Professional Documents
Culture Documents
Anthem Dental Enrollment Enrollment Form 2014
Uploaded by
Tanveer Shaikh0 ratings0% found this document useful (0 votes)
19 views2 pagesANTHEM is a registered trademark of ANTHEM Insurance Companies, Inc. The Blue Cross name and symbol are registered marks of The Blue Cross association.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentANTHEM is a registered trademark of ANTHEM Insurance Companies, Inc. The Blue Cross name and symbol are registered marks of The Blue Cross association.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
19 views2 pagesAnthem Dental Enrollment Enrollment Form 2014
Uploaded by
Tanveer ShaikhANTHEM is a registered trademark of ANTHEM Insurance Companies, Inc. The Blue Cross name and symbol are registered marks of The Blue Cross association.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
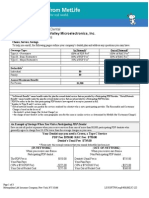
Anthem Blue Cross Life and Health Insurance Company is an independent licensee of the Blue Cross Association.
ANTHEM is a registered trademark of
Anthem Insurance Companies, Inc. The Blue Cross name and symbol are registered marks of the Blue Cross Association.
09-04114.05 E801 CA 04/29/2011
Anthem
Dental Enrollment Department
PO Box 1193
Minneapolis MN 55440-1193
PART A EMPLOYEE INFORMATION Employee complete Parts A thru D and return form to benefit administrator.
Employees
Last First Middle Initial
Name:
Social Security Number
/ /
Gender:
Male Female
Marital
Single Married Widowed Divorced Legally Separated
Status:
Date of Birth (Month-Day-Year)
/ /
Employees
Address
Home Phone Number Work Phone Number
Address:
City State Zip Code
PART B ENROLLMENT INFORMATION - Select Coverage Type (Check One Box Only):
Employee Only* Family
Employee and Spouse No Coverage * If waiving coverage for employee and/or any
Employee and Dependent Child(ren) eligible family members, you must complete Part D.
PART C DEPENDENT INFORMATION
Relationship
To Employee
First Name, Middle Initial, Last Name
(Include Last Name Only if Different From Employees)
Gender
Date of Birth
Month/Day/Year
Full Time
Student?
Unmarried?
Spouse M F / /
Dependent Child M F / / Y N Y N
Dependent Child M F / / Y N Y N
Dependent Child M F / / Y N Y N
PART D EMPLOYEE SIGNATURE Select One
Do you (the employee) have other dental coverage? Yes No Do your dependents have other dental coverage? Yes No
Name of Carrier: ___________________________________ Policy/Identification Number: ______________________________
I waive coverage for myself and/or my dependents and understand that by waiving coverage, whether entirely or partially paid by my
employer, that I waive the right to change this selection unless permitted in the group contracts participation requirements and enrollment
restrictions. Anthem Blue Cross reserves the right to decline any further dental enrollment changes.
Employee Signature: Date:
I am enrolling myself and/or my dependents and authorize payroll deductions, if applicable. I have read, or have had read to me, the
completed application and I realize that any false statement or misrepresentation in the application may result in a loss of coverage under
the policy. Refer to Note back of form for additional information. Employee Signature: Date:
PART E GROUP ENROLLMENT I NFORMATI ON - THI S PART TO BE COMPLETED BY EMPLOYER
New Group
Hire Date: _______/________/________
Prior Coverage Start Date (if applicable): ________/________/________
Coverage Effective Date: ________/________/________
Rehire Date Lay Off Began: ________/________/_______
Date Rehired: ________/________/_______
Return from Leave of Absence
Date Leave Began: ________/________/________
Date Returned to Work: ________/________/________ Existing Anthem Dental Group
Hire Date: _______/________/________
Prior Coverage Start Date (if applicable): ________/________/________
Coverage Effective Date: ________/________/________
Employee Change Part Time to Full Time
Date of Status Change: ________ /________/________
Effective Date: ________ /________/________
New Hire Apply Probationary Period (if
applicable) to determine Effective Date
Hire Date: __________ /______/_______
Effective Date:______ /_______/_______
Open Enrollment
Effective Date:
______ /_______/_______
Previously Waived Coverage or Loss of Coverage
Qualifying Event Reason:_________________________________
Hire Date: _____________ /_______/________
Event Date: ___________ /_______/________
Effective Date: ________ /_______/________
Group Name: Group & Subgroup Numbers:
Group Representatives Signature: Date: Phone Number: ( )
Dent al Member shi p Enr ol l ment For m
Notes to Employee:
California law prohibits an HIV test from being required or used by health insurance companies as a condition of
obtaining health insurance coverage.
REQUIREMENT FOR BINDING ARBITRATION The following provision does not apply to class actions: IF YOU ARE
APPLYING FOR COVERAGE, PLEASE NOTE THAT ANTHEM BLUE CROSS AND ANTHEM BLUE CROSS LIFE AND
HEALTH INSURANCE COMPANY REQUIRE BINDING ARBITRATION TO SETTLE ALL DISPUTES INCLUDING BUT
NOT LIMITED TO DISPUTES RELATING TO THE DELIVERY OF SERVICE UNDER THE PLAN/POLICY OR ANY
OTHER ISSUES RELATED TO THE PLAN/POLICY AND CLAIMS OF MEDICAL MALPRACTICE, IF THE AMOUNT IN
DISPUTE EXCEEDS THE JURISDICTIONAL LIMIT OF SMALL CLAIMS COURT. It is understood that any dispute
including disputes relating to the delivery of services under the plan/policy or any other issues related to the plan/policy,
including any dispute as to medical malpractice, that is as to whether any medical services rendered under this contract
were unnecessary or unauthorized or were improperly, negligently or incompetently rendered, will be determined by
submission to arbitration as provided by California law, and not by a lawsuit or resort to court process except as
California law provides for judicial review of arbitration proceedings. Both parties to this contract, by entering into it, are
giving up their constitutional right to have any such dispute decided in a court of law before a jury, and instead are
accepting the use of arbitration. THIS MEANS THAT YOU AND ANTHEM BLUE CROSS AND/OR ANTHEM BLUE
CROSS LIFE AND HEALTH INSURANCE COMPANY ARE WAIVING THE RIGHT TO A JURY TRIAL FOR BOTH
MEDICAL MALPRACTICE CLAIMS, AND ANY OTHER DISPUTES INCLUDING DISPUTES RELATING TO THE
DELIVERY OF SERVICE UNDER THE PLAN/POLICY OR ANY OTHER ISSUES RELATED TO THE PLAN/POLICY.
Empl oyer I nst r uc t i ons
Review Parts A, B, C, and D to be sure all information is complete, accurate and legible.
For risk groups, please disregard Full-time Student and Unmarried sections in Part C. This information does
not need to be completed.
When reporting effective dates use contractual start and stop guidelines as defined in your contract (i.e., first
of month, end of month, or actual dates).
Employer Complete Part: E - Group Enrollment Information
Check one reason for enrollment and provide requested information including coverage effective dates.
New Group New customer initial employee enrollment. Complete the Prior Coverage Start Date if your
plan benefits include waiting periods and credit for prior creditable coverage applies.
Existing Dental Group Enrolling additional employees from an acquisition/merger who were not
previously offered/enrolled in your dental plan. Complete the Prior Coverage Start Date only if your plan
benefits include waiting periods and credit for prior creditable coverage applies.
New Hire Enroll newly hired employee. If a probationary period applies, the coverage effective date is
after the probationary period.
Open Enrollment An employee is enrolling during groups open enrollment period.
Rehire A former employee was rehired.
Return From Leave of Absence An employee is returning from leave of absence.
Employee Status Change The employees employment status changed and the employee is now eligible
for dental benefits.
Previously Waived Coverage or Loss of Coverage If an employee waives coverage; he/she can only
enroll at a later date if the group contract includes an Open Enrollment period or if the individual has a loss
of other insurance coverage. If an employee or dependent involuntarily losses coverage and are now
eligible to enroll, complete this section.
Group Name Provide group name as listed in your contract.
Group and Subgroup Number Provide applicable numbers for individual employee.
Group Representative Sign, date, and provide your phone number.
Send Completed Forms To:
Anthem
Attn: Dental Enrollment Department
PO Box 1193
Minneapolis MN 55440-1193
You might also like
- Blue Shield CA Employee Enrollment Template v20160101Document8 pagesBlue Shield CA Employee Enrollment Template v20160101Anonymous RLktVcNo ratings yet
- 48 ReservoirDocument5 pages48 Reservoirapi-68594053No ratings yet
- 8 Margauxs Way #8, Norfolk, MA 02056 - MLS# 71652630 - RedfinDocument7 pages8 Margauxs Way #8, Norfolk, MA 02056 - MLS# 71652630 - Redfinashes_xNo ratings yet
- 366 Page ST AvonDocument14 pages366 Page ST AvonyukiNo ratings yet
- Metlife - Dental Ppo 12 15Document3 pagesMetlife - Dental Ppo 12 15api-252555369No ratings yet
- Insurance ID Card and Important Information: Aravind Reddy Patlolla 399 Graphic BLVD New Milford, NJ 07646Document1 pageInsurance ID Card and Important Information: Aravind Reddy Patlolla 399 Graphic BLVD New Milford, NJ 07646Aravind ReddyNo ratings yet
- Lloyds of LondonDocument4 pagesLloyds of LondonVinayak NarichaniaNo ratings yet
- Cigna Global GOP ProviderDocument2 pagesCigna Global GOP ProviderRoyer HyacintheNo ratings yet
- Liberty Mutual FormsDocument3 pagesLiberty Mutual FormsdadavemysterNo ratings yet
- Healthcare - Gov/sbc-Glossary: Important Questions Answers Why This MattersDocument10 pagesHealthcare - Gov/sbc-Glossary: Important Questions Answers Why This MattersQFQEWFWQEFwqNo ratings yet
- Tax Invoice: Charge DetailsDocument3 pagesTax Invoice: Charge DetailsRohit SharmaNo ratings yet
- IDS 2013 RecapDocument28 pagesIDS 2013 RecapDiaa Eldin SaadNo ratings yet
- Complete With DocuSign App2515089pdf QuotepdDocument8 pagesComplete With DocuSign App2515089pdf QuotepdSilvia GloverNo ratings yet
- Anshul Kirti: 839 N Marshall STDocument1 pageAnshul Kirti: 839 N Marshall STAnshul KirtiNo ratings yet
- MorningStar ES0143416115Document4 pagesMorningStar ES0143416115José J. Ruiz SorianoNo ratings yet
- Cna Liscense NumberDocument2 pagesCna Liscense Numberapi-548066065No ratings yet
- You Can Get This Information in Large Print and Braille. Call 1-800-841-2900 From Monday ToDocument6 pagesYou Can Get This Information in Large Print and Braille. Call 1-800-841-2900 From Monday ToAbhishek MeeNo ratings yet
- Healthcare - Gov/sbc-Glossary: Important Questions Answers Why This MattersDocument8 pagesHealthcare - Gov/sbc-Glossary: Important Questions Answers Why This Mattersapi-252555369No ratings yet
- Your Automatic Payments Schedule: PO Box 3199 Winston Salem, NC 27102-3199Document4 pagesYour Automatic Payments Schedule: PO Box 3199 Winston Salem, NC 27102-3199Yenny VidalNo ratings yet
- GetR229Form PDFDocument3 pagesGetR229Form PDFGerson RegisNo ratings yet
- LucidChart MarzoDocument2 pagesLucidChart MarzoHenry M Gutièrrez SNo ratings yet
- Action Required - Dairyland® Insurance Policy 11408173515 For LUIS LANDAETA WETTELDocument5 pagesAction Required - Dairyland® Insurance Policy 11408173515 For LUIS LANDAETA WETTELJulu EmimaryNo ratings yet
- Action Required:: Contact UsDocument2 pagesAction Required:: Contact UsHuy LeNo ratings yet
- Receipt PDFDocument2 pagesReceipt PDFPramod ChavanNo ratings yet
- Câmbio Atividade 12b Esther-OliveiraDocument3 pagesCâmbio Atividade 12b Esther-OliveiraSabine PessanNo ratings yet
- KeyBank Rollover FormDocument1 pageKeyBank Rollover FormmicheleNo ratings yet
- PDFDocument2 pagesPDFAjay vermaNo ratings yet
- Providers - Blue Shield Promise Health Plan PDFDocument3 pagesProviders - Blue Shield Promise Health Plan PDFMohamed ElmallahNo ratings yet
- 5Document10 pages5John C. LewisNo ratings yet
- Alvarado, Sandra E: SubscriberDocument3 pagesAlvarado, Sandra E: SubscriberJohn LarbieNo ratings yet
- Healthcare - Gov/sbc-Glossary: Important Questions Answers Why This MattersDocument9 pagesHealthcare - Gov/sbc-Glossary: Important Questions Answers Why This Mattersapi-252555369No ratings yet
- DWS NEWS RELEASE - Unemployment Insurance Claims Report (1.7)Document2 pagesDWS NEWS RELEASE - Unemployment Insurance Claims Report (1.7)Jennifer WeaverNo ratings yet
- StabilityDocument3 pagesStabilitykinsonprabuNo ratings yet
- INsuranceDocument26 pagesINsuranceBhavaniNo ratings yet
- CignaDocument7 pagesCignaUNKNOWN LSANo ratings yet
- GPDocument3 pagesGPHarshitNo ratings yet
- Department of Workforce ServicesDocument1 pageDepartment of Workforce ServicesJonna CaballeroNo ratings yet
- Farmers Auto OnDemand R123Document2 pagesFarmers Auto OnDemand R123luisalcantara12345678No ratings yet
- 2019-2020 Full PPO 0 Deductible SBC PDFDocument9 pages2019-2020 Full PPO 0 Deductible SBC PDFrgbrbNo ratings yet
- Seven Generations Energy LTD.: Canada ResearchDocument27 pagesSeven Generations Energy LTD.: Canada ResearchAnonymous m3c6M1No ratings yet
- Blue Shield of California Shield Savings Plans A36813 2011Document2 pagesBlue Shield of California Shield Savings Plans A36813 2011DennisNo ratings yet
- Invoice - Zoya Ali Traders LLC 2023-02-02Document2 pagesInvoice - Zoya Ali Traders LLC 2023-02-02Bahar AliNo ratings yet
- Dept. of Health Wellspan Death ReportDocument44 pagesDept. of Health Wellspan Death ReportAnonymous nhLKKmcDNo ratings yet
- PENNDOT BOP Strike Off LetterDocument6 pagesPENNDOT BOP Strike Off LetterbcgpNo ratings yet
- Account Settings ComEd - An Exelon Company PDFDocument1 pageAccount Settings ComEd - An Exelon Company PDFLola100% (1)
- Payslip To Print 04 29 2017 PDFDocument1 pagePayslip To Print 04 29 2017 PDFDoraNo ratings yet
- Application For Ignition Interlock License/Return of Regular Driver LicenseDocument2 pagesApplication For Ignition Interlock License/Return of Regular Driver LicenseLee KellyNo ratings yet
- Order HistoryDocument1 pageOrder HistoryTrenton DunstanNo ratings yet
- Tax Information Account 943420759Document12 pagesTax Information Account 943420759DavidNo ratings yet
- Os SS 27Document1 pageOs SS 27Nard CruzNo ratings yet
- Classy Glass Inc Policy Package HighlightedDocument90 pagesClassy Glass Inc Policy Package HighlightedTMJ4 NewsNo ratings yet
- 2017 Toyota Camry Le Se Xle XseDocument4 pages2017 Toyota Camry Le Se Xle XseGeorge ZabarasNo ratings yet
- NYC - TLC - Driver ApplicationDocument5 pagesNYC - TLC - Driver ApplicationMahid SamadNo ratings yet
- Disconnect Notice: HgehgeffhhgeefehhfhfeggeehfhghghheffegeeefgggggggfhefgfefhgfghgggDocument3 pagesDisconnect Notice: HgehgeffhhgeefehhfhfeggeehfhghghheffegeeefgggggggfhefgfefhgfghgggDaniel GonzalesNo ratings yet
- Welcome To Blue Cross and Blue Shield of Illinois and Fort Dearborn LifeDocument6 pagesWelcome To Blue Cross and Blue Shield of Illinois and Fort Dearborn LifeBuy BaNo ratings yet
- Official Seal or Stamp of Service/Employing Agency (If None, ADocument2 pagesOfficial Seal or Stamp of Service/Employing Agency (If None, Aมดน้อย ผู้น่ารักNo ratings yet
- Employee Enrollment Application: Group Size 51+ Eligible Employees - Medically UnderwrittenDocument6 pagesEmployee Enrollment Application: Group Size 51+ Eligible Employees - Medically Underwrittenmdugan5026No ratings yet
- Anthem Blue Cross Medical Enrollment Form 2014Document4 pagesAnthem Blue Cross Medical Enrollment Form 2014Tanveer ShaikhNo ratings yet
- Employees Retirement System of Texas Texas Employees Group Benefits Program (GBP) Evidence of Insurability (EOI) Application Active/Retired EmployeesDocument5 pagesEmployees Retirement System of Texas Texas Employees Group Benefits Program (GBP) Evidence of Insurability (EOI) Application Active/Retired EmployeesCarroll MixsonNo ratings yet
- How to Enroll in Medicare Health Insurance: Choose a Medicare Part D Drug Plan and a Medicare Supplement PlanFrom EverandHow to Enroll in Medicare Health Insurance: Choose a Medicare Part D Drug Plan and a Medicare Supplement PlanNo ratings yet
- Anthem Blue Cross Medical Enrollment Form 2014Document4 pagesAnthem Blue Cross Medical Enrollment Form 2014Tanveer ShaikhNo ratings yet
- Retail L0Document57 pagesRetail L0Tanveer ShaikhNo ratings yet
- INFA Cloud Integration Editions ComparisonDocument2 pagesINFA Cloud Integration Editions ComparisonTanveer ShaikhNo ratings yet
- Teradata Bteq UtilityDocument29 pagesTeradata Bteq UtilityjennamanniNo ratings yet
- Chukwuemeka ElukaDocument6 pagesChukwuemeka ElukaTanveer ShaikhNo ratings yet
- SQLDocument11 pagesSQLRaj KumarNo ratings yet
- Getting Away With Murder by Robert James BidinottoDocument4 pagesGetting Away With Murder by Robert James BidinottoЕкатерина ИвановнаNo ratings yet
- Ebralinag Case, DigestDocument2 pagesEbralinag Case, Digestoihah100% (1)
- Mendoza vs. SorianoDocument10 pagesMendoza vs. SorianoDeb BieNo ratings yet
- Philippine Veterans Bank Employees Union-NUBE Vs - Philippine Veterans BankDocument1 pagePhilippine Veterans Bank Employees Union-NUBE Vs - Philippine Veterans BankErika Mariz CunananNo ratings yet
- United States v. Maestas, 642 F.3d 1315, 10th Cir. (2011)Document17 pagesUnited States v. Maestas, 642 F.3d 1315, 10th Cir. (2011)Scribd Government DocsNo ratings yet
- Uruguayans of To Day - William Belmont PDFDocument790 pagesUruguayans of To Day - William Belmont PDFSoledad RodriguezNo ratings yet
- Sanlakas vs. Executive Secretary Reyes (GR 159085, 3 February 2004)Document3 pagesSanlakas vs. Executive Secretary Reyes (GR 159085, 3 February 2004)adobopinikpikan100% (1)
- Herminio Perez Adames v. Joseph A. Califano, JR., Secretary of Health, Education and Welfare, 552 F.2d 1, 1st Cir. (1977)Document2 pagesHerminio Perez Adames v. Joseph A. Califano, JR., Secretary of Health, Education and Welfare, 552 F.2d 1, 1st Cir. (1977)Scribd Government DocsNo ratings yet
- Decidendi Is The Legal Resonning Behind A Judge's Decision and Is Binding OnDocument3 pagesDecidendi Is The Legal Resonning Behind A Judge's Decision and Is Binding OnKevin Chai Jin Chern100% (1)
- Norwex Et. Al. v. SweportsDocument6 pagesNorwex Et. Al. v. SweportsPriorSmartNo ratings yet
- Statcon AssignmentDocument2 pagesStatcon AssignmentJuris Mendoza100% (1)
- R V Hinks House of Lords 26th October 2006Document25 pagesR V Hinks House of Lords 26th October 2006Eric TittoNo ratings yet
- List of Cases in CrimLaw IDocument2 pagesList of Cases in CrimLaw ILenz Meret CataquisNo ratings yet
- Chavez V JBC DigestDocument2 pagesChavez V JBC DigestJanine OlivaNo ratings yet
- Syllabus ClaridadesDocument12 pagesSyllabus ClaridadesIsmael ManaligodNo ratings yet
- Davao Light v. OpenaDocument22 pagesDavao Light v. OpenaMari DesNo ratings yet
- Petition For Change of Trial Venue - AmpatuanDocument1 pagePetition For Change of Trial Venue - AmpatuanAlexis Dominic San Valentin100% (1)
- CPC Course Outline Yuvraj ParekhDocument3 pagesCPC Course Outline Yuvraj ParekhShashwat DroliaNo ratings yet
- Carbonell vs. CADocument2 pagesCarbonell vs. CACharmila SiplonNo ratings yet
- De Bisschop Vs GalangDocument2 pagesDe Bisschop Vs GalangtinctNo ratings yet
- Fabian vs. DesiertoDocument2 pagesFabian vs. DesiertoMang Jose100% (1)
- NFSW V OvejeraDocument23 pagesNFSW V OvejeraemmanuelcaddaliNo ratings yet
- 01 Alunan v. VelosoDocument4 pages01 Alunan v. VelosogabbyborNo ratings yet
- Gutierrez V CollectorDocument3 pagesGutierrez V Collectormichee coi100% (1)
- Missouri Courts Appellate PracticeDocument27 pagesMissouri Courts Appellate PracticeGeneNo ratings yet
- United States v. Frank Chappell, 3rd Cir. (2011)Document5 pagesUnited States v. Frank Chappell, 3rd Cir. (2011)Scribd Government DocsNo ratings yet
- Confessions Made To Police Office Under Section 25Document26 pagesConfessions Made To Police Office Under Section 25Soumya SinhaNo ratings yet
- Compilation For FinalsDocument25 pagesCompilation For FinalsIrish AnnNo ratings yet
- Public Premises ActDocument48 pagesPublic Premises ActNandini TarwayNo ratings yet
- Enforcement of Foreign JudgementsDocument17 pagesEnforcement of Foreign JudgementsDhriti SharmaNo ratings yet