Professional Documents
Culture Documents
Big Data Meets The Electronic Medical Record
Uploaded by
Warren Smith QC (Quantum Cryptanalyst)Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Big Data Meets The Electronic Medical Record
Uploaded by
Warren Smith QC (Quantum Cryptanalyst)Copyright:
Available Formats
SPECIAL EDITORIAL
Big Data Meets the Electronic Medical Record
A Commentary on Identifying Patients at Increased Risk for Unplanned Readmission
Greg de Lissovoy, PhD, MPH
hen should a patient be discharged from an inpatient hospital stay? The quick answer might be, only after the course of treatment is complete and further diagnosis, treatment, or monitoring is not required. However, that approach suggests an extended length of stay, whereas other considerations might argue for a more accelerated approach to discharge. For example, the patient may be eager to return home to family or friends willing and able to provide continuing care. The hospital can be a dangerous place; prolonged admission exposes the patient to risks of hospital-acquired infection or other misadventure.1 When continuing treatment is required, care in a less costly setting such as an outpatient clinic or skilled nursing facility may be feasible. Third-party insurance coverage such as Medicare that pays a set amount per admission gives the hospital a nancial incentive to shorten length of stay. In short, the decision to discharge may represent a delicate balance of competing objectives. Florence Rothman, age 87, was admitted to Sarasota Memorial Hospital in early 2003 with a diagnosis of aortic stenosis and underwent a routine valve replacement procedure. After an unremarkable course of treatment she was discharged in apparent good health. Four days later she collapsed and was taken to the emergency department where she died as a result of complications of surgery.2,3 Stunned by this unexpected turn of events, her sons Michael Rothman and Steven Rothman met with medical staff and hospital ofcials in an effort to understand how their mothers precarious condition could have escaped notice at the time of discharge. They were surprised to learn that the hospitals sophisticated electronic medical records (EMRs) system, while amassing substantial quantities of data over the course of an admission, generated no summary indicators of a patients condition or red ags that could inform decisions about readiness for discharge. The Rothmans vowed to nd a way by which future patients might avoid their mothers fate (M. Rothman, personal written communication, June 18, 2013).3 Although neither of the brothers was trained in medicine or health services research, they were no strangers to massive electronic databases. Michael Rothman, who holds a PhD in chemistry, spent much of his career as a computer scientist at the IBM Watson Research Laboratory and then became chief information ofcer for a major bank. Later he founded a company specializing in large data system design and analytics. Steven Rothman is an electrical engineer who began his career at the MITRE Corporation, a contract research organization spun-off from Massachusetts Institute of Technology. While working on aerospace projects in Colorado and New Mexico he became interested in oil and gas exploration and created a company that applied sophisticated mathematics and data visualization to the analysis of seismic data.2,3 With active support from the hospital, the Rothmans put their expertise to work exploring the EMR data repository. Their vision was to create algorithms that would
From the Department of Health policy and management, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD. The author declares no conict of interest. Reprints: Greg de Lissovoy, PhD, MPH, Department of Health policy and management, Johns Hopkins Bloomberg School of Public Health, Hampton House Room 325, 624 North Broadway, Baltimore, MD 21205. E-mail: gdelisso@jhsph.edu. Copyright r 2013 by Lippincott Williams & Wilkins ISSN: 0025-7079/13/5109-0759
Medical Care
Volume 51, Number 9, September 2013
www.lww-medicalcare.com |
759
Special Editorial
Medical Care
Volume 51, Number 9, September 2013
utilize existing EMR data to track patient health status over time, and to present this information as simple and meaningful metrics, available to the clinician in near real time.3 Several years of effort culminated in the Rothman Index (RI), as described in this issue of Medical Care.4 Building a model that can predict risk for hospital readmission is not a novel concept. Most of the numerous existing models rely on administrative data generally available only after the patient has been discharged and are most useful for retrospective assessment of quality of care. Only a handful of published models utilize data accessible while the patient is hospitalized, when outputs are available to guide the course of treatment.5 That situation will likely change rapidly with the marriage of 2 emerging technologies, EMRs and data mining. The EMR makes extensive clinical and demographic data immediately available without the delay required to obtain administrative data such as diagnostic codes that are typically assigned after discharge. Data mining is a general term applied to a wide range of computationintensive methods for detecting meaningful patterns in very large databases containing disparate data.6 Development of the RI exemplies this approach. Developers of clinical risk prediction models face many challenges. EMRs contain an extensive array of data types ranging from laboratory values to free-form text from which model variables must be constructed. The quantity of data that can accumulate during even a brief hospital stay is substantial; meaningful information must be extracted from what amounts to background noise. Software development is hampered by a lack of standardization across commercial EMR systems.7 The predictive power of the RI and of other published risk of readmission models is modest at best and generally characterized by high sensitivity and low specicity.4,811 In a continuing effort to reduce rates of avoidable readmission, the Centers for Medicare and Medicaid Services recently issued more stringent requirements for discharge planning as a condition for hospital participation in the Medicare program.8 Health status and readmission risk measures generated through real-time analysis of EMR data could potentially improve planning for a patients transition from inpatient to the next stage of care. Developers and clinical end users must collaborate to learn how to integrate these new health status metrics with existing information on
patient clinical and social characteristics to improve quality of care both during the hospital stay and after discharge. Precision and utility of risk-assessment algorithms will likely improve as the EMR evolves. The process of model building itself can inform the design of more efcient and useful EMR systems. Data mining will help identify factors most closely associated with good and bad outcomes for specic conditions while also revealing essentially irrelevant information now recorded as a legacy of traditional paperbased medical records. Florence Rothman will be watching! REFERENCES
1. Hauck K, Zhao X. How dangerous is a day in the hospital? A model of adverse events and length of stay for medical inpatients. Med Care. 2011;49:10681075. 2. PeraHealth Corporation. Available at: http://www.perahealth.com/. Accessed June 23, 2013. 3. HIStalk Interview with Michael Rothman, October 25, 2010. Available at: http://histalk2.com/2010/10/25/histalk-interviews-michael-rothmanpresident-rothman-healthcare-corporation/. Accessed June 23, 2013. 4. Bradley EH, Yakusheva O, Horvitz LI, et al. Identifying patients at increased risk for unplanned readmission. Med Care. 2013;51: 761766. 5. Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306: 16881698. 6. Manyika J, Chui M, Brown B, et al. Big Data: The Next Frontier for Innovation, Competition, and Productivity. Washington: McKinsey Global Institute. Available at: http://www.mckinsey.com/insights/business_technology/big_data_the_next_frontier_for_innovation. Accessed July 19, 2013; 2011. 7. Cholleti S, Post A, Gao J, et al. Leveraging derived data elements in data analytic models for understanding and predicting hospital readmission. AMIA Annu Symp Proc. 2012. Available at: http://www.ncbi.nlm.nih. gov/pmc/articles/PMC3540449/. Accessed July 13, 2013. 8. Department of Health and Human Services, Centers for Medicare and Medicaid Services. Revision to State Operations Manual (SOM) Hospital Appendix A. Center for Clinical Standards and Quality/Survey and Certification Group. Available at: http://www.cms.gov/Medicare/ Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/ Downloads/Survey-and-Cert-Letter-13-32.pdf. Accessed July 17, 2013. 9. Hasan O, Meltzer D, Shaykevich SA, et al. Hospital readmission in general medicine patients. J Gen Int Med. 2009;25:211219. 10. Amarasingham R, Moore BJ, Tabak YP, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using Electronic Medical Record data. Med Care. 2010;48: 981988. 11. Donze J, Aujesky D, Williams D, et al. Potentially avoidable 30-day hospital readmissions in medical patients: derivation and validation of a prediction model. JAMA Intern Med. 2013;173:632638.
760 | www.lww-medicalcare.com
2013 Lippincott Williams & Wilkins
You might also like
- Pauli Matrices: Classi Cation and Joint Higher Rank Numerical RangeDocument17 pagesPauli Matrices: Classi Cation and Joint Higher Rank Numerical RangeWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Understanding The Effects of Leakage in Superconducting Quantum Error Detection CircuitsDocument8 pagesUnderstanding The Effects of Leakage in Superconducting Quantum Error Detection CircuitsWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- InTech-Cultural Robotics The Culture of Robotics and Robotics in CultureDocument10 pagesInTech-Cultural Robotics The Culture of Robotics and Robotics in CultureWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- 3D Simulation System of Guiding Mobile Robot Based On Open GL LibraryDocument4 pages3D Simulation System of Guiding Mobile Robot Based On Open GL LibraryWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Application of The Novint Falcon Haptic Device As An Actuator in Real-Time ControlDocument12 pagesApplication of The Novint Falcon Haptic Device As An Actuator in Real-Time ControlWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Word Serial Architecture of CORDICDocument3 pagesWord Serial Architecture of CORDICWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Robo Cup@SapienzaDocument8 pagesRobo Cup@SapienzaWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Low-Bandwidth Re Ex-Based Control For Lower Power Walking: 65 KM On A Single Battery ChargeDocument70 pagesLow-Bandwidth Re Ex-Based Control For Lower Power Walking: 65 KM On A Single Battery ChargeWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- An Evaluation of Potential Operating Systems For Autonomous Underwater VehiclesDocument37 pagesAn Evaluation of Potential Operating Systems For Autonomous Underwater VehiclesWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Vibration Analysis of Tapered BeamDocument51 pagesVibration Analysis of Tapered BeamWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- A Dynamic Approach To Foster Cognitive Computing Using The Laws of ThoughtDocument5 pagesA Dynamic Approach To Foster Cognitive Computing Using The Laws of ThoughtWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Configuration Space Analysis of Rigid MechanismsDocument11 pagesConfiguration Space Analysis of Rigid MechanismsWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Swarm Robotics: Collective Behavior Inspired by NatureDocument2 pagesSwarm Robotics: Collective Behavior Inspired by NatureWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Intelligent Fuzzy Logic Based Controller Scheme For A Mobile Robot NavigationDocument54 pagesIntelligent Fuzzy Logic Based Controller Scheme For A Mobile Robot NavigationWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Template Matching Approach For Face Recognition SystemDocument6 pagesTemplate Matching Approach For Face Recognition SystemWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Technical Basis of Digital CurrenciesDocument22 pagesTechnical Basis of Digital CurrenciesWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Virtual Control and Monitoring For A Neurovisual Therapeutic DeviceDocument5 pagesVirtual Control and Monitoring For A Neurovisual Therapeutic DeviceWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Swarm Robot Control For Human Services and Moving Rehabilitation by Sensor FusionDocument11 pagesSwarm Robot Control For Human Services and Moving Rehabilitation by Sensor FusionWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Primecoin: Cryptocurrency With Prime Number Proof-of-WorkDocument6 pagesPrimecoin: Cryptocurrency With Prime Number Proof-of-WorkWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Quaternion Based Parameterization of Orientation-FinalDocument25 pagesQuaternion Based Parameterization of Orientation-FinalWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- An Analysis of The Bitcoin Electronic Cash SystemDocument45 pagesAn Analysis of The Bitcoin Electronic Cash SystemWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Sensor Module For Mobile RobotDocument6 pagesSensor Module For Mobile RobotWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Anonymous Byzantine Consensus From Moderately-Hard Puzzles: A Model For BitcoinDocument8 pagesAnonymous Byzantine Consensus From Moderately-Hard Puzzles: A Model For BitcoinWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Cryptocurrencies, Network Effects, and Switching CostsDocument37 pagesCryptocurrencies, Network Effects, and Switching CostsWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Bitcoin: A Search-Theoretic ApproachDocument28 pagesBitcoin: A Search-Theoretic ApproachWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Bitcoin Primer PDFDocument48 pagesBitcoin Primer PDFAyam ZebossNo ratings yet
- Double-Spending Fast Payments in Bitcoin Due To Client Versions 0.8.1Document2 pagesDouble-Spending Fast Payments in Bitcoin Due To Client Versions 0.8.1Warren Smith QC (Quantum Cryptanalyst)No ratings yet
- Internet Protocol Adoption: Learning From BitcoinDocument4 pagesInternet Protocol Adoption: Learning From BitcoinWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Have A Snack, Pay With BitcoinsDocument5 pagesHave A Snack, Pay With BitcoinsWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- Proofs of SpaceDocument23 pagesProofs of SpaceWarren Smith QC (Quantum Cryptanalyst)No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Clean Versus Sterile Management of Chronic WoundsDocument3 pagesClean Versus Sterile Management of Chronic WoundsDon RicaforteNo ratings yet
- Branches of Medicine & Wards and Departements - EditkuDocument31 pagesBranches of Medicine & Wards and Departements - EditkuGigih Sanjaya PutraNo ratings yet
- JADWAL PELATIHAN IhcaDocument1 pageJADWAL PELATIHAN Ihcalilik ari prasetyoNo ratings yet
- Renal Cell CarcinomaDocument9 pagesRenal Cell CarcinomaSahirNo ratings yet
- List of Reference BooksDocument2 pagesList of Reference BooksShagorShagorNo ratings yet
- 12i3uasd Asdhgas D WawanDocument9 pages12i3uasd Asdhgas D Wawanwaluyo ningratNo ratings yet
- Order 704189 - PSC Requisition - Ulta Lab TestsDocument2 pagesOrder 704189 - PSC Requisition - Ulta Lab TestsAmerica PerfectoNo ratings yet
- Diploma in DiabetologyDocument8 pagesDiploma in Diabetologydawood260No ratings yet
- Cipp 2015 AbstractsDocument88 pagesCipp 2015 AbstractsBuyanaaRise100% (2)
- A Rare Case Report: Abdominal Muscle Myoclonic JerksDocument4 pagesA Rare Case Report: Abdominal Muscle Myoclonic JerksasclepiuspdfsNo ratings yet
- Learning Disability Eye Test LeafletDocument4 pagesLearning Disability Eye Test LeafletInclusionNorthNo ratings yet
- Patient Discharge SummaryDocument1 pagePatient Discharge SummaryampalNo ratings yet
- Differential Diagnosis of Liver NoduleDocument46 pagesDifferential Diagnosis of Liver NoduleJoydip SenNo ratings yet
- SilosDocument3 pagesSilosapi-548205221100% (1)
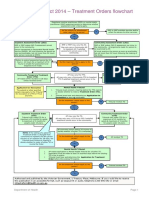
- Flowchart - Mental Health Act Treatment OrderDocument1 pageFlowchart - Mental Health Act Treatment OrderEdwin100% (1)
- HPA Axis Terkait Dengan Gangguan Jiwa (Dr. Hadi) .PPSXDocument19 pagesHPA Axis Terkait Dengan Gangguan Jiwa (Dr. Hadi) .PPSXMbak RockerNo ratings yet
- Endoscopy Neo InfantsDocument490 pagesEndoscopy Neo InfantsAlexandra NechiforNo ratings yet
- Bertino2022 Book ClinicalEthicsForConsultationPDocument181 pagesBertino2022 Book ClinicalEthicsForConsultationPJonatán Pérez RochaNo ratings yet
- Riza T. Calixtro: ObjectivesDocument2 pagesRiza T. Calixtro: ObjectivesLorinel MendozaNo ratings yet
- Experienced Pharmaceutical Sales LeaderDocument3 pagesExperienced Pharmaceutical Sales LeaderchadiresidencyNo ratings yet
- Indonesia Ophthalmologic Anesthesia Society (IOAS) : Susunan Acara Pertemuan Ilmiah Tahunan Ke - 4 16 - 17 Juli 2022Document4 pagesIndonesia Ophthalmologic Anesthesia Society (IOAS) : Susunan Acara Pertemuan Ilmiah Tahunan Ke - 4 16 - 17 Juli 2022ruthameliapNo ratings yet
- Angie ResumeDocument2 pagesAngie Resumeapi-270344093No ratings yet
- Critical Incident Reporting and Learning: Key PointsDocument7 pagesCritical Incident Reporting and Learning: Key PointsRavikiran SuryanarayanamurthyNo ratings yet
- Anemia in Pregnancy by MahreeDocument53 pagesAnemia in Pregnancy by MahreesherzadmahreeNo ratings yet
- Secrets of Pediaatric OrthopaedicsDocument610 pagesSecrets of Pediaatric OrthopaedicsPanagiotis Poulios100% (9)
- Biomedicines: Emerging Medical Treatments For Meningioma in The Molecular EraDocument21 pagesBiomedicines: Emerging Medical Treatments For Meningioma in The Molecular EraNorAmalinaNo ratings yet
- Toxoplasma Gondii.Document21 pagesToxoplasma Gondii.Sean MaguireNo ratings yet
- Diagnostic Imaging Pathways Article PDFDocument12 pagesDiagnostic Imaging Pathways Article PDFchald ald smithNo ratings yet
- Pictotrans: Pathology of The Breast Quiz From Dra. Edna May Lasap-GoDocument32 pagesPictotrans: Pathology of The Breast Quiz From Dra. Edna May Lasap-Go2012No ratings yet
- Burn AsseessmentDocument3 pagesBurn AsseessmentHCX dghhqNo ratings yet