Professional Documents
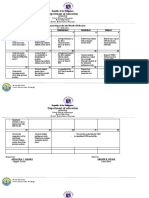
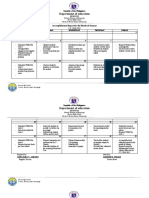
Culture Documents
All About Our Kidneys
Uploaded by
Liezl SabadoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
All About Our Kidneys
Uploaded by
Liezl SabadoCopyright:
Available Formats
ALL ABOUT OUR KIDNEYS
Useful links: Life with a single kidney and How to look after your kidneys
We can live quite well with only one kidney and some people live a healthy life even though born
with one missing. But while bones can break, muscles can waste away and the brain can sleep
without risk to life, if both of your kidneys fail, as happens in end stage kidney failure, bone, muscle
or brain can not carry on.
How do our kidneys work?
Think of your kidneys as an extremely sophisticated, waste disposal system, which sorts non-
recyclable waste from recyclable waste, 24 hours a day, 7 days a week, while also cleaning your
blood. Much of this waste is produced by the body as it processes the food you eat.
KidneyEd TV
Our video collections of videos on YouTube, which have been grouped into playlists, to learn more
about the kidneys and the urinary system and other related topics. Start with the video below and
later you can view a wide range of reviewed kidney health education videos on our
profile KidneyHealthAus - on YouTube.
Without any kidney function our body dies. Some kidney function is essential for life!
Most people are born with two kidneys, each one about the size of an adult fist, are bean-shaped and weigh around 150 grams
each. The kidneys are located at both sides of your backbone just under the rib cage or above the small of your back. They are
protected from injury by a large padding of fat, your lower ribs and several muscles.
What do your kidneys do?
Our kidneys are small biological marvels with a fascinating design. Healthy kidneys act like a filter to make sure the right amount
of wastes and fluids are removed. Every hour your blood supply circulates through the kidneys about 12 times. Each day your
kidneys process around 200 litres of blood, with around 1 to 2 litres of waste leaving the body as urine. Our kidneys make three
important hormones, erythropoietin, renin and active vitamin D. Erythropoietin stimulates the production of red blood cells, renin
is involved in the control of blood pressure and active vitamin D controls calcium uptake and helps make strong bones.
What is the role of your kidneys in keeping you healthy?
For organs so small, your kidneys works hard - they have a number of vital roles to play in the daily functions of our body, as
they:
act as filters for your body to clean blood of wastes, yet retain essential elements needed by the body
they keep the proper balance of salts and acids in the body, and produce hormones and enzymes which help to:
control your blood pressure
help to keep your internal water balance
make red blood cells and help maintain your blood composition and pH levels
maintain strong and healthy bones and help to keep mineral balance
Your kidneys are master chemists of the body, intervene in many processes and balances in the body and control many vital
body functions. The major role of the kidneys is to remove waste from the blood and eliminate it in the urine. To remove this
waste and extra water, blood enters the kidney through the renal artery; blood is then cleaned in the kidney as it passes through
tiny filters called nephrons. The nephrons are the basic working units of the kidneys, controlling the formation of urine. One
kidney contains about one million nephrons, and each nephron contains a filtering apparatus called a glomerulus.
Anatomy of the kidneys
We have about a million hairpin-like glomeruli at birth, but lose about 100,000 of these every decade of life. Droplets of filtered
blood pass through a number of tubules (tiny tubes) into the medulla, a central collecting region. The glomeruli and tubules
together make up nephrons, long and extremely fine tubes which, if connected, would run for 80 kilometres (50 miles).
Cleaned blood returns to the body by the renal vein. Waste and extra water removed by the kidney passes through a tube called
the ureter to the bladder, where it is stored as urine or wee. When the bladder is full, urine passes out of the body through
another tube called the urethra.
The process of removing waste and extra water in simple terms is:
food and drink enters the stomach and are broken down into nutrients
solid waste products are removed and nutrients enter the bloodstream.
nutrients are used by the body for energy, growth, repair and maintenance of body functions.
this process creates waste which is removed by the kidneys.
extra nutrients not immediately needed by the body are also removed by the kidneys.
waste products and extra water move from the kidneys to the bladder, then leave the body as urine
The kidneys are designed to last a life-time. They do an amazing job! It is important to care for them.
We recommend these kidney education tools below for a visual introduction to the kidney. Click on either diagram to view animated presentations onhow our
kidneys work and how dialysis works to replace the work of healthy kidneys.
Diagram of how a healthy kidney works Structure of the kidneys and bladder
Kidney Health Australia acknowledges the generosity of DaVita (USA) for allowing us to use these images and host their excellent teaching resource (flash
animation) on our website.
WHAT CAN GO WRONG WITH THE KIDNEYS?
Most kidney diseases attack the nephrons. Sometimes kidney failure can happen quickly, caused for
example by a sudden loss of large amounts of blood or an accident. A sudden drop in kidney function
is called Acute Kidney Failure and is often short lived, but can occasionally lead to lasting kidney
damage. More often kidney function worsens over a number of years.
This is actually good news, because if kidney disease is found early, medication, dietary and lifestyle
changes can increase the life of your kidneys and keep you feeling your best for as long as possible.
Kidney disease progression can also be slowed with medicines which help to protect your kidneys. Your GP can prescribe these
medicines for your, which are available through your local pharmacist.
Take the test at Check My Kidneys to find out if you are at increased risk of kidney disease
What does Chronic Kidney Disease mean?
If you lose over 1/3 of your kidney function for over 3 months, it is called Chronic Kidney Disease or CKD. Sometimes kidney
disease leads to kidney failure, which requires dialysis or a kidney transplant to keep you alive. Early detection and treatment
can help prevent kidney failure and the need for dialysis or transplant treatment.
If you are diagnosed with CKD, this means that your kidneys have been damaged and are not working as well as they should
normally. Kidney disease is called a silent disease as there are often no warnings.
It is not uncommon for people to lose up to 90% of their kidney function before getting any symptoms.
People can live a near normal life with as little as 20 percent of their total kidney function.
When symptoms do occur the initial signs may be general, such as feeling tired or generalised itching.
As kidney disease progresses, symptoms can include changes in the urine (reduced volume, discolouration, blood or
pus), nausea and vomiting and appetite loss.
Other symptoms include swollen or numb hands and feet (because of water retention), weakness and lethargy,
darkened skin and muscle cramps.
About 50 people a day die of a kidney related disease.
How do you know if you have CKD?
In most cases CKD does not cause any symptoms and is detected because a test has shown
an abnormality. It may be a urine test for blood or protein; an X-ray or scan of the kidneys; or a
blood test to measure kidney function. Most cases are discovered by your GP as part of normal
care.
How common is CKD?
1 in 9 Australians over age 25 years have at least one clinical sign of existing CKD, such as
reduced kidney function or evidence of kidney damage. It is less common in young adults. In
the older person it is more common due to the natural aging of the kidneys. A number of
diseases can damage the kidneys such as diabetes, hypertension (high blood pressure) and
some inherited conditions. Almost all of these will damage both kidneys at the same time.
Go to our Fast Facts on CKD webpage for more stats
Useful links: Kidney Disease: Are you one in three?
KHA Kidney Health Resources including simplified translated versions
KHA webpages: Your heart and CKD and Diabetes and CKD
Urinary tract infections (also known as UTIs)
A UTI should be treated promptly as a kidney infection is serious. It is important to see a doctor if a kidney infection
or kidney stones are suspected because lasting damage or even kidney failure can occur if these conditions are left untreated. Infection which has spread
from cystitis or pyelonephritis can be life threatening.
WHY DO KIDNEYS FAIL?
Inside each kidney there are about one million tiny units called nephrons which filter blood as it passes through each nephron and water and waste products
are removed. Most of the water returns to the blood, the waste products collect in the bladder then leave the body as urine (wee).
'A closer look at kidney disease'
Professor Alan Cass
The George Institute - Renal and Metabolic Division
What can I do to keep my kidneys healthy?
Key recommendations to staying healthy and keeping your kidneys healthy as well are:
keep your blood pressure below 130/90 and maintain healthy levels of cholesterol
its important to have your cholesterol levels checked regularly - the recommended level is no higher than 5.5 mmol/litres
lead a healthy lifestyle and maintain healthy weight, be active for more than 30 minutes most days
eat a balanced healthy diet low in saturated fats
become a non smoker
if you have diabetes make sure you actively treat your blood glucose levels - normal levels are 4-6 mmol/L before meals and 4-8 mmol/L two-
hours after meals
Healthy Eating
The food you eat plays a huge role in the health and well being of your body. As well as providing the body with a variety of nutrients, food choicescan also
help in weight reduction and weight control.
eat healthy foods - with as many fresh ingredients as possible.
don't over eat - always leave a meal feeling like you could eat a little bit more.
eat breakfast - a good breakfast activates your metabolism first thing in the morning.
avoid fad diets - they are hard to maintain over a long period and can create or worsen ill health.
check nutrition panels on all parcelled foods you buy - choose only foods that list a low percentage of sugar and salt and are low in saturated fats
- find out about food ingredients.
To satisfy thirst - drink water instead!
Drink plenty of fluids - but choose to drink water instead! Water is the recommended choice, it is also
calorie-free, inexpensive and readily available. Sugar drinks have lots of calories, while caffeine and alcohol
are both diuretics and can leave the body dehydrated.
Research also states that one drink containing sugar each day, has been shown in females to be
associated with an 80 % increase in the risk of acquiring diabetes.
Note: Bottled mineral water contains salt which can lead to fluid retention and even increased blood
pressure in susceptible people. Check the label and choose low sodium varieties (less than 30mg sodium
per 100ml).
Losing weight can reduce how hard your kidneys need to work
Weight loss can also lead to a decrease in the amount of protein lost via urine. High levels of protein in the urine can make your kidney function worse.
Obesity may also cause some people with existing forms of some kidney disease to loose their kidney function more rapidly. There is also evidence to
suggest excess weight is also associated with an increased risk of kidney cancer. If you are overweight, you have an increased risk of
developing diabetes and high blood pressure - both are major risk factors for kidney disease. Losing as little as 5 kilograms reduces blood pressure in most
people who are 10% above a healthy weight.
Do at least 30 minutes of physical activity most days of the week
Stay fit. The key is to start slowly and gradually increase time and intensity of activities. Physical activity leads to increased strength, stamina and energy.
You can break down any activity into 3 x 10 minute bursts, which can be increased as fitness improves.
STOP exercising without delay, tell your health care team or go to hospital if you:
- have chest pain or pressure
- feel dizzy or light headed
- have an irregular or fast heart beat that persists when the activity is completed
- have excessive shortness of breath
Useful weblink: Measure Up and CKD for tips on a healthy life
Be or remain a non-smoker
It is well known smoking harms your health and greatly increases your risk of developing many chronic conditions. Smoking causes narrowing of the
arteries, including small vessels that are in the filter in sections of your kidney, and reduces the ability of the kidneys to work properly. Smoking has been
linked to cancer of the kidneys, the bladder and ureter (the small tubes that run from your kidneys to the bladder). The message is clear: don't smoke. If you
do smoke, giving up is one of the best things you can do to keep your kidneys healthier. Order a free QUIT pack - call the QUIT Hotline 137 848
Don't drink too much alcohol
Be smart about your alcohol intake. While some studies show alcohol causes no harm to the kidneys, it may be dangerous if you already have kidney
problems. Alcohol makes your kidney produce more urine than normal, and excessive drinking can have a negative impact on other parts of the body that
may contribute to kidney damage, such as the liver. To avoid dehydration caused by more frequent urination, ensure you alternate between alcoholic and
non-alcoholic drinks. A glass of water is of course the ideal choice here.
There have been studies that have shown that heavy drinking may contribute to high blood pressure and heart disease, which over time may contribute to
kidney disease. Alcohol has a high sugar content and therefore may lead to weight gain, another risk factor for kidney disease.
How many alcoholic drinks can you have without it affecting your kidneys?
There is evidence to suggest that one standard drink for women and the elderly (e.g.100ml wine; 285ml full strength beer; 30 ml spirit) or two standard
drinks for men, three to four times a week, may have a positive health effect.
Useful link: Australian guidelines to reduce health risks from drinking alcohol
Quick links: Fact Sheets> - Recommended weblinks - Organ Donation
22 June 2013 - Disclaimer: Information provided is intended as an introduction to this topic and not meant to substitute for your doctor's or health
professional's advice. All care is taken to ensure this information is relevant and applicable to each Australian state. Kidney Health Australia recognises each
person's experience is individual and variations do occur in treatment and management due to personal circumstances. Consult a healthcare professional
for specific treatment recommendations.
If concerned your medication may be affecting your health, refer to ABC Health Consumer Guides or check with Medicines Line 1300 MEDICINE (1300 633
424) for independent pharmacist advice on prescriptions, over-the-counter, and complementary (herbal / natural / vitamin / mineral) medicines.
Kidney
From Wikipedia, the free encyclopedia
For other uses, see Kidney (disambiguation).
Kidney
Human kidneys viewed from behind with spineremoved
Latin Ren (Greek: nephros)
System Urinary system and endocrine system
Artery Renal artery
Vein Renal vein
Nerve Renal plexus
MeSH Kidney
Dorlands/Elsevier Kidney
The kidneys are organs that serve several essential regulatory roles in most animals,
including vertebrates and some invertebrates. They are essential in the urinary system and also
serve homeostatic functions such as the regulation of electrolytes, maintenance ofacidbase balance, and
regulation of blood pressure (via maintaining salt and water balance). They serve the body as a natural filter of
the blood, and remove wastes which are diverted to the urinary bladder. In producing urine, the kidneys excrete
wastes such asurea and ammonium, and they are also responsible for the reabsorption of water, glucose,
and amino acids. The kidneys also produce hormones including calcitriol, erythropoietin, and the enzyme renin.
Located at the rear of the abdominal cavity in the retroperitoneum, the kidneys receive blood from the
paired renal arteries, and drain into the paired renal veins. Each kidney excretes urine into a ureter, itself a
paired structure that empties into the urinary bladder.
Renal physiology is the study of kidney function, while nephrology is the medical specialty concerned
with kidney diseases. Diseases of the kidney are diverse, but individuals with kidney disease frequently display
characteristic clinical features. Common clinical conditions involving the kidney include
the nephritic and nephrotic syndromes, renal cysts, acute kidney injury, chronic kidney disease, urinary tract
infection, nephrolithiasis, and urinary tract obstruction.
[1]
Various cancers of the kidney exist; the most common
adult renal cancer is renal cell carcinoma. Cancers, cysts, and some other renal conditions can be managed
with removal of the kidney, or nephrectomy. When renal function, measured by glomerular filtration rate, is
persistently poor, dialysis and kidney transplantation may be treatment options. Although they are not severely
harmful, kidney stones can be painful and a nuisance. The removal of kidney stones
involves ultrasound treatment to break up the stones into smaller pieces, which are then passed through the
urinary tract. One common symptom of kidney stones is a sharp pain in the medial/lateral segments of the
lower back.
Contents
[hide]
1 Anatomy
o 1.1 Location
o 1.2 Structure
o 1.3 Blood supply
o 1.4 Histology
o 1.5 Innervation
2 Functions
o 2.1 Excretion of wastes
o 2.2 Reabsorption of vital nutrients
o 2.3 Acid-base homeostasis
o 2.4 Osmolality regulation
o 2.5 Blood pressure regulation
o 2.6 Hormone secretion
3 Development
4 Evolutionary adaptation
5 Related terms
6 Diseases and disorders
o 6.1 Congenital
o 6.2 Acquired
o 6.3 Diagnosis
6.3.1 Clinical
6.3.2 Laboratory
6.3.3 Imaging studies
6.3.4 Renal biopsy
7 Calculations
o 7.1 Filtration Fraction
o 7.2 Renal Clearance
8 In other animals
9 History
10 Kidneys as food
11 See also
12 Additional Images
13 References
14 External links
Anatomy[edit source | editbeta]
Location[edit source | editbeta]
Surface projections of the organs of the trunk, showing kidneys at the level of T12 to L2.
A CT scan in which the kidneys are shown
In humans the kidneys are located in the abdominal cavity, more specifically in the paravertebral gutter and lie
in aretroperitoneal position at a slightly oblique angle. There are two kidneys. One is on each side of the
spine.
[2]
The asymmetry within the abdominal cavity caused by the liver typically results in the right kidney
being slightly lower than the left, and left kidney being located slightly more medial than the right.
[3][4]
The left
kidney is approximately at the vertebral level T12 to L3,
[5]
and the right slightly lower. The right kidney sits just
below the diaphragm and posterior to the liver, the left below the diaphragm and posterior to the spleen.
Resting on top of each kidney is anadrenal gland. The upper (cranial) parts of the kidneys are partially
protected by the eleventh and twelfth ribs, and each whole kidney and adrenal gland are surrounded by two
layers of fat (the perirenal and pararenal fat) and therenal fascia. Each adult kidney weighs between 125 and
170 grams in males and between 115 and 155 grams in females.
[6]
The left kidney is usually slightly larger than
the right kidney.
[7]
Structure[edit source | editbeta]
1. Renal pyramid 2. Interlobular artery 3. Renal artery 4. Renal vein 5. Renal hilum 6. Renal pelvis 7. Ureter 8. Minor calyx 9. Renal
capsule 10. Inferior renal capsule 11. Superior renal capsule 12. Interlobular vein 13. Nephron 14. Minor calyx 15. Major calyx
16. Renal papilla 17. Renal column
The kidney has a bean-shaped structure; each kidney has a convexand concave surface. The concave
surface, the renal hilum, is the point at which the renal artery enters the organ, and the renal
veinand ureter leave. The kidney is surrounded by tough fibrous tissue, the renal capsule, which is itself
surrounded by perinephric fat, renal fascia (of Gerota) and paranephric fat. The anterior (front) border of these
tissues is the peritoneum, while the posterior (rear) border is the transversalis fascia.
The superior border of the right kidney is adjacent to the liver; and the spleen, for the left kidney. Therefore,
both move down on inhalation.
The kidney is approximately 1114 cm in length, 6 cm wide and 4 cm thick.
The substance, or parenchyma, of the kidney is divided into two major structures: superficial is the renal
cortex and deep is therenal medulla. Grossly, these structures take the shape of 8 to 18 cone-shaped renal
lobes, each containing renal cortex surrounding a portion of medulla called a renal
pyramid (of Malpighi).
[6]
Between the renal pyramids are projections of cortex calledrenal
columns (of Bertin). Nephrons, the urine-producing functional structures of the kidney, span the cortex and
medulla. The initial filtering portion of a nephron is the renal corpuscle, located in the cortex, which is followed
by a renal tubule that passes from the cortex deep into the medullary pyramids. Part of the renal cortex,
a medullary ray is a collection of renal tubules that drain into a single collecting duct.
The tip, or papilla, of each pyramid empties urine into a minor calyx; minor calyces empty into major calyces,
and major calyces empty into the renal pelvis, which becomes the ureter. At the hilum, the ureter and renal vein
exit the kidney while the renal artery enters. Surrounding these structures is hilar fat and lymphatic tissue with
lymph nodes. The hilar fat is contiguous with a fat-filled cavity called the renal sinus. The renal sinus
collectively contains the renal pelvis and calyces and separates these structures from the renal medullary
tissue.
[8]
Blood supply[edit source | editbeta]
3D-rendered computed tomography, showing renal arteries and veins.
The kidneys receive blood from the renal arteries, left and right, which branch directly from the abdominal
aorta. Despite their relatively small size, the kidneys receive approximately 20% of the cardiac output.
[6]
Each renal artery branches into segmental arteries, dividing further into interlobar arteries which penetrate the
renal capsule and extend through the renal columns between the renal pyramids. The interlobar arteries then
supply blood to the arcuate arteries that run through the boundary of the cortex and the medulla. Each arcuate
artery supplies several interlobular arteries that feed into the afferent arteriolesthat supply the glomeruli.
The interstitium is the functional space in the kidney beneath the individual filters (glomeruli) which are rich
in blood vessels. The interstitum absorbs fluid recovered from urine. Various conditions can lead
to scarring and congestion of this area, which can cause kidney dysfunction and failure.
After filtration occurs the blood moves through a small network of venules that converge into interlobular veins.
As with the arteriole distribution the veins follow the same pattern, the interlobular provide blood to the arcuate
veins then back to the interlobar veins which come to form the renal vein exiting the kidney for transfusion for
blood.
Histology[edit source | editbeta]
Microscopic photograph of the renal medulla
Microscopic photograph of the renal cortex
Renal histology studies the structure of the kidney as viewed under a microscope. Various distinct cell
types occur in the kidney, including:
Kidney glomerulus parietal cell
Kidney glomerulus podocyte
Kidney proximal tubule brush border cell
Loop of Henle thin segment cell
Thick ascending limb cell
Kidney distal tubule cell
Kidney collecting duct cell
Interstitial kidney cells
Renal arteries and their branches
The renal artery enters into the kidney at the level of first lumbar vertebra just below the superior mesenteric
artery. As it enters the kidney it divides into branches: first the segmental artery, which divides into 2 or 3 lobar
arteries, then further divides into interlobar arteries, which further divide into the arcuate artery which leads into
the interlobular artery, which form afferent arterioles. The afferent arterioles form the glomerulus (network of
capillaries closed in Bowman's capsule). From here, efferent arterioles leaves the glomerulus and divide into
peritubular capillaries, which drain into the interlobular veins and then into arcuate vein and then into interlobar
vein, which runs into lobar vein, which opens into the segmental vein and which drains into the renal vein, and
then from it blood moves into the inferior vena cava.
Innervation[edit source | editbeta]
The kidney and nervous system communicate via the renal plexus, whose fibers course along the renal arteries
to reach each kidney.
[9]
Input from the sympathetic nervous system triggers vasoconstriction in the kidney,
thereby reducing renal blood flow.
[9]
The kidney also receives input from the parasympathetic nervous system,
by way of the renal branches of the vagus nerve (cranial nerve X); the function of this is yet
unclear.
[9][10]
Sensory input from the kidney travels to the T10-11 levels of the spinal cord and is sensed in the
correspondingdermatome.
[9]
Thus, pain in the flank region may be referred from corresponding kidney.
[9]
Functions[edit source | editbeta]
Main article: Renal physiology
The kidney participates in whole-body homeostasis, regulating acid-base
balance, electrolyte concentrations, extracellular fluid volume, and regulation of blood pressure. The kidney
accomplishes these homeostatic functions both independently and in concert with other organs, particularly
those of the endocrine system. Various endocrine hormones coordinate these endocrine functions; these
include renin, angiotensin II, aldosterone, antidiuretic hormone, and atrial natriuretic peptide, among others.
Many of the kidney's functions are accomplished by relatively simple mechanisms of filtration, reabsorption,
and secretion, which take place in the nephron. Filtration, which takes place at the renal corpuscle, is the
process by which cells and large proteins are filtered from the blood to make an ultrafiltrate that eventually
becomes urine. The kidney generates 180 liters of filtrate a day, while reabsorbing a large percentage, allowing
for the generation of only approximately 2 liters of urine. Reabsorption is the transport of molecules from this
ultrafiltrate and into the blood. Secretion is the reverse process, in which molecules are transported in the
opposite direction, from the blood into the urine.
Excretion of wastes[edit source | editbeta]
The kidneys excrete a variety of waste products produced by metabolism. These include the nitrogenous
wastes called "urea", from protein catabolism, as well as uric acid, fromnucleic acid metabolism. Formation of
urine is also the function of the kidney. The concentration of nitrogenous wastes, in the urine of mammals and
some birds, is dependent on an elaborate countercurrent multiplication system. This requires several
independent nephron characteristics to operate: a tight hair pin configuration of the tubules, water and ion
permeability in the descending limb of the loop, water impermeability in the ascending loop and active ion
transport out of most of the ascending loop. In addition, countercurrent exchange by the vessels carrying the
blood supply to the nephron is essential for enabling this function.
Reabsorption of vital nutrients[edit source | editbeta]
Glucose at normal plasma levels is completely reabsorbed in the proximal tubule. The mechanism for this is the
Na+/glucose cotransporter. A plasma level of 350 mg/dL will fully saturate the transporters and glucose will be
lost in the urine. A plasma glucose level of approximately 160 is sufficient to allow glucosuria which is an
important clinical clue to diabetes mellitus.
Amino acids are reabsorbed by sodium dependent transporters in the proximal tubule. Hartnup's disease is a
deficiency of the tryptophan amino acid transporter which results inpellagra.
[11]
Location of
Reabsorption
Reabsorbed nutrient Notes
Early proximal
tubule
Glucose (100%), amino acids (100%), bicarbonate
(90%), Na+ (65%), Cl-, phosphate and H2O (65%)
PTH will inhibit phosphate excretion
AT II stimulates Na+, H2O and HCO3-
reabsorption.
Thin descending
loop of Henle
H2O
Reabsorbs via medullary hypertonicity and
makes urine hypertonic.
Thick ascending loop
of Henle
Na+ (10-20%), K+, Cl-; indirectly induces para
cellular reabsorption of Mg2+, Ca2+
This region is impermeable to H2O and the
urine becomes less concentrated as it ascends.
Early distal
convoluted tubule
Na+, Cl-
PTH causes Ca2+ reabsorption.
Collecting tubules Na+(3-5%), H2O
Na+ is reabsorbed in exchange for K+ and H+
which is regulated by aldosterone.
ADH acts on the V2 receptor and
inserts aquaporins on the luminal side
[11]
Pregnancy reduces the reabsorption of glucose and amino acids.
Acid-base homeostasis[edit source | editbeta]
Main article: Acid-base homeostasis
Two organ systems, the kidneys and lungs, maintain acid-base homeostasis, which is the maintenance
of pH around a relatively stable value. The lungs contribute to acid-base homeostasis by regulating carbon
dioxide (CO
2
) concentration. The kidneys have two very important roles in maintaining the acid-base balance:
to reabsorb bicarbonate from urine, and to excrete hydrogen ions into urine
Osmolality regulation[edit source | editbeta]
Any significant rise in plasma osmolality is detected by the hypothalamus, which communicates directly with
the posterior pituitary gland. An increase in osmolality causes the gland to secrete antidiuretic hormone (ADH),
resulting in water reabsorption by the kidney and an increase in urine concentration. The two factors work
together to return the plasma osmolality to its normal levels.
ADH binds to principal cells in the collecting duct that translocate aquaporins to the membrane, allowing water
to leave the normally impermeable membrane and be reabsorbed into the body by the vasa recta, thus
increasing the plasma volume of the body.
There are two systems that create a hyperosmotic medulla and thus increase the body plasma volume: Urea
recycling and the 'single effect.'
Urea is usually excreted as a waste product from the kidneys. However, when plasma blood volume is low and
ADH is released the aquaporins that are opened are also permeable to urea. This allows urea to leave the
collecting duct into the medulla creating a hyperosmotic solution that 'attracts' water. Urea can then re-enter the
nephron and be excreted or recycled again depending on whether ADH is still present or not.
The 'Single effect' describes the fact that the ascending thick limb of the loop of Henle is not permeable to
water but is permeable to NaCl. This allows for a countercurrent exchangesystem whereby the medulla
becomes increasingly concentrated, but at the same time setting up an osmotic gradient for water to follow
should the aquaporins of the collecting duct be opened by ADH.
Blood pressure regulation[edit source | editbeta]
Main articles: Blood pressure regulation and Renin-angiotensin system
Although the kidney cannot directly sense blood, long-term regulation of blood pressure predominantly
depends upon the kidney. This primarily occurs through maintenance of theextracellular fluid compartment, the
size of which depends on the plasma sodium concentration. Renin is the first in a series of important chemical
messengers that make up therenin-angiotensin system. Changes in renin ultimately alter the output of this
system, principally the hormones angiotensin II and aldosterone. Each hormone acts via multiple mechanisms,
but both increase the kidney's absorption of sodium chloride, thereby expanding the extracellular fluid
compartment and raising blood pressure. When renin levels are elevated, the concentrations of angiotensin II
and aldosterone increase, leading to increased sodium chloride reabsorption, expansion of the extracellular
fluid compartment, and an increase in blood pressure. Conversely, when renin levels are low, angiotensin II
and aldosterone levels decrease, contracting the extracellular fluid compartment, and decreasing blood
pressure.
Hormone secretion[edit source | editbeta]
The kidneys secrete a variety of hormones, including erythropoietin, and the enzyme renin. Erythropoietin is
released in response to hypoxia (low levels of oxygen at tissue level) in the renal circulation. It
stimulates erythropoiesis (production of red blood cells) in the bone marrow. Calcitriol, the activated form
of vitamin D, promotes intestinal absorption ofcalcium and the renal reabsorption of phosphate. Part of
the renin-angiotensin-aldosterone system, renin is an enzyme involved in the regulation of aldosterone levels.
Development[edit source | editbeta]
Main article: Kidney development
The mammalian kidney develops from intermediate mesoderm. Kidney development, also
called nephrogenesis, proceeds through a series of three successive phases, each marked by the development
of a more advanced pair of kidneys: the pronephros, mesonephros, and metanephros.
[12]
Evolutionary adaptation[edit source | editbeta]
Kidneys of various animals show evidence of evolutionary adaptation and have long been studied
in ecophysiology and comparative physiology. Kidney morphology, often indexed as the relative medullary
thickness, is associated with habitat aridity among species of mammals.
[13]
Related terms[edit source | editbeta]
Medical terms related to the kidneys commonly use terms such as renal and the prefix nephro-.
The adjective renal, meaning related to the kidney, is from the Latin rns, meaning kidneys; the prefix nephro-
is from the Ancient Greek word for kidney, nephros ().
[14]
For example, surgical removal of the kidney is
a nephrectomy, while a reduction in kidney function is called renal dysfunction.
Diseases and disorders[edit source | editbeta]
Main article: Nephropathy
See also: Glomerular lipidosis
Congenital[edit source | editbeta]
Congenital hydronephrosis
Congenital obstruction of urinary tract
Duplex kidneys, or double kidneys, occur in approximately 1% of the population. This occurrence normally
causes no complications, but can occasionally cause urine infections.
[15][16]
Duplicated ureter occurs in approximately one in 100 live births
Horseshoe kidney occurs in approximately one in 400 live births
Polycystic kidney disease
Autosomal dominant polycystic kidney disease afflicts patients later in life. Approximately one in 1000
people will develop this condition
Autosomal recessive polycystic kidney disease is far less common, but more severe, than the
dominant condition. It is apparent in utero or at birth.
Renal agenesis. Failure of one kidney to form occurs in approximately one in 750 live births. Failure of
both kidneys to form is invariably fatal.
Renal dysplasia
Unilateral small kidney
Multicystic dysplastic kidney occurs in approximately one in every 2400 live births
Ureteropelvic Junction Obstruction or UPJO; although most cases appear congenital, some appear to be
an acquired condition
[17]
Acquired[edit source | editbeta]
Drawing of an enlarged kidney by John Hunter.
Diabetic nephropathy
Glomerulonephritis
Glomerular lipidosis
Hydronephrosis is the enlargement of one or both of the kidneys caused by obstruction of the flow of urine.
Interstitial nephritis
Kidney stones (nephrolithiasis) are a relatively common and particularly painful disorder.
Kidney tumors
Wilms tumor
Renal cell carcinoma
Lupus nephritis
Minimal change disease
In nephrotic syndrome, the glomerulus has been damaged so that a large amount of protein in the blood
enters the urine. Other frequent features of the nephrotic syndrome include swelling, low serum albumin,
and high cholesterol.
Pyelonephritis is infection of the kidneys and is frequently caused by complication of a urinary tract
infection.
Renal failure
Acute renal failure
Stage 5 Chronic Kidney Disease
Kidney Failure
Main article: Renal failure
Generally, humans can live normally with just one kidney, as one has more functioning renal tissue than is
needed to survive. Only when the amount of functioning kidney tissue is greatly diminished does one
develop chronic kidney disease. Renal replacement therapy, in the form of dialysis or kidney transplantation, is
indicated when the glomerular filtration rate has fallen very low or if the renal dysfunction leads to severe
symptoms.
Diagnosis[edit source | editbeta]
Clinical[edit source | editbeta]
Many renal diseases are diagnosed on the basis of classical clinical findings. A physician (usually
a nephrologist) begins by taking a detailed clinical history and performs a physical examination. In addition to
medical history and presenting symptoms, a physician will ask about medication history, family history recent
infections, toxic/chemical exposures and other historical factors which may indicate an etiology for the patient's
renal disease. Often, some diseases are suggested by clinical history and time course alone. For example, in a
formerly healthy child with a recent upper respiratory tract infection and facial/lower limb swelling, findings of
proteinuria on urinalysis, a diagnosis of minimal change disease is highly suggested. Similarly, a patient with a
history of diabetes who presents with decreased urine output is most likely to be suffering from diabetic
nephropathy. Often, such cases do not require extensive workup (such as with renal biopsy). A presumptive
diagnosis can be made on the basis of history, physical exam and supportive laboratory studies.
Laboratory[edit source | editbeta]
Laboratory studies are an important adjunct to clinical evaluation for assessment of renal function. An initial
workup of a patient may include a complete blood count (CBC); serum electrolytes including sodium,
potassium, chloride, bicarbonate, calcium, and phosphorus; blood urea, nitrogen and creatinine; blood glucose
and glycocylated hemoglobin. Glomerular filtration rate (GFR) can be calculated.
[18]
Urine studies may include urine electrolytes, creatinine, protein, fractional excretion of sodium (FENA) and
other studies to assist in evaluation of the etiology of a patient's renal disease.
Urinalysis is used to evaluate urine for its pH, protein, glucose, specific gravity and the presence of
blood/hemoglobin. Microscopic analysis can be helpful in the identification of casts, red blood cells, white blood
cells and crystals.
[18]
Imaging studies[edit source | editbeta]
Imaging studies are important in the evaluation of structural renal disease caused by urinary tract obstruction,
renal stones, renal cyst, mass lesions, renal vascular disease, and vesicoureteral reflux.
[18]
Imaging techniques used most frequently include renal ultrasound and helical CT scan. Patients with suspected
vesicoureteral reflux may undergo voiding cystourethrogram (VCUG).
Renal biopsy[edit source | editbeta]
The role of the renal biopsy is to diagnose renal disease in which the etiology is not clear based upon
noninvasive means (clinical history, past medical history, medication history, physical exam, laboratory studies,
imaging studies).
A detailed description of renal biopsy interpretation is beyond the scope of this article. In general- a renal
pathologist will perform a detailed morphological evaluation and integrate the morphologic findings with the
clinical history and laboratory data, ultimately arriving at a pathological diagnosis. A renal pathologist is a
physician who has undergone general training in anatomic pathology and additional specially training in the
interpretation of renal biopsy specimens.
Ideally, multiple core sections are obtained and evaluated for adequacy (presence of glomeruli)
intraoperatively. A pathologist/pathology assistant divides the specimen(s) for submission for light microscopy,
immunofluorescence microscopy and electron microscopy.
The pathologist will examine the specimen using light microscopy with multiple staining techniques
(hematoxylin and eosin/H&E, PAS, trichrome, silver stain) on multiple level sections. Multiple
immunofluorescence stains are performed to evaluate for antibody, protein and complement deposition. Finally,
ultra-structural examination is performed with electron microscopy and may reveal the presence of electron-
dense deposits or other characteristic abnormalities which may suggest an etiology for the patient's renal
disease.
Calculations[edit source | editbeta]
Calculations of kidney performance are an important part of physiology and can be estimated using the
calculations below.
Filtration Fraction[edit source | editbeta]
The filtration fraction is the amount of plasma which is actually filtered through the kidney. This can be defined
using the equation:
FF=GFRRPF
FF is the filtration fraction
GFR is the glomerular filtration rate
RPF is the renal plasma flow
Normal human FF is 20%.
Renal Clearance[edit source | editbeta]
Renal clearance is the volume of plasma from which the substance is completely cleared from the blood per
unit time.
C
x
=(U
x
)VP
x
C
x
is the clearance of X (normally in units of mL/min.
U
x
is the urine concentration of X.
P
x
is the plasma concentration of X.
V is the urine flow rate.
More information regarding renal function can be found on the Renal function Wikipedia page.
In other animals[edit source | editbeta]
A pig's kidney opened.
In the majority of vertebrates, the mesonephros persists into the adult, albeit usually fused with the more
advanced metanephros; only inamniotes is the mesonephros restricted to the embryo. The kidneys
of fish and amphibians are typically narrow, elongated organs, occupying a significant portion of the trunk. The
collecting ducts from each cluster of nephrons usually drain into an archinephric duct, which
is homologous with the vas deferens of amniotes. However, the situation is not always so simple;
in cartilaginous fish and some amphibians, there is also a shorter duct, similar to the amniote ureter, which
drains the posterior (metanephric) parts of the kidney, and joins with the archinephric duct at
the bladder or cloaca. Indeed, in many cartilaginous fish, the anterior portion of the kidney may degenerate or
cease to function altogether in the adult.
[19]
In the most primitive vertebrates, the hagfish and lampreys, the kidney is unusually simple: it consists of a row
of nephrons, each emptying directly into the archinephric duct. Invertebrates may possess excretory organs
that are sometimes referred to as "kidneys", but, even in Amphioxus, these are never homologous with the
kidneys of vertebrates, and are more accurately referred to by other names, such as nephridia.
[19]
The kidneys of reptiles consist of a number of lobules arranged in a broadly linear pattern. Each lobule contains
a single branch of the ureter in its centre, into which the collecting ducts empty. Reptiles have relatively few
nephrons compared with other amniotes of a similar size, possibly because of their lower metabolic rate.
[19]
Birds have relatively large, elongated kidneys, each of which is divided into three or more distinct lobes. The
lobes consists of several small, irregularly arranged, lobules, each centred on a branch of the ureter. Birds
have small glomeruli, but about twice as many nephrons as similarly sized mammals.
[19]
The human kidney is fairly typical of that of mammals. Distinctive features of the mammalian kidney, in
comparison with that of other vertebrates, include the presence of the renal pelvis and renal pyramids, and of a
clearly distinguishable cortex and medulla. The latter feature is due to the presence of elongated loops of
Henle; these are much shorter in birds, and not truly present in other vertebrates (although the nephron often
has a short intermediate segment between the convoluted tubules). It is only in mammals that the kidney takes
on its classical "kidney" shape, although there are some exceptions, such as the multilobed reniculate
kidneys of cetaceans.
[19]
History[edit source | editbeta]
The Latin term renes is related to the English word "reins", a synonym for the kidneys in Shakespearean
English (e.g. Merry Wives of Windsor 3.5), which was also the time theKing James Version was translated.
Kidneys were once popularly regarded as the seat of the conscience and reflection,
[20][21]
and a number of
verses in the Bible (e.g. Ps. 7:9, Rev. 2:23) state that God searches out and inspects the kidneys, or "reins", of
humans. Similarly, the Talmud (Berakhoth 61.a) states that one of the two kidneys counsels what is good, and
the other evil.
Kidneys as food[edit source | editbeta]
Hkarpanna, Swedish pork and kidney stew
The kidneys can be cooked and eaten (along with other offal).
Kidneys are usually grilled or sauted, but in more complex dishes they are stewed with a sauce that will
improve their flavor. In many preparations, kidneys are combined with pieces of meat or liver, as in mixed
grill or meurav Yerushalmi. Dishes include the British steak and kidney pie, the Swedish hkarpanna (pork and
kidney stew), the French rognons de veau sauce moutarde (veal kidneys in mustardsauce) and
the Spanish riones al Jerez (kidneys stewed in sherry sauce) .
[22]
See also[edit source | editbeta]
Artificial kidney
Holonephros
Organ donation
Organ harvesting
Pelvic kidney
World Kidney Day
Additional Images[edit source | editbeta]
Right Kidney
Kidney
Right Kidney
Kidney Posterior View
Anterior relation of Left Kidney
Right kidney
Left kidney
Kidneys
Left kidney
Kidney Cross Section
References[edit source | editbeta]
1. ^ Cotran, RS S.; Kumar, Vinay; Fausto, Nelson; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran
pathologic basis of disease. St. Louis, MO: Elsevier Saunders. ISBN 0-7216-0187-1.
2. ^ "HowStuffWorks How Your Kidney Works".
3. ^ "Kidneys Location Stock Illustration".
4. ^ [1]
[dead link]
5. ^ Blens ytanatomy (Superficial anatomy of the trunk). Anca Dragomir, Mats Hjortberg and Godfried M. Romans.
Section for human anatomy at the Department of medical biology, Uppsala university, Sweden.
6. ^
a
b
c
Walter F., PhD. Boron (2004). Medical Physiology: A Cellular And Molecular Approach.
Elsevier/Saunders. ISBN 1-4160-2328-3.
7. ^ Glodny B, Unterholzner V, Taferner B, et al. (2009). "Normal kidney size and its influencing factors - a 64-slice
MDCT study of 1.040 asymptomatic patients". BMC Urology 9: 19. doi:10.1186/1471-2490-9-
19. PMC 2813848. PMID 20030823.
8. ^ Clapp, WL. Renal Anatomy. In: Zhou XJ, Laszik Z, Nadasdy T, D'Agati VD, Silva FG, eds. Silva's Diagnostic
Renal Pathology. New York, NY: Cambridge University Press; 2009.
9. ^
a
b
c
d
e
Bard, Johnathan; Vize, Peter D.; Woolf, Adrian S. (2003). The kidney: from normal development to
congenital disease. Boston: Academic Press. p. 154. ISBN 0-12-722441-6.
10. ^ Schrier, Robert W.; Berl, Tomas; Harbottle, Judith A. (1972). "Mechanism of the Antidiuretic Effect Associated
with Interruption of Parasympathetic Pathways". Journal Clinical Investigation 51 (10): 2613
20. doi:10.1172/JCI107079. PMC 332960.PMID 5056657.
11. ^
a
b
Le, Tao. First Aid for the USMLE Step 1 2013. New York: McGraw-Hill Medical, 2013. Print.
12. ^ Bruce M. Carlson (2004). Human Embryology and Developmental Biology (3rd ed.). Saint Louis:
Mosby. ISBN 0-323-03649-X.
13. ^ Al-kahtani, M. A.; C. Zuleta, E. Caviedes-Vidal, and T. Garland, Jr. (2004). "Kidney mass and relative medullary
thickness of rodents in relation to habitat, body size, and phylogeny". Physiological and Biochemical
Zoology 77 (3): 346365.doi:10.1086/420941. PMID 15286910.
14. ^ Maton, Anthea; Jean Hopkins, Charles William McLaughlin, Susan Johnson, Maryanna Quon Warner, David
LaHart, Jill D. Wright (1993). Human Biology and Health. Englewood Cliffs, New Jersey, USA: Prentice
Hall. ISBN 0-13-981176-1.
15. ^ Sample, Ian (2008-02-19). "How many people have four kidneys?". The Guardian(London).
16. ^ "Girl's Kidneys Fail, But Doctors Find Double Valves, Saving Her Life". Abcnews.go.com. 2010-05-18. Retrieved
2011-01-03.
17. ^ Stephen Jones, J.; Inderbir S. Gill, Raymond Rackley (2006). Operative Urology at the Cleveland Clinic. Andrew
C. Novick, Inderbir S. Gill, Eric A. Klein, Jonathan H. Ross (eds.). Totowa, NJ: Humana Press. ISBN 978-1-58829-
081-6. Retrieved 2010-10-09.
18. ^
a
b
c
Post TW, Rose BD, auths and Curhan GC, Sheridan AM, eds. Diagnostic Approach to the Patient With
Acute Kidney Injury (Acute Renal Failure) or Chronic Kidney Disease. UpToDate.com, Dec.
2012.http://www.uptodate.com.ezproxy2.library.arizona.edu/contents/diagnostic-approach-to-the-patient-with-
acute-kidney-injury-acute-renal-failure-or-chronic-kidney-
disease?source=preview&anchor=H12&selectedTitle=1~150#H12
19. ^
a
b
c
d
e
Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, PA: Holt-
Saunders International. pp. 367376. ISBN 0-03-910284-X.
20. ^ The Patient as Person: Explorations in Medical Ethics p. 60 by Paul Ramsey, Margaret Farley, Albert Jonsen,
William F. May (2002)
21. ^ History of Nephrology 2 p. 235 by International Association for the History of Nephrology Congress, Garabed
Eknoyan, Spyros G. Marketos, Natale G. De Santo - 1997; Reprint of American Journal of Nephrology; v. 14, no.
4-6, 1994.
22. ^ Rognons dans les recettes (French)
External links[edit source | editbeta]
Wikimedia Commons has
media related to: Kidneys
The NephCure Foundation offers educational materials on the kidney diseases/conditions Nephrotic
Syndrome and FSGS
The Kidney Foundation of Canada
electron microscopic images of the kidney (Dr. Jastrow's EM-Atlas)
European Renal Genome project kidney function tutorial
Kidney Foundation of Canada kidney disease information
Renal Fellow Network: Structure & Function of Other Animals' Kidneys
Kidney Stones
Kidney Diseases
Kidney Information
Animated Presentatin on Kidney Function
CAT Scans of various kidney diseases and conditions - CT Cases
Kidney Stones; Information and Treatments
[show]
V
T
E
Systems and organs of the animal anatomy
[show]
V
T
E
Anatomy: urinary system (TA A08, TH H3.06, GA 11.1215)
Categories:
Kidney
Endocrine system
A List of Kidney Diseases
AbderhaldenKaufmannLignac syndrome (Nephropathic Cystinosis)
Acute Kidney Failure/Acute Kidney Injury
Acute Lobar Nephronia
Acute Phosphate Nephropathy
Acute Tubular Necrosis
Adenine Phosphoribosyltransferase Deficiency
Adenovirus Nephritis
Alport Syndrome
Amyloidosis
ANCA Vasculitis Related to Endocarditis and Other Infections
Angiomyolipoma
Analgesic Nephropathy
Anorexia Nervosa and Kidney Disease
Angiotensin Antibodies and Focal Segmental Glomerulosclerosis
Antiphospholipid Syndrome
APOL1 Mutations
Apparent Mneralocorticoid Excess Syndrome
Aristolochic Acid Nephropathy, Chinese Herbal Nephropathy, Balkan Endemic Nephropathy
Bartter Syndrome
Beeturia
-Thalassemia Renal Disease
Bile Cast Nephropathy
BK Polyoma Virus Nephropathy in the Native Kidney
Bladder Rupture
Bladder Sphincter Dyssynergia
Bladder Tamponade
Border-Crossers' Nephropathy
C1q Nephropathy
Cardiorenal syndrome
CFHR5 nephropathy
Cholesterol Emboli
ChurgStrauss syndrome
Collapsing Glomerulopathy, Collapsing Glomerulopathy Related to CMV
Congenital Nephrotic Syndrome
Conorenal syndrome (Mainzer-Saldino Syndrome or Saldino-Mainzer Disease)
Contrast Nephropathy
Copper Sulpfate Intoxication
Cortical Necrosis
Cryoglobuinemia
Crystal-Induced Acute Kidney injury
Cystic Kidney Disease, Acquired
Cystinuria
Dasatinib-Induced Nephrotic-Range Proteinuria
Dense Deposit Disease (MPGN Type 2)
Dent Disease (X-linked Recessive Nephrolithiasis)
Diabetes and Diabetic Kidney Disease
Diabetes Insipidus
Dietary Supplements and Renal Failure
Duplicated Ureter
EAST syndrome
Ectopic Ureter
Edema, Swelling
Erdheim-Chester Disease
Fabrys Disease
Familial Hypocalciuric Hypercalcemia
Fanconi Syndrome
Fraser syndrome
Fibronectin Glomerulopathy
Fibrillary Glomerulonephritis and Immunotactoid Glomerulopathy
Fraley syndrome
Focal Segmental Glomerulosclerosis, Focal Sclerosis, Focal Glomerulosclerosis
Galloway Mowat syndrome
Giant Cell (Temporal) Arteritis with Kidney Involvement
Gestational Hypertension
Gitelman Syndrome
Glomerular Diseases
Glomerular Tubular Reflux
Glycosuria
Goodpasture Syndrome
Hematuria (Blood in Urine)
Hemolytic Uremic Syndrome (HUS), Atypical Hemolytic Uremic Syndrome (aHUS)
Hemorrhagic Cystitis
Hemorrhagic Fever with Renal Syndrome (HFRS, Hantavirus Renal Disease, Korean Hemorrhagic Fever,
Epidemic Hemorrhagic Fever, Nephropathis Epidemica)
Hemosiderosis related to Paroxysmal Nocturnal Hemoglobinuria and Hemolytic Anemia
Hepatic Veno-Occlusive Disease, Sinusoidal Obstruction Syndrome
Hepatitis C-Associated Renal Disease
Hepatorenal Syndrome
High Blood Pressure and Kidney Disease
HIV-Associated Nephropathy (HIVAN)
Horseshoe Kidney (Renal Fusion)
Hunner's Ulcer
Hyperaldosteronism
Hypercalcemia
Hyperkalemia
Hypermagnesemia
Hypernatremia
Hyperoxaluria
Hyperphosphatemia
Hypocalcemia
Hypokalemia, Hypokalemia-induced renal dysfunction
Hypomagnesemia
Hyponatremia
Hypophosphatemia
IgA Nephropathy
IgG4 Nephropathy
Interstitial Cystitis, Painful Bladder Syndrome (Questionnaire)
Interstitial Nephritis
Ivemark's syndrome
Ketamine-Associated Bladder Dysfunction
Kidney Stones, Nephrolithiasis
Kombucha Tea Toxicity
Lead Nephropathy and Lead-Related Nephrotoxicity
Leptospirosis Renal Disease
Light Chain Deposition Disease, Monoclonal Immunoglobulin Deposition Disease
Liddle Syndrome
Lightwood-Albright Syndrome
Lipoprotein Glomerulopathy
Lithium Nephrotoxicity
LMX1B Mutations Cause Hereditary FSGS
Loin Pain Hematuria
Lupus, Systemic Lupus Erythematosis
Lupus Kidney Disease, Lupus Nephritis
Lyme Disease-Associated Glomerulonephritis
Malarial Nephropathy
Malignancy-Associated Renal Disease
Malignant Hypertension
Malakoplakia
Meatal Stenosis
Medullary Cystic Kidney Disease
Medullary Sponge Kidney
Megaureter
Melamine Toxicity and the Kidney
Membranoproliferative Glomerulonephritis
Membranous Nephropathy
MesoAmerican Nephropathy
Metabolic Acidosis
Metabolic Alkalosis
Microscopic Polyangiitis
Milk-alkalai syndrome
Minimal Change Disease
Multicystic dysplastic kidney
Multiple Myeloma
Myeloproliferative Neoplasms and Glomerulopathy
Nail-patella Syndrome
Nephrocalcinosis
Nephrogenic Systemic Fibrosis
Nephroptosis (Floating Kidney, Renal Ptosis)
Nephrotic Syndrome
Neurogenic Bladder
Nodular Glomerulosclerosis
Non-Gonococcal Urethritis - Wikipedia, the free encyclopedia
Nutcracker syndrome
Orthostatic Hypotension
Orthostatic Proteinuria
Osmotic Diuresis
Page Kidney
Papillary Necrosis
Papillorenal Syndrome (Renal-Coloboma Syndrome, Isolated Renal Hypoplasia)
The Peritoneal-Renal Syndrome
Posterior Urethral Valve
Post-infectious Glomerulonephritis, Post-streptococcal Glomerulonephritis
Polyarteritis Nodosa
Polycystic Kidney Disease
Posterior Urethral Valves
Preeclampsia
Propofol infusion syndrome
Proteinuria (Protein in Urine)
Pseudohyperaldosteronism
Pseudohypoparathyroidism
Pulmonary-Renal Syndrome
Pyelonephritis (Kidney Infection)
Pyonephrosis
Radiation Nephropathy
Reflux Nephropathy
Rapidly Progressive Glomerulonephritis
Renal Abscess, Peripnephric Abscess
Renal Agenesis
Renal Artery Aneurysm
Renal Artery Stenosis
Renal Cell Cancer
Renal Cyst
Renal Infarction
Renal Osteodystrophy
Renal Tubular Acidosis
Renin Secreting Tumors (Juxtaglomerular Cell Tumor)
Reset Osmostat
Retroperitoneal Fibrosis
Rhabdomyolysis, Rhabdomyolysis related to Bariatric Sugery
Rheumatoid Arthritis-Associated Renal Disease
Sarcoidosis Renal Disease
Salt Wasting, Renal and Cerebral
Schistosomiasis and Glomerular Disease
Schimke immuno-osseous dysplasia
Scleroderma Renal Crisis
Serpentine Fibula-Polycystic Kidney Syndrome, Exner Syndrome
Silica Exposure and Chronic Kidney Disease
Sjgren's Syndrome and Renal Disease
Synthetic Cannabinoid Use and Acute Kidney Injury
Kidney Disease Following Hematopoietic Cell Transplantation, Kidney Disease Related to Stem Cell
Transplantation
Thin Basement Membrane Disease, Benign Familial Hematuria
Trigonitis
Tuberous Sclerosis
Tubular Dysgenesis
Tumor Lysis Syndrome
Uremia
Uremic Optic Neuropathy
Ureterocele
Urethral Caruncle
Urethral Stricture
Urinary Incontinence
Urinary Tract Infection
Urinary Tract Obstruction
Vesicointestinal Fistula
Vesicoureteral Reflux
Von Hippel-Lindau Disease
Warfarin-Related Nephropathy
Wegeners Granulomatosis, Granulomatosis with Polyangiitis
West Nile Virus and Chronic Kidney Disease
Wunderlich syndrome
You might also like
- HGPDocument1 pageHGPLiezl SabadoNo ratings yet
- Template Career Guidance Program Action Plan Sy.20!21!1Document4 pagesTemplate Career Guidance Program Action Plan Sy.20!21!1Liezl Sabado67% (3)
- Template-No 2Document7 pagesTemplate-No 2Liezl SabadoNo ratings yet
- (Page 1) Transmittal Letter Attention: Bernadette L. Lejarde, Phd. Magc Division Career Guidance Program and Homeroom Guidance CoordinatorDocument6 pages(Page 1) Transmittal Letter Attention: Bernadette L. Lejarde, Phd. Magc Division Career Guidance Program and Homeroom Guidance CoordinatorLiezl SabadoNo ratings yet
- Department of Education: Accomplishment Report For The Month of FebruaryDocument3 pagesDepartment of Education: Accomplishment Report For The Month of FebruaryLiezl SabadoNo ratings yet
- English: Quarter 3 - Module 6: Critiquing A Literary Selection Using Structuralism and Formalism ApproachDocument20 pagesEnglish: Quarter 3 - Module 6: Critiquing A Literary Selection Using Structuralism and Formalism ApproachLiezl Sabado70% (10)
- English: Quarter 3 - Module 5Document20 pagesEnglish: Quarter 3 - Module 5Liezl Sabado100% (8)
- Template Career Guidance Program Action Plan Sy.20!21!1Document4 pagesTemplate Career Guidance Program Action Plan Sy.20!21!1Liezl Sabado67% (3)
- English: Quarter 3 - Module 1: Composing An Argumentative EssayDocument15 pagesEnglish: Quarter 3 - Module 1: Composing An Argumentative EssayMarife Magsino71% (24)
- Career Guidance Portfolio: Republic of The PhilippinesDocument1 pageCareer Guidance Portfolio: Republic of The PhilippinesLiezl Sabado100% (1)
- Template Career Guidance Program Action Plan Sy.20!21!1Document4 pagesTemplate Career Guidance Program Action Plan Sy.20!21!1Liezl Sabado67% (3)
- Career Guidance Program: Department of EducationDocument4 pagesCareer Guidance Program: Department of EducationLiezl SabadoNo ratings yet
- Department of Education: What Is A Context ClueDocument45 pagesDepartment of Education: What Is A Context ClueLiezl SabadoNo ratings yet
- Sci 10 Budget of WorkDocument4 pagesSci 10 Budget of WorkAnonymous xagGSIdNo ratings yet
- Department of Education: Accomplishment Report For The Month of JanuaryDocument3 pagesDepartment of Education: Accomplishment Report For The Month of JanuaryLiezl SabadoNo ratings yet
- LDM2 Form 1. LAC ProfileDocument1 pageLDM2 Form 1. LAC ProfileRose Merie Joy Solmia100% (1)
- Department of Education: Accomplishment Report For The Month of DecemberDocument2 pagesDepartment of Education: Accomplishment Report For The Month of DecemberLiezl SabadoNo ratings yet
- Homeroom Guidance: Quarter 1 - Module 1: Decoding The Secrets of Better Study HabitsDocument10 pagesHomeroom Guidance: Quarter 1 - Module 1: Decoding The Secrets of Better Study HabitsTeresa Marie Yap Cordero86% (21)
- GUIDE-ENGLISH 10 MODULESDocument3 pagesGUIDE-ENGLISH 10 MODULESLiezl SabadoNo ratings yet
- English: Quarter 1 - Module 1 Noting Context CluesDocument29 pagesEnglish: Quarter 1 - Module 1 Noting Context CluesMary Cris GenilNo ratings yet
- E-Class Record Data SheetDocument55 pagesE-Class Record Data SheetHECTOR RODRIGUEZNo ratings yet
- English: Quarter 1 - Module 5: Expressing Emotional Responses Using A Range of Verbs, Adjectives, and AdverbsDocument36 pagesEnglish: Quarter 1 - Module 5: Expressing Emotional Responses Using A Range of Verbs, Adjectives, and AdverbsLiezl Sabado100% (1)
- E-Class Record Data SheetDocument54 pagesE-Class Record Data SheetHECTOR RODRIGUEZNo ratings yet
- Guide-Inventory of Modules For Teachers English 8 - Quarter 1Document3 pagesGuide-Inventory of Modules For Teachers English 8 - Quarter 1Liezl SabadoNo ratings yet
- E - Class RecordDocument54 pagesE - Class RecordImee GenovateNo ratings yet
- Module 2 Study NotebookDocument6 pagesModule 2 Study NotebookLorna Narciso VallejoNo ratings yet
- Daily English Lesson on Cell Phones and PoetryDocument3 pagesDaily English Lesson on Cell Phones and PoetryLiezl SabadoNo ratings yet
- PronounDocument4 pagesPronounLiezl Sabado100% (1)
- Directions: Listen To Your Teacher As He/she Reads The Song Twice Then, Answer The Questions byDocument9 pagesDirections: Listen To Your Teacher As He/she Reads The Song Twice Then, Answer The Questions byLiezl SabadoNo ratings yet
- Feeding ProgramDocument1 pageFeeding ProgramLiezl SabadoNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Basic Pathology - Lakhani, Sunil R. (SRG)Document340 pagesBasic Pathology - Lakhani, Sunil R. (SRG)Vetési Orsolya88% (8)
- Osmoregulation in Earthworms ExplainedDocument28 pagesOsmoregulation in Earthworms ExplainedMa-anJaneDiamosNo ratings yet
- Animal TissuesDocument10 pagesAnimal TissuesAlvin PaboresNo ratings yet
- Major Intra and Extracellular ElectrolytesDocument9 pagesMajor Intra and Extracellular ElectrolytesJana BlueNo ratings yet
- GEN BIO Aug 7-11Document4 pagesGEN BIO Aug 7-11Yay SandovalNo ratings yet
- Common Questions Asked in The MRCS Viva Examination PDFDocument4 pagesCommon Questions Asked in The MRCS Viva Examination PDFWael Shoabe100% (1)
- Vce Biology Unit 1 - OutlineDocument4 pagesVce Biology Unit 1 - Outlineapi-336208185No ratings yet
- The Education Act of 1982Document5 pagesThe Education Act of 1982Julaton Jerico100% (3)
- Phed 11 2022 2023 1ST SemDocument53 pagesPhed 11 2022 2023 1ST SemNicole CanoNo ratings yet
- Trimitere-Extras* Н А П Р А В Л Е Н И Е - В Ы П И С К А: Ministerul Sănătăţii al RM Министерство здравоохранения РМDocument16 pagesTrimitere-Extras* Н А П Р А В Л Е Н И Е - В Ы П И С К А: Ministerul Sănătăţii al RM Министерство здравоохранения РМNatașa ProdanNo ratings yet
- Students Hand Out Notes in Anatomy and PhysiologyDocument73 pagesStudents Hand Out Notes in Anatomy and PhysiologyCza Mae Arsenal100% (1)
- Homeostasis Lab Effects Exercise Heart RateDocument4 pagesHomeostasis Lab Effects Exercise Heart Ratethe cornchip executionerNo ratings yet
- An Introduction To Anatomy and Physiology MidwiferyDocument108 pagesAn Introduction To Anatomy and Physiology MidwiferyGayuh Kartika100% (3)
- Chapter 2.2-2.3Document15 pagesChapter 2.2-2.3Gerard Bio100% (2)
- Excretion and Homeostasis: Maintaining the Body's Internal BalanceDocument11 pagesExcretion and Homeostasis: Maintaining the Body's Internal BalancestarcandypricessNo ratings yet
- Medical Physiology, Boron, Boulpaep 812Document13 pagesMedical Physiology, Boron, Boulpaep 812Kristijan Goldašić0% (1)
- FOR5MODULEDocument6 pagesFOR5MODULEQueenda Arcibal100% (1)
- Endocrine System Chapter SummaryDocument6 pagesEndocrine System Chapter SummaryShiny ChenNo ratings yet
- Control Systems - KeyDocument2 pagesControl Systems - KeySamra ShahzadNo ratings yet
- Why Is Homeostasis So Important To Living OrganismsDocument8 pagesWhy Is Homeostasis So Important To Living OrganismsYeehong OngNo ratings yet
- Homeostasis and Immune SystemsDocument26 pagesHomeostasis and Immune Systemsshintarolle 2000No ratings yet
- 01 - Human OrganismDocument11 pages01 - Human OrganismCristine Grace Neo SapicoNo ratings yet
- Treatingt Troubled AdolescentsDocument254 pagesTreatingt Troubled AdolescentsSasu Nicoleta100% (1)
- (Modern Biology Series) Eugene Pleasants Odum-Ecology, The Link Between The Natural and The Social Sciences-Holt, Rinehart and Winston (1975) PDFDocument260 pages(Modern Biology Series) Eugene Pleasants Odum-Ecology, The Link Between The Natural and The Social Sciences-Holt, Rinehart and Winston (1975) PDFsinhababusounak100% (1)
- Principles of HomeostasisDocument31 pagesPrinciples of Homeostasisleeminhoangrybird100% (1)
- AIIMS June 2020 - Physiology SolvedDocument2 pagesAIIMS June 2020 - Physiology SolvedDoctor planet global instituteNo ratings yet
- Homeostasis..answer Key WorksheetDocument4 pagesHomeostasis..answer Key WorksheetUCL SportsNo ratings yet
- Powerful Words to Connect to Your Subconscious MindDocument37 pagesPowerful Words to Connect to Your Subconscious Mindceciliaalfonso_cna4935100% (1)
- Thermoregulation To Maintain HomeostasisDocument2 pagesThermoregulation To Maintain HomeostasisMay TranNo ratings yet
- The AnswersDocument3 pagesThe AnswersSHAHD WALIDNo ratings yet