Professional Documents
Culture Documents
GCP Training Manual
Uploaded by
patibautistaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
GCP Training Manual
Uploaded by
patibautistaCopyright:
Available Formats
TRAINING MANUAL
ICH GCP
EU Clinical Trial and GCP Directives
FDA CFR Title 21 Part 312
Background
CONTENTS
1. History of Clinical Trial Legislation
1.1 Code of Federal Regulations
1.2 Declaration of Helsinki
1.3 European GCP Guidelines
1.4 ICH
1.5 EU Directives
1.6 Regulatory Bodies
1.7 Summary
2. ICH GCP
2.1 Overview of ICH GCP
2.2 Roles and Responsibilities
2.3 IRB/IEC
2.4 Investigator
2.5 Sponsor
2.5.1 Monitor
2.6 Protocol and amendments
2.7 Investigator Brochure
2.8 Essential Documents
2.9 Ultimate responsibilities under ICH
3. Europe
3.1 EU Clinical Trials Directive
3.2 EU GCP Directive
3.3 GMP Directive
4. USA
4.1 FDA Code of Federal Regulations Title 21 Part 312
4.2 FDA 21 CFR Part 11
5. Self Assessments
5.1 ICH GCP Chapter 3: Ethics Committees
5.2 ICH GCP Chapter 4: Investigators
5.3 ICH GCP General
5.4 EU CT Directive
5.5 EU GCP Directive
5.6 FDA 21 CFR Part 312
5.7 Case Study model answer
3.4. GMP Directive and Annexe 13
At this stage it is important that you are of the existence of these documents, and
the fact that the manufacture, shipping, storage, dispensing, return and destruction
of Investigational Medicinal Product (IMP) is subject to strict control. For every
clinical trial there should be detailed procedures for all of these steps and you
should follow closely any instructions you are given.
3.5. EU Guidelines and Recommendations
There are also many guidelines and recommendations which supplement the
directives and these can be accessed via Eudralex Volume 10. New guidelines and
recommendations are being issued on a regular basis so it is important to check
regularly what the latest requirements are.
Finally another reminder that EU legislation is being revised and the new legislation
is likely to come into force in 2016.
5. SELF ASSESSMENT
5.1 ICH GCP Chapter 3
1. How often should an Ethics Committee review an on going clinical trial?
A At least once per year
B At the beginning
C At the beginning and the end
D Every 6 months
2. How many members should an Ethics Committee have?
A At least 3
B At least 5
C At least 7
D There is no specification
3. How long should Ethics Committees keep records for a clinical trial?
A 2 years after last marketing authorisation
B 3 years after end of clinical trial
C 5 years after end of clinical trial
D 15 years after end of clinical trial
4. With which of the following should Ethics Committees comply?
A SOPs, regulatory requirements and the protocol
B SOPs and the protocol
C Regulatory requirements and the protocol
D SOPs and regulatory requirements
5. What role can the investigator play in the Ethics Committee review of a study?
A None- they cant attend
B They can give information and vote
C They can give information but may not vote
D They can vote, but cant give any further information about the study
Answers: A, B, B, D, C
5.2 ICH GCP Chapter 4
1. With which of the following should Investigators comply?
A Sponsor SOPs, regulatory requirements and the protocol
B Sponsor SOPs and the protocol
C Regulatory requirements and the protocol
D Sponsor SOPs and regulatory requirements
2. Which of the following may be implemented WITHOUT prior approval by the
Ethics Committee?
A Deviation from the protocol to avoid immediate hazard to the subjects
B Minor changes to the Informed Consent Form
C Deviations from the protocol for practical reasons
D Protocol amendments
3. Which of the following does not appear in the list of information to be given to
subjects?
A Aspects of the trial which are experimental
B Payment to the investigator
C Compensation available in the event of a trial-related injury
D That records identifying the subject will be kept confidential
4. According to ICH GCP which of the following is NOT a requirement for
informed consent where the subject or their representative can read and
write?
A The subject should receive a copy of the consent form
B The subject or their legal representative should sign and personally date
the consent form
C It should be witnessed
D It should be obtained before the subject enters the study
5. Who is responsible for study drug at the site?
A The investigator/institution
B The pharmacist
C The sponsor
D The monitor
Answers: C, A, B, C, A
5.3 ICH GCP General
1. According to ICH GCP when, under normal circumstances, should the monitor visit
the site?
A They dont have to visit
B Before, during and after the study
C Every 4-6 weeks
D At Least once
2. According to chapter 8 of ICH GCP where should routine monitoring visit report be
filed?
A In the sponsor files, but not the investigator file
B In the sponsor files and the investigator files
C In the investigator files, but not the sponsor files
D It doesnt have to be kept
3. Which geographical regions are involved in ICH?
A US and Europe
B US, Europe and Australia
C US, Europe and Russia
D US, Europe and Japan
4. According to ICH GCP what is the most important consideration when conducting
clinical research?
A Quality of data
B Speed to market
C Protection of trial subjects
D Cost
5. Which responsibilities are covered under ICH GCP E6
A The Sponsor and the Investigator
B The investigator and the Ethics Committee
C The Sponsor, the Investigator and the Ethics Committee
D The Sponsor, the Investigator and the Regulatory Authority
Answers: B, A, D, C, C
5.4 EU CT Directive
1. According to the EU Clinical Trials Directive governing clinical trials what are the
timelines for a Clinical Trial Authorisation?
A 30 days
B 60 days
C 90 days
D 120 days
2. According to the EU CT Directive governing clinical trials what are the timelines for
an Ethics Committee Approval?
A 30 days
B 60 days
C 90 days
D 120 days
3. According to the EU CT Directive governing clinical trials what are the timelines for
Reporting Fatal and Life-threatening Suspected Unexpected Serious Adverse
Reactions (SUSARs) to the Competent Authority and Ethics Committee?
A Immediately
B 24 hours
C 7 days
D 15 days
4. According to the EU CT Directive governing clinical trials what are the timelines for
Reporting to the Regulatory Authority and the Ethics Committee that the study is
complete under normal circumstances?
A 15 days
B 30 days
C 60 days
D 90 days
5. According to the EU CT Directive governing clinical trials what are the timelines for
Reporting to the Regulatory Authority and the Ethics Committee that the study is
complete in the event of an early termination of a study?
A 15 days
B 30 days
C 60 days
D 90 days
Answers: B, B, C, D, A
5.5 EU GCP Directive
1. According to the EU GCP Directive how long should the Sponsor and
Investigator keep trial related documentation?
A 2 years after last marketing authorisation
B 3 years after end of clinical trial
C 5 years after end of clinical trial
D 15 years after end of clinical trial
2. Which version of the Declaration of Helsinki is referred to in the EU GCP
Directive?
A The version is not specified
B 1964
C 1996
D 2000
3. Who is responsible for ensuring the conduct of a clinical trial comples with
regulatory requirements if the sponsor delegates all of his trial-related functions
to a company?
A It is not specified
B The company they have delegated to
C They both have responsibility
D The sponsor remains responsible
4. Under what circumstances is manufacturing authorisation not required?
A It is always required
B When drug is being reconstituted prior to use or packaging in a hospital by a
pharmacist and used in that institution
C When drug is being imported from a non-EU country
D When the investigator is the sponsor
5. How often should the Investigators Brochure be validated and updated?
A At least once a year
B Every 2 years
C When new information becomes available
D There is no specification
Answers: C, C, D, "# $
5.6 FDA 21 CFR part 312
1. Under FDA regulations who is responsible for selecting monitors?
A The Investigator
B The Sponsor
C The IRB
D The FDA
2. What does IRB stand for?
A Investigational Review Board
B Investigational Research Board
C Institutional Review Board
D Investigational Review Board
3. Under FDA regulations how long does the Sponsor have to keep the clinical trial
records?
A 2 years after marketing authorisation of discontinuation of drug
B 3 years after end of clinical trial
C 5 years after end of clinical trial
D 15 years after end of clinical trial
4. How often does the Sponsor have to submit reports on study progress to the
FDA?
A At the end of the study
B Every 6 months
C Every 12 months
D Every 2 years
5. For how long after the end of the study does the investigator have to inform FDA
of changes in their financial disclosure information?
A They dont have to notify changes after the end of the study
B 1 year
C 2 years
D 5 years
Answers: B, C, A, C, B
5.7 Case Study Model Answer: Sponsor Responsibilities Exercise
In taking on the role of sponsor the investigator assumes a large amount of
responsibility, some of which can be costly and onerous.
Investigational Product: The pharmaceutical company would be responsible for
some aspects of the Investigational Product. This may include manufacturing,
packaging, labeling, randomization, blinding and coding of the product, although it
may be that the company are just providing bulk drug and the investigator is doing
the packaging, labeling and coding himself, in which case the pharmaceutical
company is only responsible for manufacture and shipping of the product. The
pharmaceutical company would also be responsible for providing and updating the
Investigator's Brochure. The investigator/sponsor would be responsible for the drug
at site, including drug storage, accountability and destruction. It would be important
that these responsibilities are clearly documented and that the investigator's role as
sponsor is also clearly documented.
Other Responsibilities: In this situation the pharmaceutical company would also
need to update the investigator if any new safety information comes to light but the
investigator takes on all other sponsor responsibilities including: Quality Assurance
and Quality Control; providing medical expertise; designing the trial using
appropriately qualified individuals (e.g. Statisticians etc.); trial management; data
handling; record keeping (both trial master file and investigator site file see ICH
GCP chapter 8); compensation; insurance and indemnity; finance; Regulatory
Authority approval; Ethics Committee approval; record access; keeping up to date
with safety information; reporting adverse reactions to the regulatory authority and
ethics committees; monitoring i.e. appointing someone to act as monitor for the
study ; audit the investigator might need to consider bringing in an auditor;
ensuring compliance with GCP, regulatory requirements and the protocol and also
dealing with any noncompliance; notifying ethics committees and regulatory
authorities if the trial ends early; and finally, writing the clinical trial report. It is also
important to remember that the investigator/sponsor would also have to undertake
all investigator responsibilities as defined in ICH GCP chapter 4.
You might also like
- Potential Interview QuestionsDocument0 pagesPotential Interview QuestionsRahul PuriNo ratings yet
- Self-Directed Certification Exam Review of GCP For Clinical Research Coordinators, Clinical Research Associates (Monitors) and Clinical InvestigatorsDocument6 pagesSelf-Directed Certification Exam Review of GCP For Clinical Research Coordinators, Clinical Research Associates (Monitors) and Clinical Investigatorsnarmi10No ratings yet
- Essential GCP by Professor David HutchinsonDocument64 pagesEssential GCP by Professor David HutchinsonhafizStudioNo ratings yet
- Introduction to Clinical Data ManagementDocument11 pagesIntroduction to Clinical Data ManagementPr Pa100% (1)
- 01 Introduction To GCPDocument22 pages01 Introduction To GCPMbellattiNo ratings yet
- Sop To Achieve GCP Clinical ResearchDocument195 pagesSop To Achieve GCP Clinical Researchشادي الاخرس100% (1)
- Konsep GCP Good Clinical PracticeDocument48 pagesKonsep GCP Good Clinical PracticeeuhsahaNo ratings yet
- Clinical Trial DocumentsDocument37 pagesClinical Trial Documentsapi-37446750% (1)
- FDA Guidelines For Clinical Trials PDFDocument2 pagesFDA Guidelines For Clinical Trials PDFStephenNo ratings yet
- Sample GCP ChecklistDocument8 pagesSample GCP Checklistsreeraj.guruvayoor100% (1)
- GCP Reference GuideDocument26 pagesGCP Reference GuidekhantstopmeNo ratings yet
- Breaking Down Barriers to EDCDocument26 pagesBreaking Down Barriers to EDCin_goodguyNo ratings yet
- Introduction to ICH-GCPDocument15 pagesIntroduction to ICH-GCPSwapnil BhowateNo ratings yet
- Basic Clinical Trial Terms Explained With PicturesDocument1 pageBasic Clinical Trial Terms Explained With PicturesJanelle Bowden100% (5)
- Clinical Data Management HuongDocument55 pagesClinical Data Management HuongAbhranAbpaucastNo ratings yet
- GCP Pocket GuideDocument26 pagesGCP Pocket GuideAman AmanNo ratings yet
- Tool Summary Sheet: Blue ItalicsDocument32 pagesTool Summary Sheet: Blue ItalicsAli FakihNo ratings yet
- Clinical Data Management (Presentation by Sarma)Document30 pagesClinical Data Management (Presentation by Sarma)T V S Sarma100% (40)
- By: Kris Traver and Nitin JainDocument14 pagesBy: Kris Traver and Nitin JainMahesh BhagwatNo ratings yet
- Clinical Data Management and E-Clinical Trials (IPS)Document22 pagesClinical Data Management and E-Clinical Trials (IPS)api-3842711100% (5)
- 05 Ich GCPDocument25 pages05 Ich GCPBhaskar Satya Sankar Balaji100% (1)
- Developing and Writing CRFDocument23 pagesDeveloping and Writing CRFsuri333No ratings yet
- Site FDA inspection checklistDocument9 pagesSite FDA inspection checklistsreeraj.guruvayoorNo ratings yet
- Handbook For GCPDocument132 pagesHandbook For GCPanotherlevel88No ratings yet
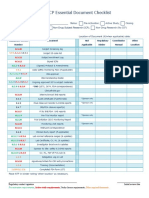
- ICH GCP Essential Document ChecklistDocument2 pagesICH GCP Essential Document ChecklistMohammed Yousffi50% (2)
- Essential Documents For The Conduct of A Clinical TrialDocument10 pagesEssential Documents For The Conduct of A Clinical TrialSandeep SinghalNo ratings yet
- Guidelines Phase1 Clinical TrialsDocument64 pagesGuidelines Phase1 Clinical TrialsJinnatNo ratings yet
- International Regulatory Requirements On Clinical Trails and Data ManagementDocument19 pagesInternational Regulatory Requirements On Clinical Trails and Data ManagementJay PraveenNo ratings yet
- Clinical Data+ManagementDocument352 pagesClinical Data+Managementpravin sNo ratings yet
- CDM Processes C1Document41 pagesCDM Processes C1api-3810976No ratings yet
- The Study Protocol Part TwoDocument12 pagesThe Study Protocol Part TwoGerman LambogliaNo ratings yet
- Clinical Research AssociateDocument2 pagesClinical Research AssociatepalkybdNo ratings yet
- Historical Perspective, Different Phases of Clinical TrialsDocument16 pagesHistorical Perspective, Different Phases of Clinical Trialsexcel proNo ratings yet
- Clinical Research Essentials QuizDocument5 pagesClinical Research Essentials Quizsufiya fatimaNo ratings yet
- CologyDocument7 pagesCologyvibhu yadav100% (1)
- Good Clinical PracticeDocument21 pagesGood Clinical PracticeanisaishakNo ratings yet
- Model Question Paper Class RoomDocument16 pagesModel Question Paper Class Roomunknowncodex0xNo ratings yet
- Linne Ringsruds Clinical Laboratory Science 7th Edition Turgeon Test BankDocument25 pagesLinne Ringsruds Clinical Laboratory Science 7th Edition Turgeon Test BankMorganLoganposxg100% (50)
- DCS CR Final Exam Question FileDocument23 pagesDCS CR Final Exam Question FileAnish RedkarNo ratings yet
- Linne Ringsruds Clinical Laboratory Science 7th Edition Turgeon Test BankDocument35 pagesLinne Ringsruds Clinical Laboratory Science 7th Edition Turgeon Test Bankjerrybriggs7d5t0v100% (18)
- Ethics GuidelinesDocument5 pagesEthics GuidelinesSirgangaramhospital HospitalNo ratings yet
- Section 12Document28 pagesSection 12heartNo ratings yet
- Good Clinical Practice 1Document4 pagesGood Clinical Practice 1CHRISTINA L WAGHANo ratings yet
- RAC Past PapersDocument6 pagesRAC Past PapersOlivia Merchant0% (2)
- Global Regulations in Clinical Trials by N.srinivas ICRIDocument62 pagesGlobal Regulations in Clinical Trials by N.srinivas ICRIravi9247No ratings yet
- CDoc - Practice Questions For Final Year Sem 8 Regular Batch 2019-20Document55 pagesCDoc - Practice Questions For Final Year Sem 8 Regular Batch 2019-20MODI ACADEMYNo ratings yet
- Dwnload Full Linne Ringsruds Clinical Laboratory Science 7th Edition Turgeon Test Bank PDFDocument35 pagesDwnload Full Linne Ringsruds Clinical Laboratory Science 7th Edition Turgeon Test Bank PDFdanagarzad90y100% (11)
- Schedule YDocument55 pagesSchedule YshilpapillaiNo ratings yet
- Question BankDocument5 pagesQuestion BankUmesh ChikhlikarNo ratings yet
- NDA ProcessDocument3 pagesNDA Processdustymarie100% (2)
- Questionnaire (HTMLE)Document16 pagesQuestionnaire (HTMLE)Angelo Mercede100% (1)
- Introduction To Investigators Responsibilities With Good Clinical PracticeDocument16 pagesIntroduction To Investigators Responsibilities With Good Clinical PracticeLuz Estefany Huaman MachacaNo ratings yet
- Investigators Responsibilities With GCPDocument16 pagesInvestigators Responsibilities With GCPLlosa JuneNo ratings yet
- M. Pharm II sem Clinical trials and PV assignmentDocument4 pagesM. Pharm II sem Clinical trials and PV assignmentAkhil BhatnagarNo ratings yet
- Good Clinical Practice Guidelines IndiaDocument4 pagesGood Clinical Practice Guidelines IndiaMonicaNo ratings yet
- SGB Amravati University B.Pharm Pharmacovigilance Question BankDocument10 pagesSGB Amravati University B.Pharm Pharmacovigilance Question BankTabassum PopatpotraNo ratings yet
- Pharmabizz QADocument15 pagesPharmabizz QArama_v100% (1)
- 9 - DR Arun Bhatt - Schedule YDocument27 pages9 - DR Arun Bhatt - Schedule Yvivek100% (1)
- Rev GCP Goals Principles Roles Resp Lepay Toth-Allen FDADocument37 pagesRev GCP Goals Principles Roles Resp Lepay Toth-Allen FDASuhaimi JaaffarNo ratings yet
- Schedule y PPT EDITTED ONEDocument38 pagesSchedule y PPT EDITTED ONEKesetha100% (2)
- Good Documentation PracticesDocument34 pagesGood Documentation PracticesSophia100% (8)
- Regulatory Perspective: Data Integrity Guidance/Policy: PDA Data Integrity Workshop September 14, 2016 Washington, D.CDocument20 pagesRegulatory Perspective: Data Integrity Guidance/Policy: PDA Data Integrity Workshop September 14, 2016 Washington, D.CCharles García SanchezNo ratings yet
- Food Safety Assignment XBFS4103 (2) .EditedDocument12 pagesFood Safety Assignment XBFS4103 (2) .EditedMeha Raj100% (1)
- Missionpharma Zambia Brochure (38412)Document13 pagesMissionpharma Zambia Brochure (38412)Patrick “Oposche” OwinoNo ratings yet
- Inspection of Quality Control LaboratoriesDocument18 pagesInspection of Quality Control LaboratoriesschumonNo ratings yet
- PHSS Control Strategy White PaperDocument13 pagesPHSS Control Strategy White PaperAkuWilliams100% (1)
- Pharmaceutical Quality Compliance Manager in NJ Resume Mark SakitisDocument3 pagesPharmaceutical Quality Compliance Manager in NJ Resume Mark SakitisMarkSakitisNo ratings yet
- Audit Report EXAMPLE 1Document3 pagesAudit Report EXAMPLE 1Thomas G. NimmerNo ratings yet
- PESSI Tenders Medicines Interferon SyringesDocument77 pagesPESSI Tenders Medicines Interferon SyringesAsim IdreesNo ratings yet
- Report On Beximco Pharma: Course: Training and Development - Course Code: HRM 340 Section: 3 Team: Cross TrainerDocument25 pagesReport On Beximco Pharma: Course: Training and Development - Course Code: HRM 340 Section: 3 Team: Cross TrainerValakNo ratings yet
- FDA与ISPE关于质量量度的试点计划Document14 pagesFDA与ISPE关于质量量度的试点计划windli2014No ratings yet
- Circular 16 2023 TT BYTDocument31 pagesCircular 16 2023 TT BYTDinh NgocNo ratings yet
- Market Expansion of Opsonin PharmaDocument35 pagesMarket Expansion of Opsonin PharmaJahidul karimNo ratings yet
- Good Hygiene Practices GHPDocument3 pagesGood Hygiene Practices GHPStanley50% (2)
- Who-Public-Consultation Cgtp-White-Paper 16 Dec 2021Document22 pagesWho-Public-Consultation Cgtp-White-Paper 16 Dec 2021bioNo ratings yet
- Validation of Sterilizing Grade Filters Bacterial Challenge TestsDocument52 pagesValidation of Sterilizing Grade Filters Bacterial Challenge TestsAjay KumarNo ratings yet
- Ombination Roducts: I CGMP RDocument6 pagesOmbination Roducts: I CGMP Rvijayns_250355172No ratings yet
- Republic of The Philippines Elliptical Road, Diliman, Quezon City, 1100Document10 pagesRepublic of The Philippines Elliptical Road, Diliman, Quezon City, 1100Vincent BautistaNo ratings yet
- SCH-M Inspection ChecklistDocument16 pagesSCH-M Inspection Checklistlalit4u78No ratings yet
- Analytical Control Strategies of VaccineDocument20 pagesAnalytical Control Strategies of VaccineDimitris PapamatthaiakisNo ratings yet
- VMP TheoryDocument34 pagesVMP Theoryparam540No ratings yet
- Guidance for Drugs in Clinical TrialsDocument25 pagesGuidance for Drugs in Clinical TrialsEve TaypeNo ratings yet
- Quality ManagementDocument20 pagesQuality ManagementChakshuBehl100% (1)
- LC Firmware Validation DeclarationDocument2 pagesLC Firmware Validation DeclarationJonathanCubillosSerratoNo ratings yet
- INVESTIGATION PROCESS IN DEVIATION MANAGEMENTDocument48 pagesINVESTIGATION PROCESS IN DEVIATION MANAGEMENThenrykayode4100% (1)
- GMP Guild For Cosmetic IngredientDocument48 pagesGMP Guild For Cosmetic IngredientLennon Tan Qin JiNo ratings yet
- SAP CFR Part11Document62 pagesSAP CFR Part11Seha Gulbaba0% (1)
- Guide to Pharmaceutical Process ValidationDocument13 pagesGuide to Pharmaceutical Process Validationran_ooNo ratings yet
- Fall 02Document67 pagesFall 02Vinay KutreNo ratings yet
- CGMP Regulations of Sterile ProductsDocument33 pagesCGMP Regulations of Sterile ProductsSukesh Potla75% (4)