Professional Documents
Culture Documents
Acute Respiratory Distress Syndrome: Clinical Review
Uploaded by
Vijeyachandhar DorairajOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Respiratory Distress Syndrome: Clinical Review
Uploaded by
Vijeyachandhar DorairajCopyright:
Available Formats
For the full versions of these articles see bmj.
com
CLINICAL REVIEW
Acute respiratory distress syndrome
Susannah K Leaver, Timothy W Evans
Department of Critical Care, Imperial College School of Medicine, Royal Brompton Hospital, London SW3 6NP Correspondence to: T W Evans t.evans@rbht.nhs.uk
BMJ 2007;335:389-94 doi:10.1136/bmj.39293.624699.AD
Why do I need to know about acute respiratory distress syndrome? Acute respiratory distress syndrome is the extreme manifestation of acute lung injury. Both these conditions complicate many medical and surgical conditions, not all of which affect the lung directly and are therefore encountered by clinicians working outside the critical care setting with varying frequency. Early recognition is important in determining outcome, as prognosis is usually dependent partly on the nature and prompt management of the precipitating condition. How are these conditions defined? Acute lung injury and acute respiratory distress syndrome are defined by refractory hypoxaemia (using the PaO2 to FiO2 ratio) in association with bilateral lung infiltrates on chest radiography, in the absence of left atrial hypertension (thereby excluding hydrostatic pulmonary oedema as a cause) but in the presence of a clinical condition known to precipitate the syndrome (box 1). Although the definition criteria outlined in box 1, developed in 1992,1 have facilitated the enrolment of patients with different underlying pathologies into large scale clinical trials, they are inadequate for several reasons. Firstly, they do not take into account the relevance of the precipitating condition to prognosis. Secondly, the most appropriate system of interpretation of chest radiographs is not defined. Thirdly, they fail to standardise the strategy of mechanical ventilatory support to be used when hypoxaemia is quantified. Consequently a further consensus conference was arranged in 2000, but no agreement concerning revised clinical definitions or criteria emerged. Indeed, the conference believed that the breadth and level of specificity of the existing definitions had enabled the easy recruitment of a large number of patients for inclusion in clinical trials of putative therapeutic interventions (personal communication). As all patients with acute respiratory distress syndrome fulfil the defining criteria for acute lung injury, we will use the latter term to refer to both conditions throughout this review, except where evidence cited is applicable only to patients with acute respiratory distress syndrome. How often is it encountered? The 1992 definition (box 1) for acute lung injury enabled the first estimations of incidence to be made, which range between 4.8 and 34 per 100 000 population a year, with substantial international variability.2 3 However, a recent
prospective study in a single county in the United States, including over 1000 patients and performed over 14 months found the incidence of acute lung injury to be higher (78.9 per 100 000 population), suggesting that some 190 600 cases occur in the US each year.4 The incidence of acute respiratory distress syndrome is influenced by the underlying clinical condition (table 1) being highest in patients with sepsis, severe sepsis, and septic shock and lower in patients with trauma.3 Other factors affecting incidence include advanced age and alcohol consumption.7 The extent to which the precipitating condition affects the lung directly or indirectly seems to influence lung compliance and recruitment (that is, opening up collapsed alveoli), appearances on computed tomography, and possibly clinical outcome.8 9
How is acute lung injury recognised? Patients present either with acute lung injury or full blown acute respiratory distress syndrome, which may have prognostic significance. Some 55% of patients with acute lung injury seem to develop acute respiratory distress syndrome within three days of admission to an intensive care unit.10 In practice, most patients present clinically with dyspnoea, which may be masked by symptoms attributable to the precipitating condition. Clinical signs are those of pulmonary oedema of varying severity. The differential diagnosis is therefore relatively limited (box 2). What is the pathophysiology of acute lung injury? Genetic susceptibility to the development of acute lung injury has been suggested through the demonstration in relevant populations of genetic polymorphisms in the expression of genes encoding specific pathophysiological pathways. Acute respiratory distress syndrome
SOURCES AND SELECTION CRITERIA We searched various sources to identify relevant evidence concerning the definition, epidemiology, and management and prognosis of patients with acute lung injury and acute respiratory distress syndrome. These included Medline, the Cochrane Library, conference proceedings, websites for specific clinical trials, and ClinicalTrials.gov (a website sponsored by the US National Institutes of Health that provided information about federally and privately supported clinical research in human volunteers)
BMJ | 25 AUGUST 2007 | VOLUME 335
389
CLINICAL REVIEW
Box 1 | Definition criteria for acute lung injury and acute respiratory distress syndrome1 In the appropriate clinical setting with one or more recognised risk factors, three criteria are required: RadiologicalNew, bilateral, diffuse, patchy, or homogeneous pulmonary infiltrates on chest radiograph consistent with pulmonary oedema ExclusionNo clinical evidence that heart failure, fluid overload, or chronic lung disease are responsible for the infiltrates; or pulmonary artery occlusion pressure of 18 mm Hg OxygenationPaO2:FiO2 ratio of <40 kPa (acute lung injury); PaO2:FiO2 ratio of <26 kPa (acute respiratory distress syndrome)
Fig 1 | Lung computed tomogram in a patient meeting the defining criteria for acute respiratory distress syndrome. The scan shows that acute respiratory distress syndrome does not affect the lung parenchyma homogeneously, with areas of dense opacification in dependent lung regions (arrow)
is characterised histopathologically by evidence of alveolar inflammation and injury leading to increased pulmonary capillary permeability. The syndrome is known to evolve through exudative, inflammatory, and fibroproliferative (or reparative) phases, usually over a total period of two to three weeks. The clinical consequences are impaired gas exchange with refractory hypoxaemia resulting from ventilation perfusion mismatch, physiological shunting, atelectasis of lung units, and reduced compliance, one of the hallmarks of acute respiratory distress syndrome. Rare complications are progressive pulmonary fibrosis and pulmonary hypertension, both of which have adverse prognostic significance.
What investigations should be performed? Investigations aim to diagnose acute lung injury and acute respiratory distress syndrome, define the extent of lung injury, and help to elucidate the precipitating condition (see table 2). Use of computed tomography of the thorax is increasing as it is more sensitive than plain chest radiography in identifying pulmonary causes of acute respiratory distress syndrome and detecting complications. Computed tomography has also shown that acute respiratory distress syndrome does not affect the lung parenchyma homogeneously (figs 1 and 2).
Table 1 | Acute respiratory distress syndrome: common precipitating conditions with effect on incidence and outcome*3 5 6
Condition Sepsis syndrome Pneumonia Extra pulmonary source Septic shock Pulmonary source Extra pulmonary source Trauma Blood transfusion (>8 units within 24 hours) Gastrointestinal aspiration Incidence of acute respiratory distress syndrome (%) 29 38 15 37 48 25 12-18 29 22-38 Mortality (%) 32 36 29 55 56 54 10 57 52
How should these patients be managed? Treatment of patients with acute lung injury is essentially supportive, coupled with aggressive management of the precipitating condition. Complications, which include the exacerbation of lung injury, multiple organ system failure, nosocomial pneumonia, deep vein thrombosis, and gastrointestinal bleeding must be minimised. Admission to an intensive care unit with experience in dealing with such cases is mandatory and may improve outcome.4 General supportive measures Nutrition The early provision of enteral nutrition (given in the semirecumbent position to reduce the risk of nosocomial pneumonia) is desirable in all critically ill patients. Although evidence is limited regarding the optimal composition, data show that there may be advantages in using feed containing eicopentaenoic acid, linolenic acid, and antioxidants. Several animal studies and one prospective, double blind, randomised controlled trial in 165 patients showed a significant reduction in mortality with such feed (absolute mortality reduction 19.4%, P=0.037).11 Fluid management The increased pulmonary vascular permeability that characterises acute lung injury suggests that fluid restriction should decrease alveolar lung oedema and improve ventilation. By contrast, reduced circulating volume decreases cardiac output and oxygen delivery and increases renal impairment. Evidence from a well constructed randomised trial in 1000 patients suggests that conservative fluid replacement is associated with significantly improved lung and central nervous system functions and a reduction in the number of days without ventilation and without the need for admission to an intensive care unit, with no increase in non-pulmonary
BMJ | 25 AUGUST 2007 | VOLUME 335
*Similar data are not available for acute lung injury. Defined as multiple fractures with or without pulmonary contusion.
390
CLINICAL REVIEW
organ dysfunction. However, the trial found no significant difference in 60 day mortality.12 Similarly, pulmonary artery catheterisation to guide fluid management has shown no mortality advantage over monitoring of central venous pressure.13 Fluid intake should therefore be guided by central venous pressure and restricted where possible while maintaining adequate peripheral perfusion.
Glycaemic control
Strict control of blood glucose (maintaining glucose concentration between 4.4 mmol/l and 6.1 mmol/l) affords a survival advantage to most critically ill patients, although no studies have been conducted exclusively in those with acute respiratory distress syndrome.14
Mechanical ventilation Lung protection
Fig 2 | CT one year later in same patient as in figure 1
Although some patients with acute lung injury can be managed using non-invasive ventilation, most require endotracheal intubation. The characteristic distribution of lung injury means that regions that are relatively unaffected receive a disproportionate volume of the delivered breath and are therefore at risk of overdistension (volutrauma), especially if the positive pressure is high, which can lead to barotrauma. Volutrauma and cyclical opening and closing of damaged lung (atelectrauma) are thought to generate proinflammatory mediators (biotrauma). A landmark multicentre, randomised trial was stopped after enrolling 861 patients, because it found that low tidal volume ventilation (6 ml/kg of predicted body weight) afforded a significant mortality advantage (P=0.007) when compared with a standard approach (such as 12 ml/kg).15 This lung protective technique can result in reduced clearance of carbon dioxide (CO2), although evidence is lacking to determine the level of consequent acidosis that is safe. In practice, permissive hypercapnia is an acceptable side effect as long as oxygenation is not compromised and the pH is maintained above 7.2.
A PATIENTS PERSPECTIVE I was 57 years old when my nightmare began on 5 July 2005. I had flu-like symptoms and breathing difficulties. I was taken to hospital with suspected pneumonia and three hours later was transferred to intensive care and put on a ventilator. My family was told I had legionnella and acute respiratory distress syndrome and had a 30% chance of survival. Four weeks later I was transferred to the Royal Brompton Hospital and after five days was given a tracheostomy. I couldnt speak and was so weak: I couldnt hold a pen, scratch my nose, or move my body. I went home on 21 September with a walking stick. What a shock! I was so weak. I was followed up at ICU outpatients at the Brompton and have been told that my lung function is now normal. I do have some numbness in my fingers and the front of my legs, but this doesnt stop me doing the things that I could do before my illness. I am a caretaker at a college and went back to work in December 2005, and life is wonderful again.
Positive end expiratory pressure The application of positive end expiratory pressure improves oxygenation by increasing functional residual capacity, recruiting small airways, and improving ventilation and perfusion mismatch by reducing intrapulmonary shunting of blood through collapsed alveoli. Minimising cyclical alveolar collapse and reopening positive end expiratory pressure may result in less ventilator associated lung injury, but high levels can cause circulatory depression and lung injury from overdistension of recruitable lung units. However, a randomised trial including 549 patients with acute lung injury or acute respiratory distress syndrome showed ventilating patients with lower (8.3 cm H2O) or higher (13.2 cm H2O) levels of positive end expiratory pressure does not influence mortality, ventilator-free days, days spent in intensive care or breathing without assistance, barotrauma, or days without organ failure.16 How the use of positive end expiratory pressure and recruitment manoeuvres (and the strategies for setting these) may be used as adjuncts to the protective ventilatory approaches outlined above has been the subject of two large scale, recently completed but unpublished randomised trials (www. abstracts2view.com/ats07/view.php?nu=ATS07L _2793&terms, www.abstracts2view.com/ats07/ view.php?nu=ATS07L_2979&terms). Until then it remains reasonable to set a positive end expiratory pressure level just above the lower inflection point on the static pressure-volume curve, to optimise alveolar recruitment while minimising shear stress. Prone ventilation Moving patients with acute respiratory distress syndrome into the prone position has consistently been shown to improve oxygenation initially in about 60% of cases, but not improve mortality.17 However, no large randomised controlled trials have been conducted, and in our opinion this difficult manoeuvre should be reserved for patients in whom adequate oxygenation cannot be achieved by lung protective mechanical ventilation alone (fig 3).
391
BMJ | 25 AUGUST 2007 | VOLUME 335
CLINICAL REVIEW
Box 2 | Acute lung injury: differential diagnoses Cardiogenic pulmonary oedema: excluded by using echocardiography Acute interstitial pneumonia: a rare rapidly progressing form of lung injury presenting in previously healthy individuals. Diagnosis is made clinically with pathological confirmation. Bronchoalveolar lavage characteristically shows both eosinophils and neutrophils Diffuse alveolar haemorrhage: consider when a patient with acute respiratory failure has an unexplained drop in haemoglobin concentration. If haemoptysis is not present, blood is usually seen at bronchoscopy (post-intubation). Haemosiderin laden macrophages appear after 48 hours and are diagnostic Idiopathic acute eosinophilic pneumonia: characterised by cough, dyspnoea, fever, and occasionally chest pain in previously healthy individuals. Raised eosinophils (typically 40%) are seen in the bronchoalveolar lavage fluid and usually in the blood. There is a rapid response (normally within 48 hours) to corticosteroids Malignancy, particularly lymphangitis carcinomatosis: this can mimic acute respiratory distress syndrome when it disseminates quickly throughout the lung. Bronchoscopy with bronchoalveolar lavage and biopsy help to differentiate between the two
Patient meets American-European Consensus Conference criteria for acute lung injury or acute respiratory distress syndrome1; precipitating condition resolved or stable Use protective ventilatory strategy to support15 Oxygenation satisfactory (SaO2>88%) No Consider prone positioning17 Oxygenation satisfactory (SaO2>88%) No Consider inhaled nitric oxide, nebulised prostacyclin19 20 Oxygenation satisfactory (SaO2>88%) No Under evaluation (2007): Consider extracorporeal gas exchange (www.cesar-trial.org) Unable to wean Yes Yes Yes Achieve stability for 72 hours with: Signs of improving minute volume requirement Signs of increasing compliance
Wean from ventilation in conventional way
Other ventilatory techniques Interest in high frequency ventilation or oscillationin which small tidal volumes (less than anatomical deadspace) are administered at very high frequencies and gas exchange occurs by convectionhas grown since the introduction of protective ventilatory strategies.18 Currently, no clear evidence indicates whether high frequency ventilation reduces mortality or long term morbidity in patients with acute lung injury or respiratory distress syndrome. Non-ventilatory adjuncts to gas exchange Inhaled nitric oxide Nitric oxide is an endogenous vasodilator. When administered by inhalation at concentrations up to 20 parts per million, it reduces pulmonary vascular resistance. Although about 60% of patients with acute lung injury have an initial noticeable improvement in oxygenation, the effect is transient (48 hours) and does not confer mortality benefit or reduction in the duration of mechanical ventilation.19 Authorities suggest that nitric oxide should not be used routinely but be reserved for patients in whom adequate oxygenation cannot be achieved by lung protective mechanical ventilation and prone positioning (fig 3).20 Nebulised prostacyclin Prostacyclin is a second endogenous vasodilator with similar physiological effects to nitric oxide. When
Table 2 | Investigations in patients with acute lung injury or acute respiratory distress syndrome
Test Chest radiography Arterial blood gases Echocardiography Computed tomography thorax (figs 1 and 2) Fibreoptic bronchoscopy with bronchoalveolar lavage How does it help? New, bilateral, diffuse, patchy, or homogeneous pulmonary infiltrates consistent with pulmonary oedema define both conditions Indicates severity of hypoxaemia, defining acute lung injury and acute respiratory distress syndrome Helps to differentiate acute lung injury from cardiogenic pulmonary oedema Aids identification of pulmonary causes of acute lung injury (such as pneumonia, lung abscess) and detection of complications such as pneumothoraces and pleural effusions Helps to exclude infection, particularly in patients who are not improving despite treatment
Re-evaluate precipitating condition, for infection bronchoalveolar lavage and consider computed tomography for collection, pneumothorax etc
Fig 3 | Our approach to the application of mechanical ventilatory support, non-ventilatory adjuncts to gas exchange, and pharmacotherapy in patients with acute lung injury and acute respiratory distress syndrome
nebulised, it has an equivalent effect on pulmonary vasodilation and oxygenation but is easier to administer, has harmless metabolites, and requires no special monitoring. However, no large randomised controlled trials in acute respiratory distress syndrome have been conducted.
Surfactant Although patients with acute respiratory distress syndrome have decreased and dysfunctional surfactant, no benefit has been found after the administration of both natural and synthetic formulationsin terms either of mortality or of the need for mechanical ventilation. By contrast, significant improvements in oxygenation have been found during the initial 24 hours of treatment.21 This treatment is not yet available outside clinical trials. Extracorporeal gas exchange The techniques involved in extracorporeal membrane oxygenation are numerous. No survival benefit has been seen among patients with acute respiratory distress syndrome in the sole randomised clinical trial of extracorporeal membrane oxygenation.22 However, the results of a study comparing transport to a centre that offers extracorporeal membrane oxygenation versus locally applied conventional ventilation in patients with acute respiratory failure are awaited (www.cesar-trial.org).
BMJ | 25 AUGUST 2007 | VOLUME 335
392
CLINICAL REVIEW
Pharmaceutical interventions Corticosteroids A well constructed, multicentre, double blind, randomised controlled trial in 180 patients focusing on the use of corticosteroids in late (fibroproliferative) acute respiratory distress syndrome has shown that methylprednisolone does not influence 60 day mortality.23 However, steroid recipients had an increased number of ventilator and shock-free days during the first 28 days (with improved respiratory compliance, oxygenation, and blood pressure) and fewer days of vasopressor therapy. The corticosteroid group had a higher rate of neuromuscular weakness, and those started on methylprednisolone more than 14 days after the onset of acute respiratory distress syndrome may have had an increased risk of death.23 The routine use of corticosteroids in patients with persistent acute respiratory distress syndrome is therefore currently not recommended. Although some clinicians have suggested that low doses may be efficacious in patients in septic shock and relative adrenal insufficiency, the preliminary results of a recently completed large scale trial have shown no survival or other advantage (clinicaltrials.gov/ct/show/NCT00147004). Other pharmacotherapies Several potential therapeutic interventions have been used in trials in acute respiratory distress syndrome. Those that have not been shown to confer survival benefit include a variety of antioxidants, -2 adrenergic receptor agonists, lisofylline, prostaglandin E1, pentoxifylline, interleukin 10, neutrophil elastase inhibitors, granulocyte macrophage colony stimulating factor, dazoxiben, indometacin, and aciclovir. A Cochrane review concluded that there was insufficient evidence to support the application of any specific pharmacotherapy.24 When is a patient ready to wean from mechanical ventilation? Although studies have not identified the optimal arterial oxygen tension in critical illness, saturations (SaO2) in excess of 88% are a reasonable target in individuals without other relevant disorders (such as cardiovascular insufficiency). A period during which ventilatory stability or improving compliance and minute
Box 3 | Problems encountered after survival from acute respiratory distress syndrome30 Reduced body weight Poor functional physical capacity Persistent pain at the site of chest drain insertion Entrapment neuropathies Heterotrophic ossification causing enlargement and immobility of large joints The cosmetic appearance of tracheostomy sites Fixed deformities of fingers or frozen shoulders Low quality of life score (below that of age and sex matched control) at one year
volume requirement are observed is desirable before weaning is started in the conventional manner (fig 3).
How many patients survive and what is their quality of life? The findings of a paper in 1985 found that most patients with acute lung injury who fail to survive seem to die from multiple organ system failure rather than from pulmonary insufficiency.25 More recently, clinical experimental evidence suggests that multiple organ system failure occurs partly through dissemination of inflammatory cytokines from the alveolar space into the pulmonary and systemic circulations, a phenomenon reduced by lung protection strategies of mechanical ventilation.26 In the Unites States alone, acute lung injury is associated with 74 500 deaths annually and the care of such patients consumes 3.6 million hospital days.4 Risk factors associated with a poor outcome include advanced age, sepsis, liver disease, and non-pulmonary organ dysfunction.27 28 In Europe, a prospective multinational study has reported crude mortality rates for intensive care units and hospitals of 22.6% and 32.7% respectively for acute lung injury and 49.4% and 57.9% respectively for acute respiratory distress syndrome.10 In a UK centre a significant reduction in mortality was seen from 66% to 34% during 1990-7.29 Persistent morbidity after discharge from intensive care is substantial. A well constructed prospective longitudinal study in 109 survivors of acute respiratory distress syndrome showed that three months after discharge from intensive care, patients had a mild to moderate restrictive pattern on lung function testing, with a mild to moderate reduction in carbon monoxide diffusion capacity. A better functional status was associated with the absence of systemic corticosteroid treatment and with illness acquired during a stay in intensive care, as well as with rapid resolution of lung injury and multi organ failure.30 See box 3 for an outline of problems encountered after survival from acute respiratory distress syndrome. Intensive care follow-up clinics are in their infancy. However, problems encountered by patients with acute lung injury and other critical illnesses suggest that these clinics, with multidisciplinary input from
393
UNANSWERED RESEARCH QUESTIONS AND ONGOING RESEARCH Trials completed but not yet formally reported UK study comparing transport of patients with severe acute respiratory failure to a centre providing extracorporeal support with conventional ventilation methods applied locally (www.cesar-trial.org) New registered trials of potential pharmacological interventions in patients with acute lung injury registered at Clinical Trials.gov New trial of safety and efficacy of a recombinant chimeric monoclonal antibody against CD14 (IC14) in hospitalised patients with acute lung injury (clinicaltrials.gov/ct/show/NCT00233207) Phase II clinical trial of activated protein C (Xigris) versus placebo for the treatment of acute lung injury (clinicaltrials.gov/ct/show/NCT00112164)
BMJ | 25 AUGUST 2007 | VOLUME 335
CLINICAL REVIEW
SUMMARY POINTS
Acute lung injury and its extreme manifestation, the acute respiratory distress syndrome, complicate a variety of serious medical and surgical conditions, not all of which affect the lung directly Dyspnoea is the commonest presenting symptom; clinical signs are those of pulmonary oedema Early admission to intensive care is needed; the precipitating illness should be identified and managed aggressively Protective techniques of mechanical ventilatory support reduce mortality Rigorous application of general supportive measures is likely to improve outcome Non-ventilatory adjuncts to gas exchange generally improve oxygenation but do not reduce mortality Although death rates are falling, long term debility in survivors is considerable
8
10
11
12
appropriate healthcare professionals, are likely to be necessary and helpful.
Contributors: Both authors contributed to the collection of data and to the text of the paper. TWE is the guarantor. Competing interests: None declared. Provenance and peer review: Commissioned and externally peer reviewed.
1 Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994;149:818-24. Goss CH, Brower RG, Hudson LD, Rubenfeld GD, ARDS Network. Incidence of acute lung injury in the United States. Crit Care Med 2003;31:1607-11. MacCallum NS, Evans TW. Epidemiology of acute lung injury. Curr Opin Crit Care 2005;11:43-9. Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, et al. Incidence and outcomes of acute lung injury. N Engl J Med 2005;353:1685-93. Gong MN, Thompson BT, Williams P, Pothier L, Boyce PD, Christiani DC. Clinical predictors of and mortality in acute respiratory distress syndrome: potential role of red cell transfusion. Crit Care Med 2005;33:1991-8. Fowler AA, Hamman RF, Zerbe GO, Benson KN, Hyers TM. Adult respiratory distress syndrome. Prognosis after onset. Am Rev Respir Dis 1985;132:472-8. Wind J, Versteegt J, Twisk J, van der Werf TS, Bindels AJ, Spijkstra JJ, et al. Epidemiology of acute lung injury and acute respiratory distress
13
14 15
16
17
3 4
18
19 20
21
22
ADDITIONAL EDUCATIONAL RESOURCES Resources for health professionals NHLBI Acute Respiratory Distress Syndrome Network (www.ardsnet.org)Large US based research group (sponsored by the National Institutes of Health) investigating new treatments for acute lung injury and acute respiratory distress syndrome Resources for patients UK Intensive Care Society (www.ics.ac.uk)Has information for patients and relatives, including two useful publications: Your Questions Answered and Critical InsightAn Intensive Care Society (ICS) Introduction to UK Adult Critical Care Services PatientUK (www.patient.co.uk)Website providing the same free, current health information and leaflets that are often provided by general practitioners to patients during consultations; has a section devoted to intensive care and critical care Royal College of Physicians (www.rcplondon.ac.uk) Website of the Royal College of Physicians of London, which has an active patient and carer forum with representation on the colleges Critical Care Committee
23
24
25
26
27
28
29
30
syndrome in the Netherlands: a survey. Respir Med 2007;6 Jul (Epub ahead of print) doi: 10.1016/j.rmed.2007.05.021 Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med 2006;354:1775-86. Suntharalingam G, Regan K, Keogh BF, Morgan CJ, Evans TW. Influence of direct and indirect etiology on acute outcome and 6-month functional recovery in acute respiratory distress syndrome. Crit Care Med 2001;29:562-6. Brun-Buisson C, Minelli C, Bertolini G, Brazzi L, Pimentel J, Lewandowski K, et al. Epidemiology and outcome of acute lung injury in European intensive care units. Results from the ALIVE study. Intensive Care Med 2004;30:51-61. Pontes-Arruda A, Aragao AM, Albuquerque JD. Effects of enteral feeding with eicosapentaenoic acid, gamma-linolenic acid, and antioxidants in mechanically ventilated patients with severe sepsis and septic shock. Crit Care Med 2006;34:2325-33. National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 2006;354:2564-75. National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med 2006;354:2213-24. Finney SJ, Zekveld C, Elia A, Evans TW. Glucose control and mortality in critically ill patients. JAMA 2003;290:2041-7. Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8. Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 2004;351:327-36. Mancebo J, Fernandez R, Blanch L, Rialp G, Gordo F, Ferrer M, et al. A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med 2006;173:1233-9. Wunsch H, Mapstone J. High-frequency ventilation versus conventional ventilation for treatment of acute lung injury and acute respiratory distress syndrome. Cochrane Database Syst Rev 2004; (1):CD004085. Griffiths MJ, Evans TW. Inhaled nitric oxide therapy in adults. N Engl J Med 2005;353:2683-95. Adhikari NK, Burns KE, Freidrich JO, Granton JT, Cook DJ, Meade MO. Effect of nitric oxide on oxygenation and mortality in acute lung injury: systematic review and meta analysis. BMJ 2007;334:779-82. Spragg RG, Lewis JF, Walmrath HD, Johannigman J, Bellingan G, Laterre PF, et al. Effect of recombinant surfactant protein C-based surfactant on the acute respiratory distress syndrome. N Engl J Med 2004;351:884-92. Morris AH, Wallace CJ, Menlove RL, Clemmer TP, Orme JF Jr, Weaver LK, et al. Randomized clinical trial of pressure-controlled inverse ratio ventilation and extracorporeal CO2 removal for adult respiratory distress syndrome. Am J Respir Crit Care Med 1994;149:295-305. National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med 2006;354:1671-84. Adhikari NK, Burns KE, Meade MO. Pharmacologic therapies for adults with acute lung injury and acute respiratory distress syndrome. Cochrane Database Syst Rev 2004;(4):CD004477. Montgomery AB, Stager MA, Carrico CJ, Hudson LD. Causes of mortality in patients with the adult respiratory distress syndrome. Am Rev Respir Dis 1985;132:485-9. Ranieri VM, Suter PM, Tortorella C, de Tullio R, Dayer JM, Brienza A, et al. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA 1999;282:54-61. Ely EW, Wheeler AP, Thompson BT, Ancukiewicz M, Steinberg KP, Bernard GR. Recovery rate and prognosis in older persons who develop acute lung injury and the acute respiratory distress syndrome. Ann Intern Med 2002;136:25-36. Doyle RL, Szaflarski N, Modin GW, Wiener-Kronish JP, Matthay MA. Identification of patients with acute lung injury. Predictors of mortality. Am J Respir Crit Care Med 1995;152:1818-24. Abel SJ, Finney SJ, Brett SJ, Keogh BF, Morgan CJ, Evans TW. Reduced mortality in association with the acute respiratory distress syndrome (ARDS). Thorax 1998;53:292-4. Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 2003;348:683-93.
394
BMJ | 25 AUGUST 2007 | VOLUME 335
You might also like
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- Arti Revi 11Document8 pagesArti Revi 11LuLu NikhlaturNo ratings yet
- Recentadvancesinthe Managementofacute Exacerbationsofchronic ObstructivepulmonarydiseaseDocument16 pagesRecentadvancesinthe Managementofacute Exacerbationsofchronic Obstructivepulmonarydiseaseadek07No ratings yet
- Demystifying COVID-19: Understanding the Disease, Its Diagnosis. and TreatmentFrom EverandDemystifying COVID-19: Understanding the Disease, Its Diagnosis. and TreatmentNo ratings yet
- The Acute Respiratory Distress Syndrome: Ariel M. Modrykamien, MD, and Pooja Gupta, MDDocument9 pagesThe Acute Respiratory Distress Syndrome: Ariel M. Modrykamien, MD, and Pooja Gupta, MDGitaNo ratings yet
- Lakshminarasimhachar 2016Document18 pagesLakshminarasimhachar 2016mel.espinoza90No ratings yet
- The Acute Respiratory Distress Syndrome: Review SeriesDocument10 pagesThe Acute Respiratory Distress Syndrome: Review Seriesadek07No ratings yet
- Ali 01Document10 pagesAli 01Juan Fernando Garcia RobledoNo ratings yet
- PHYS THER-1981-Kigin-1724-36Document15 pagesPHYS THER-1981-Kigin-1724-36Bobeică S MihailNo ratings yet
- RCT of Aprv Vs LPV in Ards PtsDocument11 pagesRCT of Aprv Vs LPV in Ards PtsOldriana Prawiro HapsariNo ratings yet
- Relationship Between Extravascular Lung Water and Severity Categories of Acute Respiratory Distress Syndrome by The Berlin DefinitionDocument9 pagesRelationship Between Extravascular Lung Water and Severity Categories of Acute Respiratory Distress Syndrome by The Berlin DefinitionVictor Euclides Briones MoralesNo ratings yet
- Acute Respiratory Distress Syndrome - Epidemiology, Pathophysiology, Pathology, and Etiology in Adults - UpToDateDocument32 pagesAcute Respiratory Distress Syndrome - Epidemiology, Pathophysiology, Pathology, and Etiology in Adults - UpToDatecuentaparatrabajosdelau10No ratings yet
- Copd Review 2002 ChestDocument8 pagesCopd Review 2002 ChestLeonardo GarciaNo ratings yet
- Concise Clinical Review: Non-Cystic Fibrosis BronchiectasisDocument11 pagesConcise Clinical Review: Non-Cystic Fibrosis BronchiectasisJuwitaNo ratings yet
- Acute Asthma Exacerbations: Phenotypes and Management: Charles B. Cairns, MD TDocument10 pagesAcute Asthma Exacerbations: Phenotypes and Management: Charles B. Cairns, MD TKaren Aguilar PalominoNo ratings yet
- Prophylaxis and Treatment For AspirationDocument19 pagesProphylaxis and Treatment For Aspirationbalab2311No ratings yet
- Acute Respiratory Distress Syndrome (ARDS) : An Evidence-Based ManagementDocument14 pagesAcute Respiratory Distress Syndrome (ARDS) : An Evidence-Based ManagementshofwaNo ratings yet
- Andrew Et AlDocument18 pagesAndrew Et AlmuarifNo ratings yet
- Mechanical Ventilation - Lessons From The ARDSNet TrialDocument5 pagesMechanical Ventilation - Lessons From The ARDSNet TrialRDG20202No ratings yet
- Ards 2Document7 pagesArds 2LUCIBELLOT1No ratings yet
- Acute Respiratory Distress Syndrome: Jesse B. Hall, MD, FCCPDocument12 pagesAcute Respiratory Distress Syndrome: Jesse B. Hall, MD, FCCPMayun CacoellNo ratings yet
- Preoperative Pulmonary EvaluationDocument8 pagesPreoperative Pulmonary EvaluationKhaled AlameriNo ratings yet
- Pulmonary Function TestDocument7 pagesPulmonary Function TestGhada HusseinNo ratings yet
- Cardiovascular Comorbidities in Chronic Obstructive Pulmonary Disease (COPD) - Current Considerations For Clinical PracticeDocument14 pagesCardiovascular Comorbidities in Chronic Obstructive Pulmonary Disease (COPD) - Current Considerations For Clinical Practicerbatjun576No ratings yet
- Review ArdsDocument25 pagesReview ArdsAdel HamadaNo ratings yet
- COPD2019Document9 pagesCOPD2019ClintonNo ratings yet
- Acute Lung InjuryDocument5 pagesAcute Lung InjuryKinanti Devia LarasatiNo ratings yet
- Low-Tidal-Volume Ventilation in The Acute Respiratory Distress SyndromeDocument8 pagesLow-Tidal-Volume Ventilation in The Acute Respiratory Distress SyndromeJimmy Christianto SuryoNo ratings yet
- What's New in Respiratory DisordersDocument4 pagesWhat's New in Respiratory DisorderssobanNo ratings yet
- Acute Respiratory Distress Syndrome - Epidemiology, Pathophysiology, Pathology, and Etiology in Adults - UpToDateDocument27 pagesAcute Respiratory Distress Syndrome - Epidemiology, Pathophysiology, Pathology, and Etiology in Adults - UpToDateFrancisco MuñozNo ratings yet
- Acute Exacerbation of Chronic Obstructive Pulmonary DiseaseDocument5 pagesAcute Exacerbation of Chronic Obstructive Pulmonary Diseaseteguh sNo ratings yet
- Thorax 2010 MacDuff Ii18 31Document15 pagesThorax 2010 MacDuff Ii18 31guillosarahNo ratings yet
- BTS 2010 Guidelines Management of Spontaneous PneumothoraxDocument15 pagesBTS 2010 Guidelines Management of Spontaneous Pneumothoraxchngwq93No ratings yet
- Acute Respiratory Distress John Rae 2019Document6 pagesAcute Respiratory Distress John Rae 2019yyullyyannaNo ratings yet
- Respiratory - ARDS Vent Revised - QuestionsDocument6 pagesRespiratory - ARDS Vent Revised - QuestionsRyan ReNo ratings yet
- Clinical Manifestations and Diagnosis of Bronchiectasis in AdultsDocument16 pagesClinical Manifestations and Diagnosis of Bronchiectasis in AdultsDAT TRANNo ratings yet
- Respiratory Medicine: XDocument8 pagesRespiratory Medicine: XYuriz HkNo ratings yet
- ArdsDocument69 pagesArdsdrabdallakawareNo ratings yet
- Thorax 2010 MacDuff Ii18 31Document15 pagesThorax 2010 MacDuff Ii18 31cynthiaNo ratings yet
- Chest: Recent Advances in Chest MedicineDocument9 pagesChest: Recent Advances in Chest MedicinesmansakobiNo ratings yet
- Pneumothorax Classification and Etiology: Clinics in Chest Medicine November 2021Document18 pagesPneumothorax Classification and Etiology: Clinics in Chest Medicine November 2021Maria Asri PranataNo ratings yet
- ArdsDocument7 pagesArdsIpar DayNo ratings yet
- Acute Non-Cardiogenic Pulmonary EdemaDocument4 pagesAcute Non-Cardiogenic Pulmonary EdemaDr. FarhanNo ratings yet
- 29 - Pavlovsky (2022)Document12 pages29 - Pavlovsky (2022)Fermin LombardiaNo ratings yet
- Gold Criteria For COPDDocument8 pagesGold Criteria For COPDmrppserodio7856No ratings yet
- Surgical Therapy For Necrotizing Pneumonia and Lung Gangrene PDFDocument6 pagesSurgical Therapy For Necrotizing Pneumonia and Lung Gangrene PDFmichael24kNo ratings yet
- Idiopathic Pulmonary Fibrosis: Interstitial Lung DiseaseDocument5 pagesIdiopathic Pulmonary Fibrosis: Interstitial Lung DiseaseAmjaSaudNo ratings yet
- Acute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesDocument17 pagesAcute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesCandice ChengNo ratings yet
- Perioperative Lung ProtectionDocument6 pagesPerioperative Lung ProtectionWilliamRayCassidyNo ratings yet
- Perioperative Pulmonary Atelectasis - Part II. Clinical Implications Anesthesiology American Society of AnesthesiologistsDocument78 pagesPerioperative Pulmonary Atelectasis - Part II. Clinical Implications Anesthesiology American Society of Anesthesiologistsrina yulianaNo ratings yet
- Pneumothorax Classification and Etiology: Clinics in Chest Medicine November 2021Document18 pagesPneumothorax Classification and Etiology: Clinics in Chest Medicine November 2021DesyaNo ratings yet
- The Acute Respiratory Distress Syndrome in 2013: Review Open AccessDocument6 pagesThe Acute Respiratory Distress Syndrome in 2013: Review Open Accessindriyanti natasya ayu utami kottenNo ratings yet
- Actinomyces Pulmonar 2013Document8 pagesActinomyces Pulmonar 2013Elizabeth SantillanNo ratings yet
- Pneumothorax: Classification and EtiologyDocument17 pagesPneumothorax: Classification and EtiologyPASMOXNo ratings yet
- Ventilation During Lung Resection and Critical Care ComparativeDocument11 pagesVentilation During Lung Resection and Critical Care Comparativeema moralesNo ratings yet
- Ajtccm 27 1 054Document5 pagesAjtccm 27 1 054Saniska NCTNo ratings yet
- Copd 2Document26 pagesCopd 2Abid SunhanNo ratings yet
- Complicatii PneumonieDocument9 pagesComplicatii PneumonieTatiana JalbaNo ratings yet
- Table: Causes of and Conditions Associated With BronchiectasisDocument6 pagesTable: Causes of and Conditions Associated With BronchiectasisfallenczarNo ratings yet
- No 25 Bharathi Nagar Kamarajar Road Uppilipalayam Post Coimbatore Pincode: 641015 Contact No: 9092912220Document1 pageNo 25 Bharathi Nagar Kamarajar Road Uppilipalayam Post Coimbatore Pincode: 641015 Contact No: 9092912220Vijeyachandhar DorairajNo ratings yet
- FNH LiverDocument10 pagesFNH LiverVijeyachandhar DorairajNo ratings yet
- Pgi Mdms ProspectusDocument16 pagesPgi Mdms ProspectusVijeyachandhar DorairajNo ratings yet
- Cary Blair Transport MediumDocument1 pageCary Blair Transport MediumVijeyachandhar DorairajNo ratings yet
- Nbme 1Document39 pagesNbme 1rockNo ratings yet
- Skeletal Dysplasia3 PDFDocument7 pagesSkeletal Dysplasia3 PDFVijeyachandhar DorairajNo ratings yet
- Histone Modifications12Document70 pagesHistone Modifications12Vijeyachandhar DorairajNo ratings yet
- Measurement of Renal Function in PracticeDocument5 pagesMeasurement of Renal Function in PracticeVijeyachandhar DorairajNo ratings yet
- Arginine Stimulation Test For GHRHDocument2 pagesArginine Stimulation Test For GHRHVijeyachandhar DorairajNo ratings yet
- Nucleotide Excision Repair Defect and DiseasesDocument8 pagesNucleotide Excision Repair Defect and DiseasesVijeyachandhar DorairajNo ratings yet
- Arc Ureteral StonesDocument79 pagesArc Ureteral StonesVijeyachandhar DorairajNo ratings yet
- BehaviourismDocument9 pagesBehaviourismVijeyachandhar DorairajNo ratings yet
- Faq Aiims PG July 2015Document6 pagesFaq Aiims PG July 2015Vijeyachandhar DorairajNo ratings yet
- WHO Dengue Guidelines 2013Document160 pagesWHO Dengue Guidelines 2013Jason MirasolNo ratings yet
- Hepatorenal SyndromeDocument14 pagesHepatorenal SyndromeVijeyachandhar DorairajNo ratings yet
- Q Rate of Removal of Substance: F GC BS GCDocument2 pagesQ Rate of Removal of Substance: F GC BS GCVijeyachandhar DorairajNo ratings yet
- Venous ThromboliskDocument5 pagesVenous ThromboliskVijeyachandhar DorairajNo ratings yet
- 2009 CMT Framework (Revised Aug 2012)Document166 pages2009 CMT Framework (Revised Aug 2012)Vijeyachandhar DorairajNo ratings yet
- Hereditary HemochromatosisDocument6 pagesHereditary HemochromatosisVijeyachandhar DorairajNo ratings yet
- Transthoracic EcocardiographyDocument5 pagesTransthoracic EcocardiographyVijeyachandhar DorairajNo ratings yet
- Clinical Review: Systemic Lupus ErythematosusDocument5 pagesClinical Review: Systemic Lupus ErythematosusVijeyachandhar DorairajNo ratings yet
- All ChildrenDocument5 pagesAll ChildrenVijeyachandhar DorairajNo ratings yet
- Cocci Dio I o MycosisDocument7 pagesCocci Dio I o MycosisVijeyachandhar DorairajNo ratings yet
- H Pylori Infection TreatmentDocument5 pagesH Pylori Infection TreatmentVijeyachandhar DorairajNo ratings yet
- Op PoisoningDocument6 pagesOp PoisoningVijeyachandhar DorairajNo ratings yet
- Lower Gi Bleeding in AdultsDocument7 pagesLower Gi Bleeding in AdultsVijeyachandhar DorairajNo ratings yet
- BMJ 335 7628 CR 01037 PDFDocument5 pagesBMJ 335 7628 CR 01037 PDFDescargasExposicionesNo ratings yet
- Benign Prostatic Hyperplasia. - Diagnosis: Clinical ReviewDocument4 pagesBenign Prostatic Hyperplasia. - Diagnosis: Clinical ReviewVijeyachandhar DorairajNo ratings yet
- OB Gyne HistoryDocument2 pagesOB Gyne HistoryNeil Victor Ongco PajugotNo ratings yet
- 1 Gme Regulations 1997 Amended Upto May 2018Document114 pages1 Gme Regulations 1997 Amended Upto May 2018seethahereNo ratings yet
- Chocolate and The Brain: Neurobiological Impact of Cocoa Flavanols On Cognition and BehaviorDocument9 pagesChocolate and The Brain: Neurobiological Impact of Cocoa Flavanols On Cognition and BehaviorStefan AvramovskiNo ratings yet
- Crystal Aromatherapy Lesson 1Document9 pagesCrystal Aromatherapy Lesson 1crystals21No ratings yet
- NIPPVDocument35 pagesNIPPVAnusha VergheseNo ratings yet
- E-Exercise Book: Material Safety Data Sheet (MSDS)Document10 pagesE-Exercise Book: Material Safety Data Sheet (MSDS)Zia Ur RehmanNo ratings yet
- Lactose Intolerance in InfantsDocument10 pagesLactose Intolerance in InfantsflorenceNo ratings yet
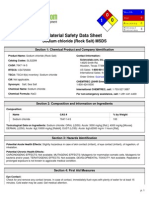
- Sodium Chloride (Rock Salt) MSDS: Section 1: Chemical Product and Company IdentificationDocument6 pagesSodium Chloride (Rock Salt) MSDS: Section 1: Chemical Product and Company IdentificationMohamed MaghawryNo ratings yet
- Crisis HiperglicémicaDocument31 pagesCrisis HiperglicémicaMelany Esteban BarzolaNo ratings yet
- Drug Card BenadrylDocument1 pageDrug Card BenadrylAdrianne Bazo100% (1)
- PERIMETRY Introduction GuideDocument70 pagesPERIMETRY Introduction GuideDana Andreea Popescu100% (1)
- Health Policy Memo MgenoviaDocument5 pagesHealth Policy Memo Mgenoviaapi-302138606No ratings yet
- Medical Nutrition in Neurobehavioral2Document34 pagesMedical Nutrition in Neurobehavioral2Lia Dwi JayantiNo ratings yet
- 17q21.31 Microdeletions FTNWDocument8 pages17q21.31 Microdeletions FTNWjohavenbNo ratings yet
- Position Document Local Management Diabetic Foot UlcersDocument28 pagesPosition Document Local Management Diabetic Foot Ulcerspolin timiselaNo ratings yet
- Antidepression ReikiDocument6 pagesAntidepression ReikiDoc Lyman88% (8)
- Effectiveness of A Comprehensive Hand Hygiene Program ForDocument11 pagesEffectiveness of A Comprehensive Hand Hygiene Program Form1k0eNo ratings yet
- Retinos PDFDocument83 pagesRetinos PDFPaulo Gan100% (2)
- EndometriosisDocument153 pagesEndometriosisoannny8661No ratings yet
- DDFGGDocument2 pagesDDFGGstrafforNo ratings yet
- Pemanfaatan Teknik Assisted Hatching Dalam Meningkatkan Implantasi EmbrioDocument10 pagesPemanfaatan Teknik Assisted Hatching Dalam Meningkatkan Implantasi EmbrioMumutTeaNo ratings yet
- A Regenerative Interventional Approach To The Management of Degenerative Low Back PainDocument16 pagesA Regenerative Interventional Approach To The Management of Degenerative Low Back PainAthenaeum Scientific PublishersNo ratings yet
- HerbalismDocument18 pagesHerbalismmieNo ratings yet
- NURSING BOOK LIST - Docx FinalDocument10 pagesNURSING BOOK LIST - Docx FinalChaitanya RkNo ratings yet
- 11th Grade Before Band Aids TextDocument1 page11th Grade Before Band Aids Textعبدالرحمن باجسيرNo ratings yet
- Can Oral Sex Cause Throat CancerDocument4 pagesCan Oral Sex Cause Throat CancerjyuldipNo ratings yet
- Article - CVD Cardiac Arrest - Bls AclsDocument2 pagesArticle - CVD Cardiac Arrest - Bls AclsAkhosh SomarajanNo ratings yet
- Daftar Pustaka NewDocument2 pagesDaftar Pustaka NewRini LianingsihNo ratings yet
- Interpretation of Histograms and Its Correlation WDocument5 pagesInterpretation of Histograms and Its Correlation WrezqiNo ratings yet
- JCIA Handbook 2020Document61 pagesJCIA Handbook 2020WAQASNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (28)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (393)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (4)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)