Professional Documents
Culture Documents
Dental Practitioner Guidance
Uploaded by
Adilah Zakiyati0 ratings0% found this document useful (0 votes)
30 views16 pagesDental Practitioner Guidance
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDental Practitioner Guidance
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
30 views16 pagesDental Practitioner Guidance
Uploaded by
Adilah ZakiyatiDental Practitioner Guidance
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 16
1
Guidance and Training manual to accompany the
Full Standard Clinical Survey Form
European Non Carious Cervical Lesions Dentine
Hypersensitivity Development Programme
November 2010
2
Dental Practitioner Guidance
Introduction
The ESCARCEL Full Standard Clinical Survey Assessment has been designed for use in the dental
surgery environment. There are four main sections to the form:
1. Identification and General Information;
2. Periodontal Health and Disease Severity Assessments;
3. Non Carious Cervical Lesions Assessment
4. Dentine Hypersensitivity Assessment;
Within each section there may be more than one related question. It is recommended that the
examination follows the order of questions on the form.
It should be noted that all questions are applicable to all participants. A symbol next to each question
will provide a reminder when a section of the clinical assessment applies to restricted age groups.
Figure 1: Symbols indicating applicable participant age groups: Adults 18-35 years old
It is important that all appropriate parts of the clinical assessment are completed accurately. The dental
practitioner and the chosen scribe should co-operate to ensure this is done.
Section 1: Identification and General Information
Before you begin the clinical assessment make sure the Identification and general information section
of the ESCARCEL. Full Standard Clinical Survey Assessment has been properly completed. Make sure
you leave no data entry area blank.
For the purpose of this pilot study, the participating countries have been allocated codes which should
be entered into box 1. Then, enter the date when the examination is carried out (box 2), the patients 3-
digit identity number (box3) and the examiners 2-digit identity number (box 4).
Boxes 5 and 6 are used for the participants age and sex respectively.
For adult patients, box 7 should be used to indicate their highest grade of education according to the
key.
Please indicate the current or recent employment status (box 8). Examiners should use their judgement
when asking potentially embarrassing questions.
Adults only 18-35 years old
3
Pre-Clinical Assessment Protocol
For the ESCARCEL Full Standard Clinical Survey Assessment you will need a dental light and the
following equipment:
Dental mirror
Dental probe PDT Sensor CPI probe Type U.S. (Williams) 2.3.4.5.7.9
Three in-one air syringe, cotton wool rolls
Section 2: Periodontal Health and Disease Severity
Assessment
Quick View Summary
o Participants aged 18 to 34 years only
o Full mouth charting
Introduction
The Periodontal Health Assessment and Periodontal Disease severity assessment can be found on
Periodontal condition section of the form. This section is made up of 3 indicators: Probing
depth, where you will be asked to record the Periodontal Pocket index; Indicator Gingival
Bleeding and Loss of Attachment, which deals with measuring the loss of attachment around
the mouth. It should be noted that these questions are applicable to all participants. The most
reliable way of measuring loss of attachment is immediately after recording bleeding and the
depth score for that tooth. Therefore you should record three measures in a teeth before moving
on to the next, remembering that third molar teeth are not counted.
Pre-Periodontal Assessments Protocol
Check Health Status
Before you begin, assess the participants health status. Note special precautions should be taken
for those participants with:
o Bleeding disorders (e.g. those taking anticoagulant medications and haemophiliacs)
o Antibiotic cover requirements e.g. those who have had infective endocarditis, with valve
replacements and those with indwelling conduits (British Society for Antimicrobial
Chemotherapy guidelines, 2006)
Equipment Periodontal probes are used for this examination which have circumferential
markings to help assess pocket depth and loss of attachment.
The sequence to collect the indexes is: Gingival Bleeding Index, Periodontal Pocket Index,
Loss of Attachment Index.
Measuring Gingival Bleeding
During the probing depth assessment, the bleeding on probing index (Yes/No) is sufficient to
highlight the bleeding condition. Score are: 0: No; 1: Yes; 9: Cannot be determined; X: Excluded.
4
Bleeding observed, directly or by using a mouth mirror, after probing. The sensing force used
should be no more than 20 grams
Using the Periodontal Probing Depth Index
The following indicators of periodontal status are used for this assessment:
(0) Health gingival; 1 = Pocket 2 -3] mm; 2 = Pocket 3-4] mm; 3 = Pocket 4 or 5mm, 4 = Pocket
5-7] mm; 5 = Pocket 7-9] mm; 6= Pocket 9mm and more and 9 = Cannot be determined; X =
Excluded teeth
A specially designed lightweight probe with 0.5mm ball tip is used, The PDT Sensor CPI probe
Type U.S. (Williams) 2.3.4.5.7.9 is recommended.
Figure 1: Showing an example of a PDT Sensor CPI probe Type U.S. (Williams) 2.3.4.5.7.9. This probe
should be used for measurement of the extent of attachment loss.
Sensing gingival pockets
Sensing gingival pockets: An index tooth should be probed, using the probe as a sensing
instrument to:
Determine pocket depth
The sensing force used should be no more than 20 grams. A practical test for establishing this
force is to place the probe point under the thumb nail and press until blanching occurs. When the
probe is inserted, the tip should follow the anatomical configuration of the surface of the tooth
root. If the patient feels pain during probing, this is indicative of the use of too much force. The
probe tip should be inserted gently into the gingival sulcus or pocket and the total extent of the
sulcus or pocket explored. For example, the probe is placed in the pocket at the disto-buccal
surface of the second molar, as close as possible to the contact point with the third molar, keeping
the probe parallel to the long axis of the tooth. The probe is then swept gently along the bottom of
the pocket, with short upward and downward movements, along the gingival sulcus or pocket to
the mesial surface of the second molar, and from the disto-buccal surface of the first molar
towards the contact area with the premolar. A similar procedure is carried out for the lingual
surfaces, starting disto-lingually/palatally to the second molar. The pocket depth is measured from
the base of the pocket to the tip of the gingival crest.
Examination and recording
The index teeth should be probed and the highest score recorded in the Probing Depth box on the
clinical form. The depth codes are:
0 = Healthy (1 black band on the probe visible)
1 = Pocket 2 -3] mm (1 black band on the probe not visible)
2 = Pocket 3-4] mm (1with and 1 black bands on the probe not visible gingival)
3 = Pocket 4 or 5] mm (1with and 2 black bands on the probe not visible gingival)
4 = Pocket 5-7] mm (2 with and 2 black bands on the probe not visible)
5 = Pocket 7-9] mm (3 with and 1 black bands on the probe not visible)
6= Pocket 9mm and more
9 = Cannot be determined
X = Excluded tooth
5
Code 9 is placed in the appropriate box when it is not possible to make a reliable recording (e.g.
large accumulations of calculus prohibiting proper probing of pockets).
Examples of Coding according to Periodontal Depth Index criteria
PDI Code 0: Healthy, no bleeding observed, but all of the lower dark band of the probe is visible,
no pocket 4 or 5mm, no pocket 6mm or more
PDI Code 1: Bleeding observed, but all of the lower (2mm to 3mm) white band of the probe is
visible, no pocket 4 or 5 mm, no pocket 6mm or more
PDI Code 3: Pocket 4 or 5mm (in photo pocket extends to top of second dark band at 4mm), no
pocket 6mm or more
6
PDI Code 4: Pocket 5-7 mm
Measuring Attachment Loss
Loss of attachment will be recorded on the appropriate index tooth in addition to the PDI score, in
order to obtain an estimate of the life-time accumulated destruction of the periodontal attachment.
Probing pockets depths give some indication of attachment loss. However, this measurement
becomes inadequate when recession of the gingiva becomes apparent (the CEJ becomes visible).
When shallow pocketing of 4-5mm (PDI score 3) is recorded at the highest score for a tooth and
no recession is visible, the estimated maximum attachment loss for that sextant is, apart from
exceptional cases, no more than 3mm and no separate record of attachment loss is made. When
deep pockets (6mm or more, equal to PDI score 4 or more) are recorded or when recession of the
gingiva is apparent (the CEJ is visible); the examiner will access and record the maximum
attachment loss at the index teeth in the same sextant with the same probe.
Definition of important terms
Clinical attachment level is the point (point C on the diagram) at which the gingival attaches to a
root surface.
Loss of attachment (point B point C on the diagram) is measured by clinical probing.
Lifetime cumulative attachment loss is the measurement (in mm) from the cemento-enamel
junction (point B) to the clinical attachment level at a given point in time.
Pocket depth and loss of attachment
(Glavind & Le 1967)
Cemento-Enamel Junction (point B) is the anatomical point where the root and crown of a tooth
meet. For convenience (and reproducibility), it is used as a fixed point from which to measure
attachment loss. However, even at healthy sites the attaching fibres are rarely found at this point.
7
Hence the threshold for attachment loss is usually set at 1 or 2 mm as measurements of less than
these figures do not represent true clinical attachment loss.
Measurement of loss of attachment health
Periodontal examination employs a sterile, disposable US Williams PDT Sensor probe, at a
pressure of 20 g. Clinical attachment level is defined as the distance from the cement-enamel
junction to the tip of the probe. Attachment loss is measured (to the nearest mm) by simple
probing by identifying the cementoenamel junction and measuring the distance to the base of the
pocket. Probing depth is defined as the distance from the soft tissues margin to the tip of the
probe. All teeth are examined excepted third molars which are excluded from analysis.
Variables are assessed for two sites per tooth: median-vestibular (mid-buccal); median-
lingual/palatine.
Periodontal indices are recorded in the following order: probing depth; and probing attachment
loss. The recording sequence is as follows: first, median-vestibular 17 for the LA indices; second,
median-palatine 17. The recording sequence for the four quadrants is quadrant 1, quadrant 2,
quadrant 3, and then quadrant 4.
Examination and recording
The index teeth should be probed and the highest score recorded in the Loss of Attachment box
on the clinical form. The depth codes are:
0 = Healthy 0 mm
1 = Slight 1-2] mm
2 = Moderate 3-4] mm
3 = Severe 5 mm or more
9 = Cannot be determined
X = Excluded tooth
Examples of Coding according to loss of attachment
LA Code 0: Health: Periodontal attachment loss 0 mm
LA Code 0: Health: Periodontalchment loss 0 mm
LA Code 1: Slight: Periodontal attachment loss 1 or 2 mm
8
LA Code 2: Moderate: Periodontal attachment loss 3 or 4 mm
LA Code 3: Severe: Periodontal attachment 5mm or more
Photographs: Denis Bourgeois
Section 3: Non Carious Cervical Lesions
The Basic Erosive Wear Examination (BEWE) has been designed to provide a simple scoring
system that can be used with the diagnostic criteria of all existing criteria of all existing indices
9
aiming to transfer their results into one unit which is the BEWE score sum. This Index has been
adapted to measure in this study every tooth and cover the buccal and lingual surfaces only in
order to comply with the primary objective of the study aiming to evaluate the prevalence of
NCCl in 18 to 35 years old (inclusive) of European subjects.
Non Carious Cervical Lesions Assessment Protocol
Remove any removable denture
Ask the participant to remove any removable oral prosthesis prior to completing the dental
assessment.
Clean and dry the teeth
Prior to the NCCL assessment make sure the participants natural teeth are clean. You
should aim, at the very least; to clean the participants teeth with a dry toothbrush to remove
plaque and flossing may be required in some cases. It may still be necessary during the
examination to further remove plaque deposits in order to visualise all tooth surfaces clearly.
Using the BEWE Codes
To use the BEWE codes correctly, the participants teeth must be clean and dry prior to
assessment. Each tooth surface should be visually assessed and allocated an appropriate 2 digit
BEWE code. This is constructed from the individual numerical codes see Table 1. The four level
score grades appearance or severity of wear on the teeth from no surface loss (0), initial loss of
enamel surface texture (1), distinct defect, hard tissue loss (dentine) less than 50% of the surface
area(2) or hard tissue loss more than 50% of the surface area.
Buccal/facial and lingual/palatal surfaces are examined with the highest score recorded.
Table 1: BEWE Codes
BEWE Codes [Lussi, 2008]
Localisation Codes
0 = No erosive wear 0 = Anatomic crown and over cervical localization
1 = Initial loss of surface texture 1 = Anatomic crown in cervical localization
2 = Distinct defect, hard tissue loss minor than 50% of the surface area 2 = Anatomic root in cervical localization
3 = Hard tissue loss more or equal than 50% of the surface area 3 = Anatomic crown and root cervical localization
9= No recorded (tarter, suppuration)
Missing Teeth = X
you could have as result to note 0 or 10, 11, 12 or 20, 21, 22 or 30, 31, 32 depend the loss of surface
(clinical crown) and the localization and 9 (no recorded).
For each tooth, the index grades 2 individual surfaces
o Buccal- assessment includes the cervical buccal portion
o Buccal cervical = cervical 1/3rd of tooth
Figure 2: Example of BEWE code allocation
10
BEWE Codes [Lussi, 2008]
Localisation Codes
0 = over cervical
0 = No erosive wear 1 = anatomic crown cervical
1 = Initial loss of surface texture 2 = anatomic root cervical
2 = Distinct defect, hard tissue loss minor than 50% of the surface area
3 = Hard tissue loss more or equal than 50% of the surface area 3 = Anatomic crown and root cervical localization
9= No recorded (tarter, suppuration)
:
you could have as result to note 0 or 10, 11, 12 or 20, 21, 22 or 30, 31, 32 depend the loss of surface (clinical
crown) and the localization and 9 (no recorded).
In cases where a tooth or teeth are missing you should use the Missing Teeth two digit BEWE
codes instead. There are three missing teeth codes: 97 (for a tooth extracted due to caries), 98 (for
a tooth missing for another reason other than caries) and 99 for a tooth still to erupt, and code P
where a tooth is missing but has been replaced by a fixed prosthesis such as a bridge pontic or
implant.
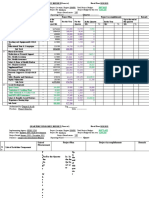
There are two charts in the dental disease assessment section of this form. The first chart is for
upper teeth while the second chart is for lower teeth. Each chart is made up of individual tooth
surfaces (Buccal and Lingual/Palatal) corresponding to each tooth in the arch.
For example, a sound tooth would be coded 00 in the bottom box. A two-digit code should be
used to indicate each tooth surfaces condition. Sound surfaces may be left blank but care must be
taken to ensure that codes are recorded in the correct space of the chart.
Figure 3: Example of Completed Upper Arch Chart
Upper Left
17 16 15 14 13 12 11 21 22 23 24 25 26 27
B 0 23 11
P 11 13
STAGE ONE: Coding Restorations
There are 4 erosion codes (0-3) that you can select from when coding the presence or absence
of a NCCL on individual tooth surfaces. For each surface you should select one of the four
codes as appropriate and record it as the first digit of the two digit BEWE code.
BEWE Code: 22
First digit = Erosion code
Second digit = Location code
11
Figure 4: Coding Restorations
BEWE Codes (Lussi, 2008)
0= No erosive wear
1=Initial loss of surface texture
2= Distinct defect, hard tissue loss than 50% of the surface area
3= Hard tissue loss more or equal than 50% of the surface area
If an initial loss of surface texture is
present you should use code 1 as the
first digit.
CODE 2: NCCL
If a distinct defect, hard tissue loss minor
than 50% of the surface area is present
you should use 2 as the first digit
Select from five
restoration codes
and record as first
digit of BEWE
code
CODE 1: NCCL
12
Photographs: A. Lussi (2);
STAGE TWO: Coding Location
There are three location codes (0, 1, 2) that you can select from when coding the presence or
absence of NCL on individual tooth surfaces. For each surface you should select one of the
three codes as appropriate and record it as the second digit of the two digit BEWE code.
Figure 5: Coding location
Location Codes)
0= Anatomic crown and over cervical localization
1=Anatomic crown in cervical localization
2= Anatomic root in cervical localization
3= Anatomic crown and root cervical localization
Each Caries code will now be considered in more detail:
CODE 3: NCCL
If hard tissue loss more or equal than 50% of
the surface area, then code it as a 3.
Location CODE 1: Anatomic crown cervical
Select from three
location codes and
record as second
digit of BEWE
code
13
STAGE THREE: Coding Missing Teeth
There are 4 codes that you can select from for coding the absence of teeth and one which
allows you to code if a fixed prosthesis has been placed. This is a two digit code and is
summarized at the bottom of the second column of the adapted table of BEWE codes. (It
should be noted that bridge pontics and implants, if present, are coded as missing teeth, using
code P).
Section 4: Dentine Hypersensitivity Assessment
Introduction
Short, sharp pain arising from exposed dentin in response to stimuli, typically thermal,
evaporative, tactile, osmotic or chemical which cannot be ascribed to any other form of dental
defect or pathology (Holland 1997)
Pre-Hypersensitivity Assessment Protocol
Location CODE 2: Anatomic root cervical
Location CODE 3: Crown and root cervical
14
Dentine Hypersensitivity indices are recorded in the following order: Hypersensitivity and Schiff
cold index.
Measuring Hypersensitivity
Hypersensitivity Index
A simple answer following the sec airblast on the buccal surface of every tooth (except the 2
nd
molars) (Yes/No) is sufficient to highlight the bleeding condition. Score are: 0: No; 1: Yes; 9:
Cannot be determined; X: Excluded.
Examiner assessment of pain Schiff cold air sensitivity scale
Following the evaporative air blast, sensitivity will be recorded by the examiner using the Schiff
Cold Air Sensitivity Scale [Schiff, 1994].
The scale is as follows:
0 = Subject does not respond to air stimulus
1 = Subject responds to air stimulus but does not request discontinuation of stimulus
2 = Subject responds to air stimulus and requests discontinuation or moves from stimulus
3 = Subject responds to air stimulus, considers stimulus to be painful, and requests
discontinuation of the stimulus
Exclusion criteria for testing teeth for sensitivity:
1. Teeth with exposed dentine but with deep, defective or facial restorations, teeth used as
abutments for fixed or removable partial dentures, teeth with full crowns, orthodontic
bands, extensive caries or cracked enamel.
2. Sensitive teeth with contributing aetiologies other than erosion, abrasion or recession of
exposed dentine.
The identified teeth - recession and or NCCL presence- are tested for sensitivity with a
cold air blast and each tooth identified has a Schiff score associated with it, recorded on
one line and another a HD score recorded on line. Exclude 7's and 8's.
The examiner will assess the evaporative (air) sensitivity on the teeth (incisors, canines, premolars
and 1
st
molars) identified at baseline. This assessment is made by directing a one-second
application of air from a triple air dental syringe at 60 psi ( 5 psi) and operating temperature
range 19C (5C) to the exposed dentine surface from a distance of approximately 1 cm for 1
second. Use fingers of non-dominant hand to mask the teeth either side. Observe the body and
eyes of the subject during the application of the stimulus.
Variables are assessed for one site per tooth: buccal. The recording sequence is as follows: buccal
17; second buccal 16, etc. The recording sequence for the four quadrants is quadrant 1, quadrant
2, quadrant 3, and then quadrant 4.
Suggested guidelines
If no response (0) check with the volunteer did you feel anything? if yes then 1
Vocal response with no movement away from the stimulus = 1
Vocal response with head and neck movement = 2
Vocal response with limb movement and yes to was that painful?=3
15
Important: Examiner will need to first score the Schiff value by communicating discreetly to his
scribe and then ask the question to the subject in order to complete the Hypersensitivity Y/N
assessment
16
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Erich FrommDocument2 pagesErich FrommTina NavarroNo ratings yet
- Hippocrates OathDocument6 pagesHippocrates OathSundary FlhorenzaNo ratings yet
- MelatoninaDocument32 pagesMelatoninaCodrut GeorgescuNo ratings yet
- Liquid Enema ProcedureDocument3 pagesLiquid Enema Procedureapi-209728657No ratings yet
- Subquery ProblemDocument9 pagesSubquery ProblemAbhi RamNo ratings yet
- Lead Avr PDFDocument9 pagesLead Avr PDFsiddharthNo ratings yet
- Senographe Crystal: The Choice Is Crystal ClearDocument7 pagesSenographe Crystal: The Choice Is Crystal ClearmuhammadyassirNo ratings yet
- Arann Magazine, Issue 1-2-Online VersionDocument36 pagesArann Magazine, Issue 1-2-Online VersionmujismileNo ratings yet
- People vs. MediosDocument10 pagesPeople vs. MediostheresagriggsNo ratings yet
- Course Syllabus Manufacturing Processes (1) Metal CuttingDocument4 pagesCourse Syllabus Manufacturing Processes (1) Metal CuttingG. Dancer GhNo ratings yet
- TelfastDocument3 pagesTelfastjbahalkehNo ratings yet
- Sindh Rescue 1122 Test Sample PapersDocument12 pagesSindh Rescue 1122 Test Sample PapersMAANJONY100% (1)
- PSB 3441 CH 1 HallucinogensDocument2 pagesPSB 3441 CH 1 HallucinogensAnonymous lm3GIU45No ratings yet
- Project PlanDocument55 pagesProject PlanAlfredo SbNo ratings yet
- RISK MANAGEMENT - Imo Multilingual Glossary On Risk Management (Secretariat)Document17 pagesRISK MANAGEMENT - Imo Multilingual Glossary On Risk Management (Secretariat)Martin NiNo ratings yet
- Owner'S Manual: Explosion-Proof Motor Mf07, Mf10, Mf13Document18 pagesOwner'S Manual: Explosion-Proof Motor Mf07, Mf10, Mf13mediacampaigncc24No ratings yet
- Variable Compression Ratio Engines A Literature Review: December 2018Document15 pagesVariable Compression Ratio Engines A Literature Review: December 2018Er Samkit ShahNo ratings yet
- CPhI Japan InformationDocument22 pagesCPhI Japan InformationctyvteNo ratings yet
- Sesion 2 - Copia-1Document14 pagesSesion 2 - Copia-1Maeva FigueroaNo ratings yet
- High CarbonDocument2 pagesHigh CarbonKarisoNo ratings yet
- Ajr.09.2772 Grading Neuroforaminal StenosisDocument4 pagesAjr.09.2772 Grading Neuroforaminal StenosisOscar NogueraNo ratings yet
- Quarterly Progress Report FormatDocument7 pagesQuarterly Progress Report FormatDegnesh AssefaNo ratings yet
- Denagard-CTC US Knowledge ReportDocument4 pagesDenagard-CTC US Knowledge Reportnick224No ratings yet
- Module 2: Environmental Science: EcosystemDocument8 pagesModule 2: Environmental Science: EcosystemHanna Dia MalateNo ratings yet
- To 33B-1-1 01jan2013Document856 pagesTo 33B-1-1 01jan2013izmitlimonNo ratings yet
- Wa0016Document3 pagesWa0016Vinay DahiyaNo ratings yet
- Chapter 54 - Drugs Acting On The Upper Respiratory TractDocument13 pagesChapter 54 - Drugs Acting On The Upper Respiratory TractJonathonNo ratings yet
- UM-1D User ManualDocument30 pagesUM-1D User ManualAhmedBalaoutaNo ratings yet
- 5L ReductionsDocument20 pages5L ReductionsCarlos Javier Orellana OrtizNo ratings yet
- Assignment 2: Loan Submission For Equipment FinanceDocument6 pagesAssignment 2: Loan Submission For Equipment FinanceIT'S SIMPLENo ratings yet