analysed here in 4 min was 163 l. Others have found that 100 l were analysed in 2 min (Storie et al., 2003), suggesting that it is important to calibrate each ow cytometer individually with sufcient readings and to monitor it continuously. Digital ow cytometers have better algorithms to identify and discard doublets. The ow rate should thus be set to minimize doublet generation, yet maximize the number of events counted as this improves the counting accuracy. As long as both calibration and experimental measurements are done at the same ow rate in the same medium, the improved doublet discrimination should not affect accuracy. In a series of eight acquisitions of the same sample of blood to determine reproducibility, the bead and cell number did not decrease linearly with time. Data for this analysis had been acquired over 10 months, and the instrument had been serviced (preventive maintenance) twice in this period. There was no clear association between service and variation. The blood volume analysed was 14.8 l. This is nearly 30 times more than evaluated in the BT chamber. It should thus be possible to enumerate small cell populations. The normal range of leukocyte concentrations is from 300010,000 cells/l; the present data ranged from 3320 to 14,040 cells/l. 4.2. Reproducibility of determinations by microscope, and ow cytometry with SPT or with constant volume There was little correlation between the expected variation (proportional to n/n) and the determined variation (b 6%) of data collected in a BrkerTrk chamber, and of repeated analyses of TruCount tubes (3%). In other trials to determine the reproducibility of CD4 counts for monitoring of HIV patients, the intralaboratory variation was 12%, and the interlaboratory variation was 3% for CD4 T cell counts (Schnizlein-Bick et al., 2000).
S. Hansen et al. / Journal of Immunological Methods 338 (2008) 5862
61
Fig. 2. Comparison of procedures for evaluation of leukocyte concentrations (a) SPT and CVA determinations are plotted as function of the predicate BT chamber counts. (bd) BlandAltman plots comparing CVA with BT counts and SPT. The median and CV are indicated by solid and dotted lines. (e) Distribution of data at low (30006000 cells/l), medium (600012,000 cells/l) and high (N 12,000 cells/l) leukocyte concentrations was determined for the three methods compared as medians and quartiles, (f) Histogram of differences of all measures between the predicate method, BT counting, and SPT and CVA.
4.3. Validation of SPT and CVA algorithms against microscopy BT counting chamber is the predicate method in our laboratory. This is different to the approach that a Clinical Im-
munology laboratory would have; they would compare data with a hematology instrument or with a SPT method (Nicholson et al., 1997; Schnizlein-Bick et al., 2000; Storie et al., 2003). Calculating leukocyte concentrations on the basis of a constant
62
S. Hansen et al. / Journal of Immunological Methods 338 (2008) 5862
volume were more similar to microscopic leukocyte counts than concentrations determined with a daily TruCount bead number. As the calculations were done on the same data set, the only difference between CVA and SPT determinations was that the volume in SPT was based on the both the actual number of beads in an individual tube and the number of beads acquired with the cells, compared with an average volume used in CVA. Thus the variation introduced in the SPT tubes is likely to be due to variation in precision of bead measurements. The fact that the number of beads in each TruCount tube may vary, and may vary more than the volume aspirated by a ow cytometer over constant time, has not been proposed before. As CVA used the same data les as the SPT, there were no differences in pipetting or viscosity. This conrms and extends the result of earlier studies (Bergeron et al., 2003; Storie et al., 2003; Walker et al., 2006) in which the volume sampled during a xed amount of time was sufciently accurate to calculate absolute cell concentrations. The single platform test using TruCount tubes has previously been shown to be different from other single platform methods (Nicholson et al., 1997; Schnizlein-Bick et al., 2000), but is thought to be more accurate than two platform evaluation in interlaboratory comparisons (Schnizlein-Bick et al., 2000). The difference between SPT and two platform measurements was attributed to hematology instruments that were part of the dual platform. 5. Conclusion Flow cytometry is a versatile and powerful technique that allows statistical analysis at the single cell level. The expansion of detection systems to more than 15 simultaneous uorochomes has received much coverage in scientic literature, and it is surprising that the studies by Bergeron et al. (2003) and Storie et al. (2003) on which this work is based, have not gained as much popularity. In this study we show that it is possible to determine leukocyte concentration by acquiring data for a xed time provided the acquisition volume of the ow cytometer is monitored. Combined with the digital revolution in computing and the expansion of the number of parameters detected, CVA will make ow cytometry even more versatile, and more precise. CVA is the method of choice as it is signicantly cheaper than SPT, and less labour intensive than BT counting.
Acknowledgements The technical assistance of Anne Marie Toft, and the participation of the immunotherapy patients and control persons, are appreciated. The project was funded by Aarhus University Hospital, the Velux Foundation and the Aarhus University Research Foundation. References
Bergeron, M., Lustyik, G., Phaneuf, S., Ding, T., Nicholson, J.K.A., Janossy, G., Shapiro, H., Barnett, D., Mandy, F., 2003. Stability of currently used cytometers facilitates the identication of pipetting errors and their volumetric operation: time can tell all. Cytometry B Clin. Cytom. 52, 37. Bousquet, J., Mller, U.R., Dreborg, S., Jarisch, R., Malling, H.J., Mosbech, H., Urbanek, R., Youlten, L., 1987. Immunotherapy with Hymenoptera venoms. Position paper of the Working Group on Immunotherapy of the European Academy of Allergy and Clinical Immunology. Allergy 42, 401. Glencross, D., Scott, L.E., Jani, I.V., Barnett, D., Janossy, G., 2002. CD45-assisted PanLeucogating for accurate, cost-effective dual-platform CD4+ T-cell enumeration. Cytometry 50, 69. Hoffmann, H.J., Skjold, T., Raithel, M., Adolf, K., Hilberg, O., Dahl, R., 2006. Response of respiratory our allergics in an ingested our challenge may involve plasmacytoid dendritic cells, CD25+ T cells and CD152+ T cells. Int. Arch. Allergy Immunol. 140, 252. Hoffmann, H.J., Malling, T.M., Topcu, A., Ryder, L.P., Nielsen, K.R., Varming, K., Dahl, R., Omland, O., Sigsgaard, T., 2007. CD4(dim)CD25(bright) Treg cell frequencies above a standardized gating threshold are similar in asthmatics and controls. Cytometry A 71, 371. Martini, F., D'Ofzi, G., Girardi, E., Vitale, A., Cimini, E., Mollicone, B., Vlassi, C., Aiuti, F., 2007. The 2005 Italian Quality Control Study for the evaluation of CD4 cells in centers involved in the treatment of HIV type 1 patients. AIDS Res. Hum. Retroviruses 23, 777. Nicholson, J.K., Stein, D., Mui, T., Mack, R., Hubbard, M., Denny, T., 1997. Evaluation of a method for counting absolute numbers of cells with a ow cytometer. Clin. Diagn. Lab. Immunol. 4, 309. Schnizlein-Bick, C.T., Spritzler, J., Wilkening, C.L., Nicholson, J.K., O'Gorman, M.R., 2000. Evaluation of TruCount absolute-count tubes for determining CD4 and CD8 cell numbers in human immunodeciency virus-positive adults. Site Investigators and The NIAID DAIDS New Technologies Evaluation Group. Clin. Diagn. Lab. Immunol. 7, 336. Storie, I., Sawle, A., Goodfellow, K., Whitby, L., Granger, V., Reilly, J.T., Barnett, D., 2003. Flow rate calibration I: a novel approach for performing absolute cell counts. Cytometry B Clin. Cytom. 55, 1. Walker, C.L., Whitby, L., Granger, V., Storie, I., Reilly, J.T., Barnett, D., 2006. Flow rate calibration. III. The use of stabilized biostandards to calibrate the ow rate and calculate absolute CD4+ T-cell counts. Cytometry B Clin. Cytom. 70, 154. Yarchoan, R., Venzon, D.J., Pluda, J.M., Lietzau, J., Wyvill, K.M., Tsiatis, A.A., Steinberg, S.M., Broder, S., 1991. CD4 count and the risk for death in patients infected with HIV receiving antiretroviral therapy. Ann. Intern. Med. 115, 184.
You might also like
- Evaluation of PCV, Cd4 T Cell Counts, ESR and WBC Counts in Malaria Infected Symptomatic HIV (Stage 11) Male HIV/ Aids Subjects On Antiretroviral Therapy (Art) in Nnewi, South Eastern NigeriaDocument5 pagesEvaluation of PCV, Cd4 T Cell Counts, ESR and WBC Counts in Malaria Infected Symptomatic HIV (Stage 11) Male HIV/ Aids Subjects On Antiretroviral Therapy (Art) in Nnewi, South Eastern NigeriaIOSR Journal of PharmacyNo ratings yet
- Use of Fresh Blood For Quality Control: Erythrocyte Sedimentation RateDocument6 pagesUse of Fresh Blood For Quality Control: Erythrocyte Sedimentation RateTriana AmaliaNo ratings yet
- Perioperative Reliability of An On-Site Prothrombin Time Assay Under Different Haemostatic ConditionsDocument4 pagesPerioperative Reliability of An On-Site Prothrombin Time Assay Under Different Haemostatic Conditionsbelqis ratuNo ratings yet
- Immuno-Monitoring of CD8+ T Cells in Whole Blood Versus PBMC SamplesDocument8 pagesImmuno-Monitoring of CD8+ T Cells in Whole Blood Versus PBMC SamplesastheniiaNo ratings yet
- VCC VancouverStyleGuideDocument6 pagesVCC VancouverStyleGuideLink BuiNo ratings yet
- Reliability of Parameters of Complete Blood Count With Different Storage PDFDocument6 pagesReliability of Parameters of Complete Blood Count With Different Storage PDFLink BuiNo ratings yet
- Changes in Treg Numbers and Activity in Papillary Thyroid Carcinoma With and Without Hashimoto's ThyroiditisDocument8 pagesChanges in Treg Numbers and Activity in Papillary Thyroid Carcinoma With and Without Hashimoto's ThyroiditisjameeraNo ratings yet
- 393 FullDocument6 pages393 FullYaser MNo ratings yet
- Implementation of Changes in Complete Blood Count and Red Cell Indices of Whole Blood IncubatedDocument3 pagesImplementation of Changes in Complete Blood Count and Red Cell Indices of Whole Blood IncubatedEditor IJTSRDNo ratings yet
- Guidance For Storing Blood Samples in Laboratories Performingcomplete Blood Count With DifferentialDocument6 pagesGuidance For Storing Blood Samples in Laboratories Performingcomplete Blood Count With Differentialimran ahmed siddiquiNo ratings yet
- Ok 1Document6 pagesOk 1cydolusNo ratings yet
- Characterization of Circulating Tumor Cells by Fluorescence in Situ HybridizationDocument8 pagesCharacterization of Circulating Tumor Cells by Fluorescence in Situ HybridizationNidhi JaisNo ratings yet
- Short Communication: Storage Stability of Commonly Used Haematological Parameters at 33 °CDocument7 pagesShort Communication: Storage Stability of Commonly Used Haematological Parameters at 33 °CSyarifah Tridani FitriaNo ratings yet
- Int J Lab Hematology - 2022 - Marinov - Validation of A Single Tube 3 Colour Immature Red Blood Cell Screening Assay ForDocument7 pagesInt J Lab Hematology - 2022 - Marinov - Validation of A Single Tube 3 Colour Immature Red Blood Cell Screening Assay ForMaria SousaNo ratings yet
- Diagnostic Accuracy of Xpert MTB/RIF On Bronchoscopy Specimens in Patients With Suspected Pulmonary TuberculosisDocument6 pagesDiagnostic Accuracy of Xpert MTB/RIF On Bronchoscopy Specimens in Patients With Suspected Pulmonary TuberculosisMARTIN FRANKLIN HUAYANCA HUANCAHUARENo ratings yet
- Evaluation of The Roche Coaguchek Xs Handheld Coagulation Analyzer in A Cardiac Outpatient ClinicDocument4 pagesEvaluation of The Roche Coaguchek Xs Handheld Coagulation Analyzer in A Cardiac Outpatient Clinicgladi panitia ltlNo ratings yet
- MMC 1Document5 pagesMMC 1giovanniNo ratings yet
- RT Real-Time PCR Detection of HRVDocument8 pagesRT Real-Time PCR Detection of HRVNashiely RdzNo ratings yet
- Immature GranulocytesDocument10 pagesImmature Granulocytespieterinpretoria391No ratings yet
- PCT FeverDocument6 pagesPCT FeverAndi BintangNo ratings yet
- Carraro 2013 RSBMTV 46 N 2 P 161Document5 pagesCarraro 2013 RSBMTV 46 N 2 P 161Emerson CarraroNo ratings yet
- Flow Cytometric Analysis of Normal and Reactive SpleenDocument10 pagesFlow Cytometric Analysis of Normal and Reactive SpleenmisterxNo ratings yet
- Extended Leukocyte Differential Count and C-Reactive Protein inDocument8 pagesExtended Leukocyte Differential Count and C-Reactive Protein ini chen chenNo ratings yet
- Some Hemostatic Parameters of Patients With Pulmonary Tuberculosis Infection Attending Aminu Kano Teaching Hospital Kano, NigeriaDocument5 pagesSome Hemostatic Parameters of Patients With Pulmonary Tuberculosis Infection Attending Aminu Kano Teaching Hospital Kano, Nigeriaaminu ibrahim gadakaNo ratings yet
- Erroneous Automated Optical Platelet Counts PDFDocument8 pagesErroneous Automated Optical Platelet Counts PDFfar faraNo ratings yet
- JR 2 AnasDocument7 pagesJR 2 AnasCitra DewiNo ratings yet
- Novel Parameters of Extended Complete Blood Cell Count UnderDocument6 pagesNovel Parameters of Extended Complete Blood Cell Count Underi chen chenNo ratings yet
- 15dec05 Guide To Flow Cytometry Absolute Cell Counting Chapter17Document8 pages15dec05 Guide To Flow Cytometry Absolute Cell Counting Chapter17joanaritalexandre2552No ratings yet
- Journal Pone 0043702Document8 pagesJournal Pone 0043702Muhamad Wirawan AdityoNo ratings yet
- Jomb 40 3 2103252UDocument9 pagesJomb 40 3 2103252Ualesraa jawharatNo ratings yet
- Evaluation of The Effect of Temperature and Time of Incubation On Complete Blood Count (CBC) TestsDocument4 pagesEvaluation of The Effect of Temperature and Time of Incubation On Complete Blood Count (CBC) TestsYaser MNo ratings yet
- Ishage ProtocolDocument9 pagesIshage ProtocolEfrain E. Cabrera RojasNo ratings yet
- Diagnostic Value of Procalcitonin For Acute Complicated AppendicitisDocument10 pagesDiagnostic Value of Procalcitonin For Acute Complicated AppendicitisAnonymous 4K2TOtpfNo ratings yet
- Whole Blood MiceDocument6 pagesWhole Blood MiceFiy Jannatin AliyahNo ratings yet
- (13360329 - Endocrine Regulations) Elevated Neutrophil-Lymphocyte Ratio in Patients With Euthyroid Chronic Autoimmune ThyreotidisDocument6 pages(13360329 - Endocrine Regulations) Elevated Neutrophil-Lymphocyte Ratio in Patients With Euthyroid Chronic Autoimmune Thyreotidisjournal proNo ratings yet
- Impact of Low Volume Citrate Tubes On Results of First Line Hemostasis TestingDocument6 pagesImpact of Low Volume Citrate Tubes On Results of First Line Hemostasis TestingSidney WatersNo ratings yet
- Jurnal Meningitis TBDocument5 pagesJurnal Meningitis TBPutri KartikaNo ratings yet
- Estimating platelet counts: auto analyzer vs smear methodsDocument7 pagesEstimating platelet counts: auto analyzer vs smear methodsLaboratorium RS BELLANo ratings yet
- 1 s2.0 S0085253815349693 MainDocument5 pages1 s2.0 S0085253815349693 MainSotero MoralesNo ratings yet
- Hemostatic Changes in Active Pulmonary TuberculosisDocument6 pagesHemostatic Changes in Active Pulmonary Tuberculosisdvt nsNo ratings yet
- 2 A Rapid High-Precision Flow Cytometry Based Technique For Total WhiteDocument14 pages2 A Rapid High-Precision Flow Cytometry Based Technique For Total WhitePablo LópezNo ratings yet
- Evaluation of I Stat Clinical&Laboratory ScienceDocument13 pagesEvaluation of I Stat Clinical&Laboratory ScienceTony ChenNo ratings yet
- Chaves 2005 PDFDocument5 pagesChaves 2005 PDFWa Nur Arlin RahmadhantyNo ratings yet
- Stationary Versus Agitated Storage of Whole Blood.6 PDFDocument5 pagesStationary Versus Agitated Storage of Whole Blood.6 PDFAngel CallesNo ratings yet
- JM 002076Document5 pagesJM 002076Malú CarranzaNo ratings yet
- Splenic Blood Flow and Intrasplenic Platelet Kinetics in Relation To Spleen VolumeDocument5 pagesSplenic Blood Flow and Intrasplenic Platelet Kinetics in Relation To Spleen VolumedenisegmeloNo ratings yet
- Platelet Counting by The Coulter LH 750, Sysmex XE 2100Document7 pagesPlatelet Counting by The Coulter LH 750, Sysmex XE 2100blanket_thNo ratings yet
- Validacion de AgaDocument7 pagesValidacion de AgaSATURNONo ratings yet
- Automated Urine Sediment AnalyzerDocument5 pagesAutomated Urine Sediment AnalyzerCarolinaAngelaNo ratings yet
- Diagnostic Value of C-Reactive Protein and Hematological Parameters in Neonatal SepsisDocument9 pagesDiagnostic Value of C-Reactive Protein and Hematological Parameters in Neonatal SepsisIOSRjournalNo ratings yet
- Efficacy of Ascitic Acid Dipstick Leukocyte Esterase Activity in Early Diagnosis of Spontaneous Bacterial PeritonitisDocument6 pagesEfficacy of Ascitic Acid Dipstick Leukocyte Esterase Activity in Early Diagnosis of Spontaneous Bacterial PeritonitisIJAR JOURNALNo ratings yet
- Blood Surveillance and Detection On Platelet Bacterial Contamination Associated With Septic Events.Document7 pagesBlood Surveillance and Detection On Platelet Bacterial Contamination Associated With Septic Events.Pritha BhuwapaksophonNo ratings yet
- Evaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationDocument9 pagesEvaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationbalkisNo ratings yet
- Diagnostics 12 00068Document9 pagesDiagnostics 12 00068Nyuori CosmasNo ratings yet
- Rapid ESR Test Using Inclined TubeDocument5 pagesRapid ESR Test Using Inclined TubeIshwar ChandraNo ratings yet
- Plateletcrit, Mean Platelet Volume, Platelet Distribution Width: Its Expected Values and Correlation With Parallel Red Blood Cell ParametersDocument4 pagesPlateletcrit, Mean Platelet Volume, Platelet Distribution Width: Its Expected Values and Correlation With Parallel Red Blood Cell ParametersSoumik SahaNo ratings yet
- Evaluation of The Abbott CELL-DYN 4000 HematologyDocument10 pagesEvaluation of The Abbott CELL-DYN 4000 Hematologypasamuco473No ratings yet
- RetikulositDocument4 pagesRetikulositFajar Tea JieNo ratings yet
- Lembar Jawaban SoalDocument5 pagesLembar Jawaban SoalWahyuNo ratings yet
- Quick guide to Laboratory Medicine: a student's overviewFrom EverandQuick guide to Laboratory Medicine: a student's overviewNo ratings yet
- Rheinfelden 28th February/3rd March 1638!: Protestant Brief 1Document1 pageRheinfelden 28th February/3rd March 1638!: Protestant Brief 1davdavdavdavdavdavdaNo ratings yet
- Cd4's and IL-10Document12 pagesCd4's and IL-10davdavdavdavdavdavdaNo ratings yet
- Evolution of Flow Cytometry As A Drug Screening PlatformDocument3 pagesEvolution of Flow Cytometry As A Drug Screening PlatformdavdavdavdavdavdavdaNo ratings yet
- Iphone 6s Manual User GuideDocument196 pagesIphone 6s Manual User GuideSamuel ShepherdNo ratings yet
- GneisenauDocument4 pagesGneisenaudavdavdavdavdavdavdaNo ratings yet
- TAL Enemy BattalionDocument2 pagesTAL Enemy BattaliondavdavdavdavdavdavdaNo ratings yet
- Rheinfelden 28th February/3rd March 1638!: Imperialist Brief 1Document1 pageRheinfelden 28th February/3rd March 1638!: Imperialist Brief 1davdavdavdavdavdavdaNo ratings yet
- GustavPlayBook PDFDocument48 pagesGustavPlayBook PDFdavdavdavdavdavdavdaNo ratings yet
- John Guest Speedfit Catalog Auguet 2014 EN PDFDocument48 pagesJohn Guest Speedfit Catalog Auguet 2014 EN PDFdavdavdavdavdavdavdaNo ratings yet
- BLK Qtrly Commentary 2015 q3 AmersDocument14 pagesBLK Qtrly Commentary 2015 q3 AmersdavdavdavdavdavdavdaNo ratings yet
- Sfo PlaybookDocument40 pagesSfo PlaybookdavdavdavdavdavdavdaNo ratings yet
- Indg 330Document3 pagesIndg 330davdavdavdavdavdavdaNo ratings yet
- GustavPlayBook PDFDocument48 pagesGustavPlayBook PDFdavdavdavdavdavdavdaNo ratings yet
- SiA Playbook FINAL-1Document56 pagesSiA Playbook FINAL-1davdavdavdavdavdavdaNo ratings yet
- Intracellular signaling pathwaysDocument2 pagesIntracellular signaling pathwaysdavdavdavdavdavdavdaNo ratings yet
- Ni 2987Document11 pagesNi 2987davdavdavdavdavdavdaNo ratings yet
- Piis2213858713701657 2Document14 pagesPiis2213858713701657 2davdavdavdavdavdavdaNo ratings yet
- MHC Class I and Class I-like gene expression in malignant T cellsDocument5 pagesMHC Class I and Class I-like gene expression in malignant T cellsdavdavdavdavdavdavdaNo ratings yet
- NM 3670Document6 pagesNM 3670davdavdavdavdavdavdaNo ratings yet
- Shipping Guide IX Final 2009Document28 pagesShipping Guide IX Final 2009davdavdavdavdavdavdaNo ratings yet
- Embj 201386030 FullDocument17 pagesEmbj 201386030 FulldavdavdavdavdavdavdaNo ratings yet
- Expression of A-Defensin 1-3 in T CellsDocument8 pagesExpression of A-Defensin 1-3 in T CellsdavdavdavdavdavdavdaNo ratings yet
- Leflunomide & AdenosineDocument10 pagesLeflunomide & AdenosinedavdavdavdavdavdavdaNo ratings yet
- Ni 2499Document11 pagesNi 2499davdavdavdavdavdavdaNo ratings yet
- 00 - All OOBs (Orders of Battle) in One DocumentDocument244 pages00 - All OOBs (Orders of Battle) in One Documentairfix199975% (4)
- French Clothing in The TYWDocument14 pagesFrench Clothing in The TYWdavdavdavdavdavdavda100% (1)
- Bassoe PaperDocument9 pagesBassoe PaperdavdavdavdavdavdavdaNo ratings yet
- Infect. Immun. 2014 Winter IAI.01443 13Document36 pagesInfect. Immun. 2014 Winter IAI.01443 13davdavdavdavdavdavdaNo ratings yet
- JC SupplementalDocument5 pagesJC SupplementaldavdavdavdavdavdavdaNo ratings yet
- Science 2013 Millien 792 6Document6 pagesScience 2013 Millien 792 6davdavdavdavdavdavdaNo ratings yet
- T-TEST GUIDE: WHEN & HOW TO APPLY POPULATION MEAN HYPOTHESIS TESTSDocument30 pagesT-TEST GUIDE: WHEN & HOW TO APPLY POPULATION MEAN HYPOTHESIS TESTSmichelleNo ratings yet
- Taich YamaguchiDocument8 pagesTaich Yamaguchidaniela cubillos escobarNo ratings yet
- MCQ Analysis of Variance, ANOVA, Anova, Qtt501, Lpu-Noteshanger, LPU, Galgotias, AmityDocument10 pagesMCQ Analysis of Variance, ANOVA, Anova, Qtt501, Lpu-Noteshanger, LPU, Galgotias, Amityjayant bansalNo ratings yet
- Output Uji T DMC - DM: Group StatisticsDocument4 pagesOutput Uji T DMC - DM: Group Statisticssmk kp3No ratings yet
- Effects of Teachers Effectiveness On Students Academic Performance in Public Secondary Schools Delta State NigeriaDocument8 pagesEffects of Teachers Effectiveness On Students Academic Performance in Public Secondary Schools Delta State NigeriaRCNo ratings yet
- A Comparative Study of Bombay Stock Exchange (BSE) and National Stock Exchange (NSE)Document6 pagesA Comparative Study of Bombay Stock Exchange (BSE) and National Stock Exchange (NSE)Nitesh TripathyNo ratings yet
- 90 Tesfaye AlemayehuDocument8 pages90 Tesfaye AlemayehuchuchuNo ratings yet
- North South University: School of Business Marketing Research (Mkt470)Document41 pagesNorth South University: School of Business Marketing Research (Mkt470)Sadman Shabab RatulNo ratings yet
- Thesis LengkapDocument55 pagesThesis LengkapIndraDimasNo ratings yet
- The Implementation of Cooperative Script Technique in Teaching Reading Comprehension To The Students of Senior High SchoolDocument12 pagesThe Implementation of Cooperative Script Technique in Teaching Reading Comprehension To The Students of Senior High SchoolAzida KhairaniNo ratings yet
- CGL Main Constituents Hazelnut OilDocument10 pagesCGL Main Constituents Hazelnut OilveromendoNo ratings yet
- Module 3A0 Tests For A Population MeanDocument52 pagesModule 3A0 Tests For A Population MeanShaun LeeNo ratings yet
- Testimonial Theatre-Making: Establishing or Dissociating The SelfDocument9 pagesTestimonial Theatre-Making: Establishing or Dissociating The SelfLucretia DespinoiuNo ratings yet
- F - TestDocument9 pagesF - TestsalhotraonlineNo ratings yet
- Midterm Exam T Test Paired 13Document2 pagesMidterm Exam T Test Paired 13Arly Kurt TorresNo ratings yet
- Journal of Primary Education: Sinta Kurnia Dewi, Sri Maryati Deliana & HaryadiDocument8 pagesJournal of Primary Education: Sinta Kurnia Dewi, Sri Maryati Deliana & HaryadiLaily SyuhadaNo ratings yet
- Lecture11 - REVISION - FINAL EXAMDocument21 pagesLecture11 - REVISION - FINAL EXAMHiền NguyễnNo ratings yet
- DATT Group Project - REGDocument19 pagesDATT Group Project - REGrao saadNo ratings yet
- ComputerDocument17 pagesComputerAyeshaNo ratings yet
- AR Benjie Manila 2017Document76 pagesAR Benjie Manila 2017Benjie Modelo ManilaNo ratings yet
- Melli Eliza (Kel - 10)Document18 pagesMelli Eliza (Kel - 10)RizkyNo ratings yet
- MBR Lab Week 10-12-1Document65 pagesMBR Lab Week 10-12-1Sadaqat AliNo ratings yet
- MODULE 27 Two Sample T-Tests When Variances Unequal 19 July 05Document15 pagesMODULE 27 Two Sample T-Tests When Variances Unequal 19 July 05jainaastha28_1951858No ratings yet
- One and Two Sample T Tests ExplainedDocument49 pagesOne and Two Sample T Tests ExplainedDigi MatesNo ratings yet
- Experimental Design With Sample TableDocument17 pagesExperimental Design With Sample TableAustinSalvadorNo ratings yet
- Digital Literacy Research MethodologyDocument15 pagesDigital Literacy Research Methodologynesha krishaNo ratings yet
- Tawa-Tawa Soap As AntifungalDocument14 pagesTawa-Tawa Soap As AntifungalCharlene BuendiaNo ratings yet
- Social Science MS - 2017Document56 pagesSocial Science MS - 2017dashrathrai17No ratings yet
- Glyn Davis, Branko Pecar - Statistics For Business Students - A Guide To Using Excel & IBM SPSS Statistics-Glyn Davis, Branko Pecar (2021)Document757 pagesGlyn Davis, Branko Pecar - Statistics For Business Students - A Guide To Using Excel & IBM SPSS Statistics-Glyn Davis, Branko Pecar (2021)navigaree100% (1)