Professional Documents
Culture Documents
Abdominal Infections
Uploaded by
Patrico Rillah SetiawanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abdominal Infections
Uploaded by
Patrico Rillah SetiawanCopyright:
Available Formats
Abdominal Infections
Biliary Tract Infections
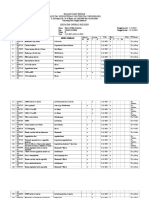
TREATMENT Community-acquired infections in patients without previous biliary procedures AND who are not severely ill Ceftriaxone 1 g IV q24h PLUS metronidazole 500 mg IV q8h OR Ertapenem 1 g IV q24h OR PCN allergy: ciprofloxacin 400 mg IV q12h PLUS metronidazole 500 mg IV q8h OR PO Regimen: amoxicillin/clavulanate 875 mg PO BID OR PO Regimen (PCN allergy): ciprofloxacin 500 mg PO BID PLUS metronidazole 500 mg PO q8h Hospital-acquired infections OR patients with prior biliary procedure OR patients who are severely ill Piperacillin/tazobactam 3.375 g IV q6h OR PCN allergy: ciprofloxacin 400 mg IV q12h PLUS metronidazole 500 mg IV q8h In severely ill patients with cholangitis or complicated cholelithiasis, adequate biliary drainage is crucial as antibiotics will not enter bile in the presence of obstruction. Duration Uncomplicated cholecystitis: treat only until obstruction is relieved. No post-procedure antibiotics are necessary if the obstruction is successfully relieved. Complicated cholecystitis: 5-10 days. Trend is now favoring shorter regimens. Biliary sepsis: 5-14 days. Shorter course favored if source controlled. Average duration is 7 days. TREATMENT NOTES Microbiology Gram-negative rods - E. coli, Klebsiella spp, Proteus spp, Pseudomonas (mainly in patients already on broad-spectrum antibiotics or those who have undergone prior procedures). Anaerobes - Bacteroides spp., generally in more serious infections, or in patients with a history of biliary manipulations. Enterococcus spp. - treatment not always indicated; use clinical judgment. Yeast - Rare, mainly in immunocompromised patients or those with extensive antibiotic history. Other considerations
CT scan is important in assessing need for drainage in severe disease. Some patients will present with diffuse peritonitis. Reference: IDSA Guidelines for Intra-Abdominal Infections: Clin Infect Dis 2003;37:997.
Pancreatitis
TREATMENT Mild to moderate pancreatitis - no antibiotics Severe acute pancreatitis (SAP)* - no prophylactic antibiotics No necrosis - no antibiotics Sterile pancreatic necrosis - no antibiotics Infected pancreatis necrosis* - empiric therapy: Meropenem 1 g IV q8h OR PCN allergy: ciprofloxacin 400 mg IV q12h PLUS metronidazole 500 mg IV q8h *Definitions Severe acute pancreatitis (SAP) is defined as pancreatitis associated with one or more of the following: >30% pancreatic necrosis APACHE II 9 More than 3 Ransons criteria Ransons criteria to predict severity of acute pancreatitis Zero Hours Age WBC Blood glucose Lactate dehydrogenase Aspartate aminotransferase (AST) >55 > 16,000/mm3 > 200 mg/dL > 350 U/L > 250 U/L
48 Hours Hematocrit Blood urea nitrogen (BUN) Serum calcium pO2 Fall by 10% Increase by 5 mg/dL despite fluids < 8 mg/dL < 60 mmHg
Base deficit Fluid sequestration
> 4 MEq/L > 6000 mL
Infected pancreatic necrosis is defined as one or both of the following: CT scan with gas Percutaneous aspirate or surgical specimen with organisms evident on Gram stain or culture
Duration For infected pancreatic necrosis, continue antibiotics for 14 days after source control is obtained. Continuation of antibiotics beyond this time places the patient at risk for colonization or infection with resistant organisms and drug toxicity. Antibiotics do not need to be continued until radiographic abnormalities have resolved. TREATMENT NOTES Penicillins and cephalosporins penetrate poorly into the pancreas Infection develops in 30-50% of patients with necrosis documented by CT scan or at the time of surgery. Peak incidence of infection occurs in the 3rd week of disease. Prophylactic antibiotics have been associated with a change in the spectrum of pancreatic isolates from enteric Gram-negatives to Gram-positive organisms and fungi. There is insufficient evidence to recommend selective gut decontamination in management of pancreatitis. References Lack of utility of prophylactic antibiotics: Ann Surg 2007;245:674. Guidelines for management of SAP: Crit Care Med 2004;32:2524. Ransons criteria: Surg Gyneecol Obstet 1974;139:69.
Peritonitis
DEFINITIONS Primary peritonitis is spontaneous infection of the peritoneal cavity, usually associated with liver disease and ascites [spontaneous bacterial peritonitis (SBP)]. Secondary peritonitis is infection of the peritoneal cavity due to spillage of organisms into the peritoneum, usually associated with GI or genitourinary tract (e.g., due to perforation, trauma, pelvic inflammatory disease). Tertiary peritonitis is a recurrent infection of the peritoneal cavity following an episode of secondary peritonitis.
Primary Peritonitis/Spontaneous Bacterial Peritonitis (SBP)
TREATMENT Ceftriaxone 1 g IV q24h is preferred. Amoxicillin/clavulanic acid 875 mg PO BID is the preferred oral regimen. Ciprofloxacin 400 mg IV/500 mg PO q12h can by used in PCN-allergic patients who have NOT been taking fluoroquinolones for SBP prophylaxis. Duration Treat for 5 days.
PROPHYLAXIS Cirrhotic patients with gastrointestinal hemorrhage Norfloxacin 400 mg PO BID for 7 days Ceftriaxone 1 g IV q24h can be used only if patient is NPO, then switch to norfloxacin 400 mg PO BID once bleeding is controlled. Non-bleeding cirrhotic patients with ascites Norfloxacin 400 mg PO daily OR TMP/SMX 1 DS PO daily TREATMENT NOTES Microbiology Gram-negative rods (Enterobacteriaceae, esp E. coli and K. pneumoniae), S. pneumoniae, enterococci, and other streptococci. Polymicrobial infections should raise concern for GI perforation. Diagnostic criteria 250 PMN per mm3 of ascitic fluid. Positive culture with < 250 PMN should prompt repeat tap. If PMN < 250 OR culture remains positive, patient should be treated. Follow-up Consider repeat paracentesis after 48 hours of therapy. Consider changing antibiotics if ascites fluid PMN has not dropped by 25% after 48 hours and/or patient is not clinically responding. Notes on prophylaxis against SBP All patients with cirrhosis and upper GI bleeding should receive prophylaxis for 7 days (50% develop SBP after bleed). Patients who get SBP should get lifelong prophylaxis to prevent future episodes (40-70% risk of recurrence in 1 year). Prophylaxis should be considered for those with low protein concentrations in ascites (< 10 g/L) or immunosuppression but must be carefully weighed against the risk of resistance. References: Diagnosis, treatment, and prophylaxis of SBP: J Hepatol 2000;32:142. Management of variceal hemorrhage in cirrhosis: Hepatology 2007;46:922-38.
Secondary Peritonitis/GI Perforation
TREATMENT Perforation of esophagus, stomach, small bowel, colon, or appendix Patient mild to moderately ill Ceftriaxone 1 g IV q24h PLUS metronidazole 500 mg IV q8h OR Ertapenem 1 g IV q24h OR PCN allergy: ciprofloxacin 400 mg IV q12h PLUS metronidazole 500 mg IV q8h
Patient severely ill or immunosuppressed Piperacillin/tazobactam 3.375 g IV q6h OR PCN allergy: ciprofloxacin 400 mg IV q12h PLUS metronidazole 500 mg IV q8h Antifungal Therapy Empiric antifungal therapy is generally NOT indicated for GI perforation unless patient has one of the following risk factors: Esophageal perforation, immunosuppression, prolonged antacid therapy, prolonged antibiotic therapy, prolonged hospitalization, persistent GI leak. For patients who are clinically stable and have not received prior long-term azole therapy: Fluconazole 400-800 mg IV/PO q24h For patients who are NOT clinically stable or have received prior long-term azole therapy: Caspofungin 75 mg IV x 1, then 50 mg IV q24h Duration of therapy for secondary peritonitis/GI perforation Stomach Uncomplicated Definition Duration Complicated Definition Duration Late operation or no operation 5-7 days, may require longer course Late operation or no operation 5-7 days, may require longer course Late operation or no operation 5-7 days, may require longer course Necrotic/gangrenous appendix 5-7 days, may require longer course Operated on within 24 hours 24-48 hours Operated on within 12 hours 24-48 hours Operated on within 12 hours 24-48 hours Non-necrotic or gangrenous appendix 24 hours Small Bowel Colon Appendix
TREATMENT NOTES Microbiology Causative agents for small bowel, colon, appendix: anaerobes (esp B. fragilis), Enterobacteriaceae (esp E. coli, K. pneumoniae, Enterobacter spp, Proteus spp); infections are usually polymicrobial. Pathogens causing tertiary peritonitis are variable and are often resistant to or not covered by the initial antimicrobial regimen; thus, a change in antimicrobials is advised. Diagnosis Prompt abdominal and pelvic CT scan is optimal for identification of source and defintiion of treatment; possible surgical options.
Treatment A change in antimicrobial therapy should be considered in patients with hospitalacquired infections who are already on antimicrobials. Treatment of enterococci remains controversial but may be of benefit in critically ill patients. Treatment of Candida spp is generally indicated only when they are recovered from blood or are the primary organism in the peritoneal culture. Postoperative antibiotics for appendicitis are unnecessary unless there is clinical evidence of peritonitis, abscess, or gangrene. Duration of therapy must be customized to the individual patient. Surgery and Infectious Diseases consultation should be considered. Surgery Antibiotics are adjunctive to source control, which is an absolute necessity. This may be accomplished with surgical debridement or percutaneous catheter drainage, depending on the clinical circumstances. Surgery consultation is strongly encouraged. The goal of source control is to evacuate devitalized or avascular infected material, define microbiology, and assist with determining the duration of antimicrobial therapy. Lack of source control is defined as ongoing contamination and/or an undrained collection of infection. Uncomplicated diverticulitis can usually be managed with antibiotics alone, although up to one-third of patients will have another episode. Surgery is generally advised after a first attack of complicated diverticulitis or after 2 or more attacks of uncomplicated diverticulitis. Non-operative management of perforated phlegmonous appendicitis when there is no abscess cavity to drain may be an option; Surgery input is critical.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Maju Ilmiah DigestifDocument85 pagesMaju Ilmiah DigestifPatrico Rillah SetiawanNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Advanced SCC Upper and Lower LipDocument7 pagesAdvanced SCC Upper and Lower LipPatrico Rillah SetiawanNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Employee Application Form - Actual SynergyDocument2 pagesEmployee Application Form - Actual SynergyPatrico Rillah SetiawanNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Idsa 2010Document32 pagesIdsa 2010Monica S. SuarezNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Treatment of Squamous Cell Carcinoma of The LipDocument4 pagesTreatment of Squamous Cell Carcinoma of The LipPatrico Rillah SetiawanNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Adenosquamous Carcinoma in Buccal Mucosa-A Case: KeywordsDocument3 pagesAdenosquamous Carcinoma in Buccal Mucosa-A Case: KeywordsPatrico Rillah SetiawanNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Spinal Cord InjuryDocument97 pagesSpinal Cord Injuryamoon1275% (4)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Pasien Digest Him - 6 Nov 18Document2 pagesPasien Digest Him - 6 Nov 18Patrico Rillah SetiawanNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Surgery of Choice in Patients With Recurrent ASBODocument29 pagesSurgery of Choice in Patients With Recurrent ASBOPatrico Rillah SetiawanNo ratings yet
- Wounds & Ulcers: Dr. Ranjeet PatilDocument40 pagesWounds & Ulcers: Dr. Ranjeet PatilPatrico Rillah SetiawanNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Abdominal Wall DefectsDocument16 pagesAbdominal Wall DefectsDesta FransiscaNo ratings yet
- Rev1 - 1661 3289 1 SMDocument6 pagesRev1 - 1661 3289 1 SMPatrico Rillah SetiawanNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Spinal Cord InjuryDocument97 pagesSpinal Cord Injuryamoon1275% (4)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Symptom Management Guidelines: Care of Malignant WoundsDocument7 pagesSymptom Management Guidelines: Care of Malignant WoundsPatrico Rillah Setiawan100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Symptom Management Guidelines: Care of Malignant WoundsDocument7 pagesSymptom Management Guidelines: Care of Malignant WoundsPatrico Rillah Setiawan100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Torsio Testis2016Document6 pagesTorsio Testis2016Patrico Rillah SetiawanNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Log Booc PWTDocument12 pagesLog Booc PWTPatrico Rillah SetiawanNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Perianalabscessfistulainano 170831035922Document47 pagesPerianalabscessfistulainano 170831035922Patrico Rillah SetiawanNo ratings yet
- Abstrak Rico FinalDocument1 pageAbstrak Rico FinalPatrico Rillah SetiawanNo ratings yet
- Kocher Manoeuvre Is A Surgical Manoeuvre To Expose Structures in The Retroperitoneum Behind The Duodenum and PancreasDocument1 pageKocher Manoeuvre Is A Surgical Manoeuvre To Expose Structures in The Retroperitoneum Behind The Duodenum and PancreasPatrico Rillah SetiawanNo ratings yet
- Pasienigd Bedah Selasa, 3 Januari 2017 Dokter: RAY/NTP/RIF/OLE/MAD/KP/RKYDocument2 pagesPasienigd Bedah Selasa, 3 Januari 2017 Dokter: RAY/NTP/RIF/OLE/MAD/KP/RKYPatrico Rillah SetiawanNo ratings yet
- Design BajuDocument2 pagesDesign BajuPatrico Rillah SetiawanNo ratings yet
- Pasienigd Bedah Selasa, 3 Januari 2017 Dokter: RAY/NTP/RIF/OLE/MAD/KP/RKYDocument2 pagesPasienigd Bedah Selasa, 3 Januari 2017 Dokter: RAY/NTP/RIF/OLE/MAD/KP/RKYPatrico Rillah SetiawanNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Neuro Surgery Department October 2015Document46 pagesNeuro Surgery Department October 2015Patrico Rillah SetiawanNo ratings yet
- Ankle Injury Orto ICO 2Document76 pagesAnkle Injury Orto ICO 2Patrico Rillah SetiawanNo ratings yet
- Gem Cisp UrolDocument5 pagesGem Cisp UrolPatrico Rillah SetiawanNo ratings yet
- Abstrak Rico FinalDocument1 pageAbstrak Rico FinalPatrico Rillah SetiawanNo ratings yet
- Daftar Pasien ICO Onko 2Document1 pageDaftar Pasien ICO Onko 2Patrico Rillah SetiawanNo ratings yet
- Log Book PurwokertoDocument11 pagesLog Book PurwokertoPatrico Rillah SetiawanNo ratings yet
- Triple-Negative Breast Cancer - Future inDocument7 pagesTriple-Negative Breast Cancer - Future inPatrico Rillah SetiawanNo ratings yet
- Cytopathic Agents from Measles Cases IsolatedDocument10 pagesCytopathic Agents from Measles Cases IsolatedRoger TNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Fallacy of Vaccination 1899Document24 pagesFallacy of Vaccination 1899rr100% (4)
- Public Health Pst.Document4 pagesPublic Health Pst.olaide samuelNo ratings yet
- Salmonella on Dairy FarmsDocument71 pagesSalmonella on Dairy Farmsthanh ba matNo ratings yet
- Essential Antibiotic Guide for Medical StudentsDocument74 pagesEssential Antibiotic Guide for Medical StudentskaelenNo ratings yet
- KalmeghDocument15 pagesKalmeghNaveen.M.NNo ratings yet
- Worksheet-3 17/06/2021: Microorganisms: Friend and Foe Class 8 Mcqs Questions With AnswersDocument6 pagesWorksheet-3 17/06/2021: Microorganisms: Friend and Foe Class 8 Mcqs Questions With Answersstory manNo ratings yet
- IELTS Lesson 9 Passage 1 Reading PracticeDocument16 pagesIELTS Lesson 9 Passage 1 Reading PracticeBảo ThúiNo ratings yet
- NACP V Strategy BookletDocument68 pagesNACP V Strategy BookletVaibhav KanaujiyaNo ratings yet
- Public Health Course ContentDocument2 pagesPublic Health Course ContentTabe EvelynNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Bacteriophage Report MB2006Document6 pagesBacteriophage Report MB2006jeanoriordan02No ratings yet
- Quiz No. 1 Acellular and Prokaryotic MicrobesDocument6 pagesQuiz No. 1 Acellular and Prokaryotic Microbesmaglangitjoannamarie1920No ratings yet
- Abreviaciones ChatDocument4 pagesAbreviaciones ChatrojarodNo ratings yet
- Gambaran OtomikosisDocument4 pagesGambaran OtomikosisMariany Melati100% (1)
- PTS 60.1501.08 HSE Food Water SafetyDocument55 pagesPTS 60.1501.08 HSE Food Water SafetyAmeerHamzaNo ratings yet
- Paramyxovirus Vs ParatyphoidDocument2 pagesParamyxovirus Vs ParatyphoidRaza AliNo ratings yet
- Microbial Contamination of Pharmaceutical Products and Microbial Attacks 24193Document9 pagesMicrobial Contamination of Pharmaceutical Products and Microbial Attacks 24193Labiba TasnimNo ratings yet
- Zaire,: Ebola Haemorrhagic Fever in 1976Document23 pagesZaire,: Ebola Haemorrhagic Fever in 1976bluemleinNo ratings yet
- Fascia of Upper LimbDocument45 pagesFascia of Upper LimbZaineb FarooqNo ratings yet
- HTTP DX Doi Org 10 1017 S0950268814002076Document4 pagesHTTP DX Doi Org 10 1017 S0950268814002076Alvaro SDNNo ratings yet
- Guidelines in BedmakingDocument9 pagesGuidelines in Bedmakinglex aspira100% (1)
- HBV IU Copy ConvertDocument11 pagesHBV IU Copy ConvertZulkifli AsNo ratings yet
- Health Action: in The Federal Republic of YugoslaviaDocument8 pagesHealth Action: in The Federal Republic of YugoslaviaСињор КнежевићNo ratings yet
- Top 7 health threats prioritized from a community assessmentDocument12 pagesTop 7 health threats prioritized from a community assessmentRomelle Jane M. VelascoNo ratings yet
- Microbiology Product Catalog 2020 2021Document88 pagesMicrobiology Product Catalog 2020 2021scientific trainingNo ratings yet
- Zone of InhibitionDocument3 pagesZone of InhibitionSubrata BhadraNo ratings yet
- Feco-orally Transmitted DiseasesDocument133 pagesFeco-orally Transmitted DiseasesTekletsadikNo ratings yet
- Therapeutic Indication Ofelectrohomeopathic MedicinesDocument8 pagesTherapeutic Indication Ofelectrohomeopathic MedicinesMeghanath PandhikondaNo ratings yet
- ProstatitisDocument13 pagesProstatitisBlanca HernándezNo ratings yet
- BIOL3400 UnknownLabInstructions S2023Document5 pagesBIOL3400 UnknownLabInstructions S2023DuwishaNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)