Professional Documents
Culture Documents
101 Full PDF
Uploaded by
Sava1988Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
101 Full PDF
Uploaded by
Sava1988Copyright:
Available Formats
A prospective comparison of class IA, B, and C antiarrhythmic agents in combination
with amiodarone in patients with inducible, sustained ventricular tachycardia.
L Toivonen, A Kadish and F Morady
Circulation. 1991;84:101-108
doi: 10.1161/01.CIR.84.1.101
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright 1991 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/84/1/101
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/
Downloaded from http://circ.ahajournals.org/ by guest on November 21, 2014
101
A Prospective Comparison of Class IA, B,
and C Antiarrhythmic Agents in Combination
With Amiodarone in Patients With Inducible,
Sustained Ventricular Tachycardia
Lauri Toivonen, MD; Alan Kadish, MD; and Fred Morady, MD
Background. Clinical experience suggests that combinations of antiarrhythmic agents
provide more effective control of ventricular tachyarrhythmias than does therapy with single
agents.
Methods and Results. Antiarrhythmic and electrophysiological effects of three class I
antiarrhythmic agents, one from each subclass A, B, and C, were assessed in single use and
in combination with amiodarone in patients with inducible, sustained ventricular tachycardia that was not suppressed by monotherapy with these agents. Thirty-one patients
underwent an electrophysiology test on four occasions: at baseline; after 2-4 days of
treatment with quinidine, mexiletine, or encainide; after 2 weeks of treatment with 1,200
mg/day amiodarone; and last, after 2-4 days of treatment with both amiodarone and the
previously tested class I agent. The combination of a class I agent and amiodarone prevented
the induction of sustained ventricular tachycardia in only one of 31 (3%) patients.
Ventricular tachycardia became hemodynamically stable in 11 of 31 (34%) patients because
of a marked prolongation in the tachycardia cycle length. It increased from 323+39 to
423+84 msec (n = 11, p<0.01) by adding encainide to amiodarone therapy, and it showed a
tendency to lengthen when quinidine was added to amiodarone (from 373 77 to 42558
msec; n=10, NS). Each class I agent increased amiodarone-induced depression in myocardial conduction, but the extent of the additional depression seemed to differ among the three
subclasses. Ventricular refractoriness was increased by all class I agents when used in
combination with amiodarone, although not by mexiletine or encainide when used alone.
Conclusions. Class I antiarrhythmic agents slow ventricular conduction and increase
ventricular refractoriness when used in combination with amiodarone. When amiodarone
and class I drugs by themselves do not suppress the induction of ventricular tachycardia, the
combination of amiodarone and a class I agent seldom results in noninducibility; however,
it often lengthens the ventricular tachycardia cycle length and may render the ventricular
tachycardia hemodynamically stable. (Circulation 1991;84:101-108)
linical experience suggests that combinations
of antiarrhythmic agents provide more effective control of ventricular tachyarrhythmias
than does therapy with single agents.1-3 For example, the combination of a class I agent with amiodarone has been shown to suppress the induction of
sustained ventricular tachycardia when amiodarone
alone is ineffective.4 The addition of a class I agent
to amiodarone therapy has also been demonstrated
C
From the Division of Cardiology, Department of Internal Medicine, University of Michigan Medical Center, Ann Arbor.
Address for correspondence: Lauri Toivonen, MD, Helsinki
University Central Hospital, First Department of Medicine,
Haartmaninkatu 4, SF-00290 Helsinki, Finland.
Received August 2, 1990; revision accepted February 26, 1991.
to result in slowing of the rate of induced ventricular tachycardia.5-7 However, no prior studies have
compared the electrophysiological effects of the
various types of class I agents in combination with
amiodarone.
The aim of this prospective study was to compare
See p 429
the effects of class I agents in combination with
amiodarone to determine the regimen most likely to
improve the therapeutic response when amiodarone
by itself is ineffective. One agent from each subclass8,9 was used: quinidine from subclass A, mexiletine from subclass B, and encainide from subclass C.
Their effects were assessed individually and in com-
Downloaded from http://circ.ahajournals.org/ by guest on November 21, 2014
102
Circulation Vol 84, No 1 July 1991
bination with amiodarone in patients with inducible,
sustained ventricular tachycardia.
Methods
Characteristics of Subjects
The subjects of this study were selected from a
pool of 72 consecutive patients who were referred for
the evaluation and treatment of ventricular arrhythmias and who had inducible, sustained monomorphic
ventricular tachycardia during a clinically indicated
electrophysiology test. A class I agent was administered in all patients, and electrophysiological testing
was performed in 67. Sustained ventricular tachycardia was not inducible in 12 patients. Among the
remaining patients, 48 were then treated with amiodarone, and 46 of these underwent electrophysiological testing. Eleven patients had a favorable response,
and a combination regimen was started in the remaining 35 patients. An electrophysiology test was
then performed in 31 patients, and these patients
make up the population of the present study.
There were 30 men and one woman, and their
mean (+SD) age was 629 years. All patients had
coronary artery disease and a history of remote
myocardial infarction. The mean left ventricular ejection fraction, determined by contrast or radionuclide
ventriculography, was 0.29+0.09 (range, 0.15-0.40).
The presenting arrhythmia was sustained, monomorphic ventricular tachycardia in 14 patients; cardiac
arrest with documented ventricular fibrillation in
three patients; symptomatic, nonsustained monomorphic ventricular tachycardia in 10 patients; and unexplained syncope in four patients.
Electropharmacological Testing Protocol
After sustained, monomorphic ventricular tachycardia was induced during a baseline electrophysiology test, oral therapy was started with quinidine,
mexiletine, or encainide. The choice of the antiarrhythmic agent was random, except that agents that
had caused adverse effects or that had failed on a
clinical basis to control the patient's arrhythmia were
not used. If sustained ventricular tachycardia was
inducible despite treatment with the class I agent,
therapy with amiodarone was initiated. If sustained
and hemodynamically unstable ventricular tachycardia was still inducible, the previously used class I
antiarrhythmic agent was used in combination with
amiodarone.
In assessing the therapeutic response to an antiarrhythmic regimen, the noninducibility of ventricular
tachycardia and the induction of nonsustained or
hemodynamically stable sustained ventricular tachycardia were considered to be adequate therapeutic
end points. Ventricular tachycardia with a cycle
length of more than 400 msec and a mean arterial
pressure of 80 mm Hg or more was considered hemodynamically stable.
The daily dosages of quinidine, mexiletine, and
encainide were 1,460-1,940 mg (quinidine glu-
conate), 600-750 mg, and 105-150 mg, respectively,
and were given orally in three divided daily doses at
8-hour intervals. The daily dosage of amiodarone was
1,200 mg during the loading period. The electrophysiology study was performed after at least 2 days of
therapy with quinidine and mexiletine and after 4
days of treatment with encainide, either when used
alone or in combination with amiodarone, and after
14 days of treatment with amiodarone. Electrophysiological testing was performed during the last hour
of the dosing interval, and the blood samples for
determination of the plasma drug concentrations
were drawn at the end of the test.
Programmed Electrical Stimulation
The study protocol was approved by the Human
Research Committee at the University of Michigan.
Electrophysiology tests were performed in the fasting, unsedated state after informed consent was
obtained. The baseline studies were performed at
least five half-lives after discontinuation of treatment
with all antiarrhythmic medications.
Two quadripolar electrode catheters were positioned in the right atrium and across the tricuspid
valve to record the atrioventricular conduction intervals during sinus rhythm and atrial pacing, then were
advanced to the right ventricle. A short SF cannula
that was inserted into a femoral artery was used to
continuously record the arterial pressure. Leads I,
III, and V1 and the intracardiac electrograms were
recorded on a Mingograf 7 recorder (SiemensElema, Solna, Sweden) at a paper speed of 100-200
mm/sec. Stimulation was performed with a programmable stimulator (Bloom Associates, Reading, Pa.)
with an impulse duration of 2 msec and a current
intensity of twice the late diastolic threshold, which
was always 1 mA or less.
The AH, HV, and QT intervals were measured
during sinus rhythm and atrial pacing at a cycle
length of 600 msec. The QT interval was corrected
for heart rate with Bazett's method. The ventricular
effective refractory period was determined with an
eight-beat basic drive train at cycle lengths of 600 and
400 msec and with 5-msec decrements in the extrastimulus coupling interval. The duration of the QRS
complex during ventricular pacing was determined
after 15 cycles of pacing from the right ventricular
apex at cycle lengths of 600 and 350 msec.
Programmed stimulation to induce ventricular tachycardia was performed at the right ventricular apex and
outflow tract with drive cycle lengths of 600 and 400
msec. One and two extrastimuli were delivered at
both ventricular sites and drive cycle lengths, after
which three extrastimuli were delivered. The coupling intervals of the extrastimuli were shortened in
steps of 10 msec. Ventricular tachycardia lasting at
least 30 seconds or requiring prompt termination was
considered sustained.
Downloaded from http://circ.ahajournals.org/ by guest on November 21, 2014
Toivonen et al Amiodarone Combined With Class I Drugs
103
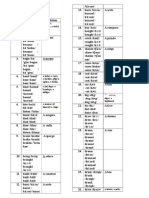
TABLE 1. Patients With Combined Antiarrhythmic Treatment and Responses in the Electrophysiology Studies
Antiarrhythmic
Electrophysiology
test result
combination
Noninducible
Sustained VT
Started
Tested*
Sustained VT
(n)
stablet (n)
(n)
(n)
(n)
Patients receiving class I agents
0
6
10
10
10
Quinidine
1
1
13
10
9
Mexiletine
0
4
12
11
11
Encainide
31
30
1
11
All patients
35
VT, ventricular tachycardia.
*Not tested in four patients because of side effects: central nervous system side effects in three patients receiving
mexiletine and worsening of heart failure in one patient receiving encainide.
tSustained ventricular tachycardia with a cycle length of more than 400 msec and mean blood pressure 80 mm Hg
or more.
Statistical Analysis
A two-way analysis of variance with repeated measures was used to compare differences in continuous
variables during various treatment phases. A Wilcoxon's signed-rank test was used to analyze changes in
the number of extrastimuli required to induce ventricular tachycardia. Linear regression analysis was
used to examine correlations between electrophysiological variables and ventricular tachycardia cycle
length. Continuous variables are expressed as
mean+ SD. Ap value less than 0.05 was considered to
be statistically significant.
Results
Effects on Ventricular Tachycardia
Noninducibility of sustained ventricular tachycardia
was achieved in one of 31 patients with a combination
of a class I agent (mexiletine) and amiodarone. Ventricular tachycardia became hemodynamically stable
in 11 patients during combination therapy (Table 1).
The number of extrastimuli required to induce
sustained ventricular tachycardia decreased during
combination therapy compared with treatment with a
TABLE 2. Cycle Length of Induced Ventricular Tachycardia
Treatment group (n)
Quinidine Mexiletine Encainide All groups
(10)
(9)
(11)
(30)
Control phase 26427
26339
28163
27045
Test phase
agent
310)48
+ 17%t
+12%
30451
30859
Amiodarone
37377
32451
+18%*
Class
+29%t
32339
34060
+36%*
+13%
+6%
42384
36281
Combination 425+58
The ventricular tachycardia cycle length (mean+SD) is given in
msec. Changes from the control phase and from the amiodarone
phase are indicated in percentages.
Comparison is performed between the baseline and the class I
agent phase and between the amiodarone and the combination
phases in the three parallel treatment groups. In addition, the
amiodarone phase is compared with the baseline in the whole
group.
*p<0.01, tp<0.05, tp<0.001.
class I agent only, from an average of 2.4 to 1.9
(p<0.O5).
Quinidine and mexiletine increased the tachycardia
cycle length, whereas no significant change occurred
with encainide (Table 2). The greatest increase occurred with amiodarone. Encainide increased the
tachycardia cycle length when combined with amiodarone. Overall, quinidine and mexiletine had no
significant additive effect on the tachycardia cycle
length in combination with amiodarone. However,
individual responses varied within treatment groups.
In 12 of 30 patients, the morphology of the induced
ventricular tachycardia was identical in all four study
phases (in 3, 4, and 5 patients in the quinidine,
mexiletine, and encainide groups, respectively). In 18
patients, it was different during at least one of the
phases. The cycle length of the induced ventricular
tachycardia increased in patients with an identical
tachycardia morphology from 270+44 at baseline to
31047, 337+60 and 423+88 msec during treatment
with a class I agent, amiodarone, and a combination,
respectively. The cycle lengths increased from
268+48 to 306+52, 343+63, and 39472 msec in the
respective phases in patients with nonidentical tachycardia morphologies. The cycle lengths did not differ
significantly between these two subgroups.
Effects on Ventricular Conduction and Refractoriness
The duration of the paced QRS complex was
prolonged by each class I agent and amiodarone
(Table 3). The degree of prolongation was similar,
except with mexiletine, which had the least effect.
The increase in the duration of the paced QRS
complex during treatment with the class I agents was
not rate dependent. In contrast, amiodarone had a
greater effect at a cycle length of 350 than at 600
msec (p<0.001). When used with amiodarone, all
class I agents increased further the duration of the
paced QRS complex. The increase was greater with
encainide than with quinidine and mexiletine. The
additive effects of the class I agents on the QRS
duration during combination therapy were not dependent on rate (Table 3).
Downloaded from http://circ.ahajournals.org/ by guest on November 21, 2014
104
Circulation Vol 84, No 1 July 1991
TABLE 3. Duration of the Paced QRS Complex
Quinidine
Test phase
Pacing cycle length, 600 msec
Control phase
Class I agent
Amiodarone
Combination
Pacing cycle length, 350 msec
Control phase
Class I agent
(10)
Treatment groups (n)
Mexiletine
Encainide
(10)
(11)
+23%*
20520
16816
+5%t
17720
16831
+22%
202+27
21229
+7%t
22630
19622
+6%*
20824
19532
+16%t
22536
16816
+28%*
21419
16719
+7%t
17923
17032
+23%X
20635
16822
All groups
(31)
16823
+20%*
20128
16823
+30%*
21835
21530
20538
23534
+ 19%*
+7%
+8%t
24848
24931
22936
Combination
Duration of the QRS complex (mean+SD) is given in msec. Changes from the control phase and from the
amiodarone phase are indicated in percentages.
Comparison is performed between the baseline and the class I agent phase and between the amiodarone and the
combination phases in the three parallel treatment groups. In addition, the amiodarone phase is compared with the
baseline in the whole group.
Amiodarone
*p<0.001, tp<0.05, tp<0.01.
The ventricular effective refractory period was
prolonged by quinidine and amiodarone (Table 4).
The changes were similar with the 600- and 400 -msec
drive cycle lengths. Mexiletine and encainide by
themselves did not increase refractoriness. In combination, encainide increased the amiodarone-induced
prolongation in the ventricular effective refractory
period determined at both drive cycle lengths. At the
400-msec drive cycle length, quinidine and mexiletine in combination with amiodarone also prolonged
ventricular refractoriness (Table 4). Therefore, each
of the class I agents increased the ventricular effective refractory period when used in combination with
amiodarone and each tended to do so more at a drive
cycle length of 400 than at 600 msec.
The cycle length of induced ventricular tachycardia
correlated with the ventricular effective refractory
period (basic drive cycle length, 400 msec) during
treatment with amiodarone (r=0.51, n =31, p <0.001)
but not with the class I agents. The duration of the
paced QRS complex did not correlate with the
tachycardia cycle length during any treatment regimen, even when the analysis was restricted to identical tachycardia morphologies.
Inclusion only of patients who had an ineffective
response in the next study phase may have biased the
assessment of the electrophysiological variables if the
efficacy was related to the extent of the electrophysiological changes. In this respect, nine patients who
responded to quinidine were compared with 15 nonresponders, and 11 patients who responded to amiodarone were compared with 35 nonresponders. The
success rate with mexiletine and encainide was not
sufficient for a similar analysis. There were no statistically significant differences between the responders and nonresponders in the duration of the paced
QRS complex, ventricular effective refractory period, and the QT interval.
Electrocardiographic Variables, Atrioventricular
Conduction, Blood Pressure, and Adverse Reactions
The sinus cycle length was increased by amiodarone from 780+40 to 880+170 msec (n=31,
p<0.001). The class I agents had no significant influence on the sinus cycle length when used alone or in
combination with amiodarone. The AH interval was
not affected by the class I agents during monotherapy. It was increased by amiodarone from 108 39 to
192+72 msec (n=21, p<0.001) during atrial pacing.
In combination, only encainide increased the AH
interval, from 195+79 msec with amiodarone alone
to 222+ 94 msec in combination (n=9, p<0.05). The
HV interval was increased by encainide from 55 + 13
to 67+22 msec (n=9, p<0.05) and by amiodarone
from 53+11 to 64+15 msec (n-21,p<0.001) during
atrial pacing. During combination of encainide and
amiodarone the HV interval was further increased,
to 74+20 msec (n=9,p<0.05). No significant changes
occurred in the HV interval during quinidine or
mexiletine.
The QT interval during sinus rhythm was prolonged from 388+30 to 44239 msec by quinidine
(n=10,p<0.001) and to 47140 msec by amiodarone
(p<0.001), but their combination did not result in a
Downloaded from http://circ.ahajournals.org/ by guest on November 21, 2014
Toivonen et al Amiodarone Combined With Class I Drugs
105
TABLE 4. Ventricular Effective Refractory Period
Test phase
Drive cycle length, 600 msec
Control phase
Class I agent
Amiodarone
Combination
Quinidine
(8)
Treatment groups (n)
Encainide
Mexiletine
(9)
(9)
25120
+9%*
27621
25823
-0%
25718
26119
+2%
26525
29423
+6%
30732
28013
+3%*
28834
28915
+6%*
30821
All groups
(26)
25521
+12%t
28519
Treatment groups (n)
Test phase
Drive cycle length, 400 msec
Control phase
Quinidine
(8)
23417
+9%:t
25517
Class I agent
Mexiletine
(10)
Encainide
(9)
All groups
(27)
24119
-1%
23713
23715
+6%
24925
23717
258+16
268+14
+7%*
26417
+12%t
Amiodarone
27023
+ 10%t
29430
+4%*
Combination
27120
28921
Ventricular effective refractory period (meanSD) is given in msec. Changes from the control phase and from the
amiodarone phase are indicated in percentages.
Comparison is performed between the baseline and the class I agent phase and between the amiodarone and the
combination phases in the three parallel treatment groups. In addition, the amiodarone phase is compared with the
baseline in the whole group.
*p<0.01, tp<O.001, tp<0.05.
further increase (477+t60 msec, NS). Neither mexiletine nor encainide prolonged the QT interval when
added to amiodarone therapy. The findings were
basically similar with the corrected QT interval.
The class I antiarrhythmic agents had no significant effect individually or in combination with amiodarone on the mean arterial pressure during sinus
rhythm. The mean arterial pressure increased during
amiodarone therapy from 90+ 13 to 95+ 14 mm Hg
(p<0.001). No proarrhythmic events occurred during
combination therapy.
Plasma Drug Concentrations
The mean plasma amiodarone concentration was
1.7+0.5 mg/l after 14 days of therapy and was
1.7+0.6 mg/l during combination therapy. The respective plasma desethylamiodarone concentrations
were 0.9+0.3 and 1.0+0.2 mg/i. The mean plasma
quinidine concentration was 2.3+0.7 mg/l during
monotherapy and was 2.7+0.7 mg/i during combination therapy. The mean plasma mexiletine concentration was 0.7+0.2 mg/l during monotherapy and
was 0.70.3 mg/l during combination therapy. The
mean plasma encainide concentration was 3020
ng/l during monotherapy and 4020 ng/l during
combination therapy. The respective concentrations
during monotherapy and combination therapy were
13060 and 14060 ng/l for O-desmethyl encainide
and 13070 and 13070 ng/l for 3-methoxy-Odesmethyl encainide. Only the plasma quinidine concentration differed significantly (p<0.05) between
monotherapy and combination therapy.
Discussion
Main Findings
In this prospective study, the electrophysiological
and antiarrhythmic effects of quinidine, mexiletine,
and encainide were assessed in combination with
amiodarone in patients who had inducible, sustained
ventricular tachycardia. The design of the study allowed a comparison of the individual effects of class
IA, B, and C antiarrhythmic agents with their effects
in combination with amiodarone in the same patients.
Amiodarone-induced slowing of myocardial conduction was accentuated by agents from all subclasses but most prominently by the class IC agent,
encainide. This indicates that, when used in combination, the class I agents and amiodarone both
contribute to depression of myocardial conduction,
consistent with blockade of sodium channels.10
Agents from all subclasses also had an additive effect
on ventricular refractoriness when combined with
amiodarone. Both mexiletine and encainide potenti-
Downloaded from http://circ.ahajournals.org/ by guest on November 21, 2014
106
Circulation Vol 84, No 1 July 1991
ated the effect of amiodarone on the ventricular
effective refractory period; however, neither agent
had an effect on refractoriness when used alone.
The combination of a class I agent with amiodarone
rarely resulted in the noninducibility of ventricular
tachycardia when the individual agents were ineffective
in suppression of induction of ventricular tachycardia.
However, quinidine and encainide in combination with
amiodarone markedly decreased the rate of ventricular
tachycardia and often resulted in unstable ventricular
tachycardia becoming hemodynamically stable. This
may be a clinically significant effect because prior
studies demonstrated that hemodynamically stable ventricular tachycardia is an adequate therapeutic end
point in patients treated with amiodarone."11,2
Effects on Conduction
Quinidine and encainide slowed myocardial conduction (as reflected in the paced QRS duration)
more than mexiletine did. The depression in conduction was similar at slow and fast rates, although
quinidine tended to have a greater effect during the
faster rate. Class I agents should demonstrate usedependent slowing of myocardial conduction during
ventricular pacing,10'13 but the methods used in the
present study may not have been accurate enough to
detect small changes with statistical significance.
Amiodarone prolonged the paced QRS complex to a
greater extent at the faster rate, indicating a rate
dependency that is consistent with the known usedependent properties of amiodarone.14,15
The additional depression of myocardial conduction produced by combining mexiletine and encainide to amiodarone was equal to the individual effect
of these drugs. In contrast, the slowing of conduction
produced by combining quinidine to amiodarone was
less than quinidine's individual effect.
Antiarrhythmic subclasses IA, B, and C differ in
respect to their time constants of sodium channel
blockade.8-10'16-18 The subclass B has the fastest,
subclass A has an intermediate, and subclass C has
the slowest kinetics. Amiodarone inhibits the sodium
channel by binding to the receptors in the inactivated
state, has rapid recovery kinetics, and also prolongs
the duration of the action potential.'4"15 It has been
hypothesized that antiarrhythmic agents that have
rapid recovery constants competitively inhibit the
sodium channel blockade exerted by agents with
slower kinetics.7'19-21 Amiodarone may, therefore,
inhibit the depression of myocardial conduction by
quinidine and encainide. This can explain why the
slowing of conduction in the ventricular muscle during the combination of quinidine and amiodarone
was less than the sum of their individual effects.
However, similar attenuation of the combined effect
was not seen with encainide, which also has slow
kinetics.9"16'22-24 This difference may be caused by the
state of the sodium channel on which the drugs exert
their influence. Encainide affects sodium channels
when they remain inactivated during the plateau of
the action potential,9,2223 whereas quinidine affects
open channels.1718 Therefore, amiodarone-induced
prolongation in the duration of the action potential
may enhance the effect of encainide. Amiodarone
should not markedly change the effect of mexiletine
because both have rapid kinetics.14'52526 Accordingly, their combined effect on conduction was equal
to the sum of their individual effects.
Effects on Refractoriness and Repolarization
Ventricular refractoriness was prolonged by agents
from all three subclasses in combination with amiodarone. Of note is that encainide and mexiletine,
when used by themselves, did not lengthen the
ventricular effective refractory period either in the
present or in previous studies.22,25,27 Therefore, the
effects on ventricular refractoriness may represent
complex pharmacodynamic interactions that are not
equivalent to the sum of the effects of the individual
drugs.
Combining quinidine with amiodarone did not
further prolong the QT interval and did not result in
proarrhythmia. Therefore, the combination of antiarrhythmic agents from classes IA and III may not
markedly accentuate the risk of provoking ventricular
arrhythmias associated with a long QT interval.28'29
In addition, neither of the other combinations resulted in adverse electrophysiological effects, although the HV conduction time was further prolonged by encainide.
Role of Drug Metabolites
The pharmacological influence of oral administration of encainide is exerted mainly by its metabolites
O-desmethyl encainide and 3 -methoxy-O-desmethyl
encainide, which are electrophysiologically similar to
encainide.23'24 The metabolites accumulate to produce steady plasma concentrations within 4 days. The
main metabolite of amiodarone, desethylamiodarone, has electropharmacological properties similar to amiodarone, except it depresses the sodium
channel to a greater extent.30,3' A stable ratio of this
metabolite and the parent compound is achieved
within 2 weeks.32
The metabolism of the class I agents can be
influenced by amiodarone33 which may distort the
comparison of their individual and combined pharmacological effects. However, in the present study,
only the quinidine plasma concentration was higher
during combination therapy than during monotherapy and only by a mean of 0.4 mg/l.
Antiarrhythmic Efficacy
Suppression of the induction of sustained ventricular tachycardia during electropharmacological testing is predictive of long-term antiarrhythmic drug
efficacy.1"34 A marked reduction in the tachycardia
rate resulting in hemodynamic stability of the ventricular tachycardia suggests protection from arrhythmia-related mortality, although not necessarily from
arrhythmia recurrence.11,12
Downloaded from http://circ.ahajournals.org/ by guest on November 21, 2014
Toivonen et al Amiodarone Combined With Class I Drugs
Although only 3% of patients became noninducible, 34% of patients achieved hemodynamic stability
of ventricular tachycardia during combination therapy. The results of this study indicate that the
potential to slow the tachycardia rate may be greater
with quinidine and encainide than with mexiletine.
Limitations of the Study
Evaluation of the effects of combination therapy
may have been influenced by 2-4 additional days of
therapy with amiodarone. However, given the known
time course of the onset of the electropharmacological effects of amiodarone,3235'36 the observed
changes in cardiac effects between the amiodarone
and the combination phases cannot be attributed to
2-4 days of additional therapy with amiodarone. The
antiarrhythmic effect of amiodarone requires several
weeks to reach its maximum32,34,35
The efficacy of combination therapy may have
been underestimated because only agents that failed
in monotherapy were evaluated in combination. Nevertheless, the present findings are relevant to clinical
practice because antiarrhythmic combinations are
generally used only when therapy with single agents
is ineffective.
A limitation of this study is that the outcome of
long-term combination therapy was not examined. A
later deterioration in cardiac function by the negative
inotropic effect of the drugs and a possible late
incidence of proarrhythmia37 may counteract the
initial beneficial effects of combination therapy.
Therefore, the long-term outcome of the combination therapy needs further study.
Clinical Implications
This study demonstrates that the combination of
class I antiarrhythmic agents with amiodarone can be
helpful in the management of patients with inducible,
sustained ventricular tachycardia. Noninducibility is
rarely achieved, but the rate of the tachycardia often
becomes markedly slower. An improvement in hemodynamic stability during ventricular tachycardia may
be likely, especially when agents from subclasses IA
and IC are added to amiodarone. The relatively small
population size in this study does not exclude the
possibility of adverse electropharmacological and
proarrhythmic effects with combination therapy.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
References
1. Duff HJ, Mitchell LB, Manyari D, Wyse GD: Mexiletinequinidine combination: Electrophysiologic correlates of a
favorable antiarrhythmic interaction in humans. J Am Coll
Cardiol 1987;10:1149-1156
2. Levy S: Combination therapy for cardiac arrhythmias. Am J
Cardiol 1988;61:95A-1O1A
3. Whitford EG, McGovern B, Shoenfeld MH, Garan H, Newell
JB, McElroy M, Ruskin JN: Long-term efficacy of mexiletine
alone and in combination with class Ia antiarrhythmic drugs
for refractory ventricular arrhythmias. Am Heart J 1988;115:
360-366
4. Bellocci F, Santarelli P, Montenero A, Giasiolla F, Nobile A:
Value of electrophysiologic testing of amiodarone alone or in
19.
20.
21.
107
combination with class I antiarrhythmic drugs for ventricular
tachycardia (abstract). Circulation 1985;72(suppl II):II-274
Marchlinski FE, Buxton AE, Josephson ME, Schmitt C:
Predicting ventricular tachycardia cycle length after procainamide by assessing cycle length-dependent changes in paced
QRS duration. Circulation 1989;79:39-46
Marchlinski FE, Buxton AE, Kindwall KE, Miller JM,
Rosenthal ME, Gottlieb CD, Bloom RB, Josephson ME:
Comparison of individual and combined effects of procainamide and amiodarone in patients with sustained ventricular
tachyarrhythmias. Circulation 1988;78:583-591
Waxman HL, Groh WC, Marchlinski FE, Buxton AE, Sadowski LM, Josephson ME, Kastor JA: Amiodarone for
control of sustained ventricular tachycardia. Am J Cardiol
1982;50:1066-1070
Vaughan Williams EM: A classification of antiarrhythmic
actions reassessed after a decade of new drugs. J Clin Pharmacol 1984;24:129-147
Campbell TJ: Kinetics of onset of rate-dependent effects of
class I antiarrhythmic drugs are important in determining their
effects on refractoriness in guinea-pig ventricle, and provide a
theoretical basis for their subclassification. Cardiovasc Res
1983;17:344-352
Buchanan JW, Saito T, Gettes LS: The effects of antiarrhythmic drugs, stimulation frequency, and potassium-induced resting membrane potential changes on conduction velocity and
dV/dt(max) in guinea-pig myocardium. Circ Res 1985;56:
696-703
Waller TJ, Kay HR, Spielman SR, Kutalek SP, Greenspan
AM, Horowitz LN: Reduction in sudden death and total
mortality by antiarrhythmic therapy evaluated by electrophysiologic drug testing: Criteria of efficacy in patients with
sustained ventricular tachyarrhythmia. JAm Coll Cardiol 1987;
10:83-89
Kadish AH, Buxton AE, Waxman HL, Flores B, Josephson
ME, Marchlinski FE: Usefulness of electrophysiologic study to
determine the clinical tolerance of arrhythmia recurrences
during amiodarone therapy. JAm Coll Cardiol 1987;10:90-96
Morady F, DiCarlo LA, Baerman JM, Krol RB: Ratedependent effects of intravenous lidocaine, procainamide and
amiodarone on intraventricular conduction. JAm Coll Cardiol
1985;6:179-185
Mason JW, Hondeghem LM, Katzung BG: Block of inactivated sodium channels and of depolarization-induced automaticity in guinea-pig papillary muscle by amiodarone. Circ Res
1984;55:277-285
Anderson KP, Walker R, Dustman T, Lux RL, Ershler PR,
Kates RE, Urie PM: Rate-related electrophysiologic effects of
long-term administration of amiodarone on canine ventricular
myocardium in vivo. Circulation 1989;79:948-958
Campbell TJ: Resting and rate-dependent depression of depolarization (Vm,,.) in guinea pig ventricular action potentials by
mexiletine, disopyramide, and encainide. J Cardiovasc Pharmacol 1983;5:291-296
Courtney KR: Review: Quantitative structure/activity relations based on use-dependent block and repriming kinetics in
myocardium. J Mol Cell Cardiol 1987;19:319-330
Packer DL, Grant AO, Strauss HC, Starmer CF: Characterization of concentration- and use-dependent effects of quinidine from conduction delay and declining conduction velocity
in canine Purkinje fibers. J Clin Invest 1989;83:2109-2119
Clarkson CW, Hondeghem LM: Evidence for a specific receptor site for lidocaine, quinidine, and bupivacaine associated
with cardiac sodium channels in guinea pig ventricular myocardium. Circ Res 1985;56:496-506
Sheldon RS, Hill RJ, Duff HJ: Antiarrhythmic drugs and the
cardiac sodium channel: Current models. Clin Chem 1989;35:
748-754
Clarkson CW, Hondeghem LM: Electrophysiologic evidence
that local anesthetics and antiarrhythmic drugs bind to a
specific receptor site in cardiac sodium channels: Displacement of bupivacaine by lidocaine. Proc West Pharmacol Soc
1984;27:23-25
Downloaded from http://circ.ahajournals.org/ by guest on November 21, 2014
108
Circulation Vol 84, No 1 July 1991
22. Carey EL, Duff HJ, Roden DM, Primm RK, Wilkinson GR,
Wang T, Oates JA, Wooseley RL: Encainide and its metabolites: Comparative effects in man on ventricular arrhythmia
and electrocardiographic intervals. J Clin Invest 1984;73:
539-544
23. Barbey JT, Thompson KA, Echt DS, Woosley RL, Roden
DM: Antiarrhythmic activity, electrocardiographic effects and
pharmacokinetics of the encainide metabolites O-desmethyl
encainide and 3-methoxy-O-desmethyl encainide in man. Cir-
culation 1988;77:380-391
24. Roden DM, Lee JT, Woosley RL, Echt DS: Antiarrhythmic
efficacy, clinical electrophysiology, and pharmacokinetics of
3-methoxy-O-desmethyl encainide (MODE) in patients with
inducible ventricular tachycardia or fibrillation. Circulation
1989;80:1247-1258
25. Hohnloser SJ, Weirich J, Antoni H: Effects of mexiletine on
steady-state characteristics and recovery kinetics of V(max)
and conduction velocity in guinea pig myocardium. J Cardiovasc Pharmacol 1982;4:232-239
26. Valenzuela C, Sanchez-Chapula J: Electrophysiologic interactions between mexiletine-quinidine and mexiletine-ropitoin in
guinea pig papillary muscle. J Cardiovasc Phannacol 1989;14:
783-789
27. Campbell RWF: Mexiletine. N Engl J Med 1987;316:29-34
28. Bauman JL, Bauernfeind RA, Hoff JV, Strasberg B, Swiryn S,
Rosen KM: Torsade de pointes due to quinidine: Observations
in 31 patients. Am Heart J 1984;107:425-430
29. Sclarowsky S, Lewin RF, Kracoff 0: Amiodarone-induced
polymorphous ventricular tachycardia. Am Heart J 1983;105:
6-12
30. Yabek SM, Kato R, Singh BN: Effects of amiodarone and its
metabolite, desethylamiodarone, on the electrophysiologic
properties of isolated cardiac muscle. J Cardiovasc Pharmacol
1986;8:197-207
31. Talajic M, DeRoode MR, Nattel S: Comparative electrophysiologic effects of intravenous amiodarone and desethylamiodarone in dogs: Evidence for clinically relevant activity of the
metabolite. Circulation 1987;75:265-271
32. Mitchell LB, Wyse DG, Gillis AM, Duff HJ: Electropharmacology of amiodarone therapy initiation: Time courses of onset
of electrophysiologic and antiarrhythmic effects. Circulation
1989;80:34-42
33. Saal AK, Werner JA, Greene HL, Sears GK, Graham EL:
Effect of amiodarone on serum quinidine and procainamide
levels. Am J Cardiol 1984;53:1264-1267
34. Wilber DJ, Garan H, Finkelstein D, Kelly E, Newell J,
McGovern B, Ruskin JN: Out-of-hospital cardiac arrest: Use
of electrophysiologic testing in the prediction of long-term
outcome. N Engl J Med 1988;318:19-24
35. Krafchek J, Lin H-T, Beckman KJ, Nielsen AP, Magro SA,
Hargis J, Wyndham CRC: Cumulative effects of amiodarone
on inducibility of ventricular tachycardia: Implications for
electrophysiological testing. PACE 1988;11:434-444
36. Greenspon AJ, Volosin KJ, Greenberg RM, Jefferies L,
Rotmensch HH: Amiodarone therapy: Role of early and late
electrophysiologic studies. JAm Coll Cardiol 1988;11:17-123
37. The Cardiac Arrhythmia Suppression Trial Investigators: Preliminary report: Effect of encainide and flecainide on mortality
in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med 1989;321:406-410
KEY WORDS * amiodarone * quinidine * mexiletine
encainide * ventricular tachycardia
Downloaded from http://circ.ahajournals.org/ by guest on November 21, 2014
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Stretching - Anderson, Bob PDFDocument194 pagesStretching - Anderson, Bob PDFxehupatl100% (6)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Psychiatric Mental Health Nursing SuccessDocument407 pagesPsychiatric Mental Health Nursing Successwhatever1919191986% (49)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- 6 - ADKAR Reinforcement Ebook PDFDocument14 pages6 - ADKAR Reinforcement Ebook PDFHenrique NarcisoNo ratings yet
- Physical characteristics and vocal qualities of major neurological movement disordersDocument1 pagePhysical characteristics and vocal qualities of major neurological movement disordersShruti KumarNo ratings yet
- Molecular Properties Impact Oral Drug AbsorptionDocument21 pagesMolecular Properties Impact Oral Drug AbsorptionSava1988100% (1)
- (90-55-3000) BIOLIS 50i - Operator's M - V5.7 PDFDocument498 pages(90-55-3000) BIOLIS 50i - Operator's M - V5.7 PDFMatrix100% (1)
- Disobsession - FRANCISCO C. XAVIER, WALDO VIEIRADocument94 pagesDisobsession - FRANCISCO C. XAVIER, WALDO VIEIRASpiritism USA100% (3)
- PhEn602 Spring09 Notes1Document66 pagesPhEn602 Spring09 Notes1Abd Al-Rahmman Al-qatanani100% (1)
- 83Document7 pages83Sava1988No ratings yet
- NinhydrinDocument26 pagesNinhydrinSava1988No ratings yet
- RW A Review On 13 Thiazolidin 4 OnesDocument10 pagesRW A Review On 13 Thiazolidin 4 OnesSava1988No ratings yet
- Dissolution Testing (Kel 3)Document28 pagesDissolution Testing (Kel 3)Anonymous QEVAyPMNo ratings yet
- A Convenient and Efficeint Synthesis of Thiazolidin 4 Ones Via Ciclization of Substituted HidrazinecarbathioamidesDocument6 pagesA Convenient and Efficeint Synthesis of Thiazolidin 4 Ones Via Ciclization of Substituted HidrazinecarbathioamidesSava1988No ratings yet
- NinhydrinDocument26 pagesNinhydrinSava1988No ratings yet
- A Bate, A Măcina, A Strivi: Vt/viDocument5 pagesA Bate, A Măcina, A Strivi: Vt/viElisaveta VicleanuNo ratings yet
- IndometacinDocument47 pagesIndometacinSava1988No ratings yet
- Design, Synthesis and Evalutation of Novel Indomethacin Antioxidant CodrugsDocument10 pagesDesign, Synthesis and Evalutation of Novel Indomethacin Antioxidant CodrugsSava1988No ratings yet
- Chapter 01. Introduction To Biopharmaceutics and Its Role in Drug DevelopmentDocument25 pagesChapter 01. Introduction To Biopharmaceutics and Its Role in Drug DevelopmentSava19880% (1)
- Structure-Activity Relationship of Indomethacin Analogues ForDocument10 pagesStructure-Activity Relationship of Indomethacin Analogues ForSava1988No ratings yet
- Designing Safer NSAIDs: Synthesis of Indomethacin-Flavonoid ConjugatesDocument8 pagesDesigning Safer NSAIDs: Synthesis of Indomethacin-Flavonoid ConjugatesSava1988No ratings yet
- Evalutation of Glycolamide Esters of Indomethacin As Potentioal COX2Document14 pagesEvalutation of Glycolamide Esters of Indomethacin As Potentioal COX2Sava1988No ratings yet
- Conversion of Tryptophab To Indole 3 Acetic AcidDocument7 pagesConversion of Tryptophab To Indole 3 Acetic AcidSava1988No ratings yet
- Akt 1Document11 pagesAkt 1Sava1988No ratings yet
- Analysis of Recent Pharmaceutical Regulatory Documents On Analytical Method ValidationDocument16 pagesAnalysis of Recent Pharmaceutical Regulatory Documents On Analytical Method ValidationSava1988No ratings yet
- Sinteza IndometacinDocument18 pagesSinteza IndometacinSava1988No ratings yet
- 101 Full PDFDocument9 pages101 Full PDFSava1988No ratings yet
- Emodin Negatively Affects The Phosphoinositide 3-kinase/AKT Signalling Pathway: A Study On Its Mechanism of ActionDocument11 pagesEmodin Negatively Affects The Phosphoinositide 3-kinase/AKT Signalling Pathway: A Study On Its Mechanism of ActionSava1988No ratings yet
- Alfa TomatinaDocument11 pagesAlfa TomatinaSava1988No ratings yet
- Flavonoide Si Sist ImunDocument14 pagesFlavonoide Si Sist ImunSava1988No ratings yet
- Ejaculare PrecoceDocument6 pagesEjaculare PrecoceSava1988No ratings yet
- Pi 3 KDocument8 pagesPi 3 KSava1988No ratings yet
- Mechanism of Actions Ofcarbamazepine and DerivatesDocument10 pagesMechanism of Actions Ofcarbamazepine and DerivatesSava1988No ratings yet
- DesloratadinaDocument3 pagesDesloratadinaSava1988No ratings yet
- 101 Full PDFDocument9 pages101 Full PDFSava1988No ratings yet
- Oral Analgesics For Chronic Low Back PainDocument7 pagesOral Analgesics For Chronic Low Back PainSava1988No ratings yet
- 101 Full PDFDocument9 pages101 Full PDFSava1988No ratings yet
- MisoprostolDocument7 pagesMisoprostolSava1988No ratings yet
- BPH Syllabus PDFDocument126 pagesBPH Syllabus PDFDivya TiwariNo ratings yet
- contentPDFs 2023 T2DM Pharmacotherapy Chart V2-2Document2 pagescontentPDFs 2023 T2DM Pharmacotherapy Chart V2-2El MaheritoNo ratings yet
- Material Safety Data Sheet: Section 1 - Product InformationDocument2 pagesMaterial Safety Data Sheet: Section 1 - Product Informationmohamed AdelNo ratings yet
- Newcastle-Ottawa Quality Assessment Form For Cohort Studies: SelectionDocument2 pagesNewcastle-Ottawa Quality Assessment Form For Cohort Studies: SelectionKlinik KalitanjungNo ratings yet
- Digestive System Parts PacketDocument2 pagesDigestive System Parts PacketRusherNo ratings yet
- Effective Communication for InterpretersDocument5 pagesEffective Communication for InterpretersRaimundo SousaNo ratings yet
- The Dark Triada Personality A Review PDFDocument18 pagesThe Dark Triada Personality A Review PDFAvengingBrainNo ratings yet
- Hematology Sample QuestionsDocument5 pagesHematology Sample QuestionsEarleen Del Rosario100% (1)
- Marriage Equality, It's Just RightDocument1 pageMarriage Equality, It's Just RightAlphonse L. Williams IIINo ratings yet
- 2011 Fyi Report DocumentDocument110 pages2011 Fyi Report DocumentSmart Horizons Lifetime Training SolutionsNo ratings yet
- Comm 602 Assignment 1Document4 pagesComm 602 Assignment 1hamiltjw2No ratings yet
- Paediatric Dermatology: by EmilyDocument42 pagesPaediatric Dermatology: by EmilySilviuNo ratings yet
- Discussion of Dr. John Bowlby's PaperDocument11 pagesDiscussion of Dr. John Bowlby's PaperFrancisCevallosNo ratings yet
- Childhood Maltreatment Predicts Unfavorable Course of Illness andDocument11 pagesChildhood Maltreatment Predicts Unfavorable Course of Illness andxyncNo ratings yet
- Final Thesis With CV (For Bookbind)Document138 pagesFinal Thesis With CV (For Bookbind)Bea Marie Eclevia100% (1)
- SPECIAL WORKSHOP ANNOUNCEMENT-with Keshe NotesDocument4 pagesSPECIAL WORKSHOP ANNOUNCEMENT-with Keshe NotesAhmad AriesandyNo ratings yet
- Prevalence and Incidence of Rheumatoid Arthritis in Italy: Original ArticleDocument6 pagesPrevalence and Incidence of Rheumatoid Arthritis in Italy: Original ArticleDiego Francesco MacaliNo ratings yet
- Journal of Cleaner Production: Waqas Nawaz, Muammer KoçDocument20 pagesJournal of Cleaner Production: Waqas Nawaz, Muammer Koçthe unkownNo ratings yet
- Liver Disease: Overview of The LiverDocument6 pagesLiver Disease: Overview of The LiverMustafa AlmasoudiNo ratings yet
- Slums: The History of A Global Injustice, by Alan MayneDocument4 pagesSlums: The History of A Global Injustice, by Alan MayneKarliane MassariNo ratings yet
- Name: Jaanvi Mahajan Course: 2ballb Hons. REGISTRATION NO.: 22212033 Subject: Law and Medicine Submitted To: Mrs. Vijaishree Dubey PandeyDocument9 pagesName: Jaanvi Mahajan Course: 2ballb Hons. REGISTRATION NO.: 22212033 Subject: Law and Medicine Submitted To: Mrs. Vijaishree Dubey Pandeyjaanvi mahajanNo ratings yet
- Suicide ReportDocument4 pagesSuicide ReportAlikman HadjiamerNo ratings yet
- Practical Logbook: Medical Parasitology Department GIT Module 104Document16 pagesPractical Logbook: Medical Parasitology Department GIT Module 104Kareem DawoodNo ratings yet