Professional Documents
Culture Documents
Respiratory Gas Analysis Update 2008
Uploaded by
Jessica CCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Respiratory Gas Analysis Update 2008
Uploaded by
Jessica CCopyright:
Available Formats
Update in
Anaesthesia
Respiratory Gas Analysis
Grant McFadyen
Correspondence Email: Bruce.McCormick@rdeft.nhs.uk
OXYGEN CONCENTRATION ANALYSERS
It is important to measure the oxygen concentration
in the gas mixture delivered to a patient during
anaesthesia. There are three main techniques available
for measurement of the inspired oxygen concentration
(FiO2): galvanic, polarographic and paramagnetic
techniques. The paramagnetic method is currently the
most widely used in modern anaesthetic machines,
however galvanic fuel cells and the polarographic
electrode are found in older machines. These analysers
measure the oxygen partial pressure in a gas sample but
they display a percentage. Regular calibration of oxygen
analysers is vital.
Paramagnetic oxygen analysers
Oxygen possesses the property of paramagnetism, which
means that it is weakly attracted into a magnetic field.
This is because it has two electrons in unpaired orbits.
Most of the gases used in anaesthesia are repelled by a
magnetic field (diamagnetism).
The sample gas, taken from the breathing circuit, is
delivered to the analyser via a sampling tube, which
should be placed as close as possible to the patients
airway. Older paramagnetic analysers used a principle
described by Figure 1.
Newer analysers have two chambers separated by
a sensitive pressure transducer. The sample gas is
delivered to one chamber and room air is delivered
to the reference chamber. An electromagnet is rapidly
switched on and off creating a changing magnetic field
to which the sample gas is subjected. The magnetic
field causes the oxygen molecules to be attracted and
agitated. This results in changes in pressure on either
side of the pressure transducer. The pressure difference
across the transducer is proportional to the oxygen
partial pressure difference between the sample gas and
the reference gas (room air, containing 21% oxygen).
Paramagnetic oxygen analysers are very accurate
and highly sensitive. The analysers should function
continuously without any service breaks. They have
a rapid response allowing measurement of inspiratory
and expiratory oxygen on a breath-to-breath basis.
They are affected by water vapour and have a water
trap incorporated into their design.
Update in Anaesthesia | www.worldanaesthesia.org
Summary
Figure 1. A paramagnetic analyser. The sample gas fills
the sample chamber. Oxygen in the sample is attracted
into the magnetic field and tends to displace the nitrogen
filled dumbbell, which has no paramagnetic properties.
The greater the concentration of oxygen present, the
greater the displacement of the dumbbell. The degree
of rotation of the pair of dumbbells is recorded by the
amount a light beam is deflected, by a mirror mounted
on the dumbbell axis
The galvanic oxygen analyser (Fuel cell)
The galvanic analyser is placed on the inspiratory limb
of the breathing system (Figure 2). Oxygen molecules
diffuse across a membrane and an electrolyte solution,
to a gold (or silver) cathode, which is connected
through the electrolyte solution to a lead anode. An
electrical current is generated which is proportional to
the partial pressure of oxygen in the inspired gas. The
equation describing the reaction is:
Pb + 2OH-
Monitoring of respiratory
gases is considered by most
to be highly important
for the conduct of safe
anaesthesia. Monitoring
of inspired oxygen levels
ensures against delivery
of hypoxic gas mixtures to
the patient and is useful
for titration of oxygen flow
where oxygen supplies are
limited. Capnography tells
an anaesthetist a great deal
about the clinical status of
the patient, both in terms
of their respiratory and
cardiovascular systems. It
also lowers the threshold
for suspicion for rare but
potential fatal pathologies
such as malignant
hyperpyrexia. It many
settings agent monitoring
is not available, but its
value in detecting and
avoiding harmful overdose
of anaesthetic agents or
awareness due to insufficient
levels, mean that, ideally, it
should be incorporated into
all anaesthetists practice.
PbO + H2O + 2e-
The galvanic analyser has a response time of
approximately twenty seconds and is accurate to within
3%. Calibration is achieved using 100% oxygen and
room air (21% oxygen). Water vapour does not affect
its performance. It has the advantage that it is a battery
and therefore self-powering, however it is depleted by
continuous exposure to oxygen due to exhaustion of the
cell, so limiting its life span to about one year.
Grant McFadyen
Consultant Anaesthetist
Morriston Hospital
Swansea SA6 6NL
UK
page 170
It is useful to measure CO2 to assess the adequacy of ventilation, to
confirm tracheal intubation, to detect oesophageal intubation, to
indicate disconnection of the breathing system or ventilator, and to
diagnose circulatory problems and malignant hyperthermia.
Applications of capnography
Provided the patient has a stable cardiac status, stable body
temperature, absence of lung disease and a normal capnograph trace,
end-tidal carbon dioxide (ETCO2) can be estimated to be about
0.5-1.0kPa below the partial pressure of CO2 in arterial blood (PaCO2).
A normal PaCO2 is about 5.3kPa (40mmHg). Note that the conversion
factor between kPa and mmHg is 7.6.
Under the conditions described above, ETCO2 can be used to assess
the adequacy of ventilation - i.e. hypo-, normo-, or hyperventilation.
ETCO2 is not as reliable in patients who have respiratory failure. Any
increased ventilation/perfusion (V/Q) mismatch is associated with a
widened partial pressure (a-ET) gradient, and leads to ETCO2 values
that do not correlate with the true PaCO2.
Figure 2. The galvanic oxygen analyser (Fuel cell)
The polarographic oxygen analyser (Clark electrode)
The polarographic analyser has similar principles to the galvanic
analyser (Figure 3). Oxygen molecules diffuse across a teflon
membrane. Current flows between a silver cathode and a platinum
anode, which is proportional to the partial pressure of oxygen in the
inspiratory gas. It is battery powered, but its life expectancy is limited to
about three years because of deterioration of the teflon membrane.
The capnograph is the gold standard for detecting oesophageal
intubation. No or very little CO2 is detected if the oesophagus has
been intubated.
The capnograph is also useful in the following circumstances:
As a disconnection alarm for a ventilator or a breathing system.
There is sudden absence of the capnograph trace.
It may detect air embolism as a sudden decrease in ETCO2,
assuming that the arterial blood pressure remains stable.
To recognise sudden circulatory collapse as a sudden decrease in
ETCO2.
To diagnose malignant hyperthermia as a gradual increase in
ETCO2.
Techniques of measurement
Most analysers in theatre work using two principles:
Figure 3. The polarographic oxygen analyser (Clark electrode)
CAPNOGRAPHY
Capnometry is the measurement of carbon dioxide (CO 2) and
capnography is the display of the change in CO2 level with the
respiratory cycle. The capnograph displays a waveform of CO2 measured in kilopascals (kPa), millimetres of mercury (mmHg) or
percentage - and also displays the numerical value of the CO2 at the
end of exhalation, the end-tidal CO2, which is the closest value to
partial pressure of CO2 in the alveolus or arterial blood.
page 171
Infrared absorption spectroscopy
This is the most commonly used technique in anaesthesia. Gases of
molecules that contain at least two dissimilar atoms absorb infrared
radiation. Using this property, CO2 concentration can be measured
continuously throughout the respiratory cycle to give a capnograph
trace. CO2 absorbs infrared radiation particularly effectively at a
wavelength of 4.3micrometers. A photodetector measures radiation
reaching it from a light source at this wavelength. According to the
Beer-Lambert Law, the amount of infrared radiation absorbed in the
CO2 sample chamber is proportional to the number of CO2 molecules
(partial pressure of CO2) present in the chamber, and so the CO2
concentration can be calculated.
Photo-acoustic spectroscopy
The sample gas is irradiated with pulsatile infrared radiation, of
a suitable wavelength. Periodic expansion and contraction of the
gas produces a pressure fluctuation of audible frequency that can
be detected by a microphone. The advantages of photo-acoustic
spectrometry over conventional infrared absorption spectrometry
are:
Update in Anaesthesia | www.anaesthesiologists.org
The photo-acoustic technique is extremely stable and its calibration
remains constant over much longer periods of time.
The very fast rise and fall times give a much truer representation
of any change in CO2 concentration.
Other techniques for measuring CO2 include Raman scattering and
mass spectrometry.
of expiration, which results in a rapid increase in the CO2 reading. The
third phase, the expiratory plateau, occurs as the CO2 is exhaled from
all of the alveoli. The highest point of the plateau is taken to represent
the end-tidal CO2 (ETCO2). This marks the end of expiration. Phase
four is the onset of inspiration.
Raman scattering
When light passes through a gas sample it can undergo two types of
reflective process:
1. Rayleigh scattering where there is no change in the energy or
frequency of the light,
2. Raman scattering where the incident light loses energy to the
molecules of the gas and is reflected at lower frequency (less than
1 millionth of the time).
The magnitude of the light frequency shift is specific to the gas and
analysis of the reflected light allows identification of the gas. The
light used is intense, coherent and monochromatic (i.e. from a laser).
The machines are rapid, with breath to breath analysis, but tend to be
bulky and heavy. They are more versatile than infra-red analysis and
more reliable than mass spectometry.
Site of sampling within the breathing system
Gas from the breathing system can be sampled either by a sidestream
or a mainstream analyser.
Sidestream sampling
Gas is drawn from the breathing system by a 1.2mm internal diameter
tube. The tube is connected to a lightweight adapter near the patients
end of the breathing system. It delivers the gas to the sample chamber.
It is made of Teflon so it is impermeable to CO2 and does not react
with anaesthetic agents. Only the precise tubing recommended by the
manufacturer should be used and only of the recommended length.
Typical infrared instruments sample at a flow rate between 50 and
150ml.min-1. When low fresh gas flows are used the sampled gas may
be returned to the breathing circuit. It is important that the tip of
the sampling tube should always be as near as possible to the patients
trachea, but the sampled gas mixture must not be contaminated by
inspired gas during the expiratory phase.
Mainstream sampling
The sample chamber is positioned within the gas stream near the
patients end of the breathing system. Although heavier and more
cumbersome, it does have advantages over sidestream sampling:
The delay between the rise and fall times of gas composition
changes and display on the capnograph is less, as gas does not need
to be transported to the monitor.
No gas is drawn from the breathing system.
The mixing of gas that occurs along the sample tube with
sidestream sampling is avoided.
There are fewer problems with water vapour condensation.
The capnograph trace (Figure 4)
The first phase occurs during inspiration. The second phase is the onset
Update in Anaesthesia | www.worldanaesthesia.org
Figure 4. A typical capnography trace; 1 inspiratory baseline; 2
expiratory upstroke; 3 expiratory plateau; 4 inspiratory downstroke
Abnormal capnography traces
Rebreathing (Figure 5)
A waveform that does not return to the baseline during inspiration
indicates rebreathing of exhaled CO2-containing gas. Possible causes
are:
The fresh gas flow is too low in non-rebreathing system (e.g.
Mapelson type A, D or E).
The soda lime in a circle system is depleted.
Figure 5. Rebreathing is indicated by failure of the trace to return to the
baseline during inspiration (arrow)
Sloping plateau (Figure 6)
This appearance is seen in patients with obstructive airways disease
(asthma and chronic obstructive pulmonary disease). In patients
with obstructive airways disease, the lungs are perfused with blood as
normal, but the alveoli are unevenly ventilated. CO2 is transferred from
the alveoli to the larger airways during expiration, but this takes longer
in lung units that have narrower bronchi. These slower emptying lung
units have a higher CO2 concentration and so the CO2 concentration
in mixed expired gas gradually rises throughout expiration, as these
slow emptying units contribute a greater proportion of the expired
gas mixture.
page 172
they cause to move in the airways is a greater proportion of the overall
lung volume when the patient is at functional residual capacity.
The curare cleft (Figure 8)
This appearance indicates reversal of neuromuscular blockade in a
ventilated patient. When a paralysed patient starts taking small breaths
as the neuromuscular blocking agent reverses, clefts are seen on the
capnograph trace.
Figure 6. The sloping plateau (arrowed)is typical of lower airways
obstruction (asthma and COPD)
Cardiac oscillations
Cardiac impulses are transmitted through the mediastinum to the
large airways and are detected by the capnograph. These oscillations
are most obvious in apnoeic patients, since the volume of gas that
Figure 8. Breathing against the ventilator.
FURTHER READING
Figure 7. Cardiac oscillations.
page 173
Williamson JA, Webb RK, Cockings J, Morgan C. The Australia incident
monitoring study. The capnograph: applications and limitations - an
analysis of 2000 incident reports. Anaesthesia and Analgesia 1993; 21:
551-7
Schmitz BD, Shapiro BA. Capnography. Respiratory Care Clinics of
North America. 1995; 1: 107-17
Al-Shaikh B, Essentials of Anaesthetic Equipment. Churchill Livingstone
1995.
Update in Anaesthesia | www.anaesthesiologists.org
You might also like
- Unilat SABDocument8 pagesUnilat SABJessica CNo ratings yet
- Adductor Canal Block For Total Knee ArthroplastyDocument3 pagesAdductor Canal Block For Total Knee ArthroplastyJessica CNo ratings yet
- Adductor Canal Block Versus Femoral Nerve Block For Total Knee ArthroplastyDocument11 pagesAdductor Canal Block Versus Femoral Nerve Block For Total Knee ArthroplastyJessica CNo ratings yet
- Multimodal Pain Management TechniquesDocument10 pagesMultimodal Pain Management TechniquesJessica CNo ratings yet
- Multimodal Pain Management TechniquesDocument10 pagesMultimodal Pain Management TechniquesJessica CNo ratings yet
- Adductor Canal Block For Total Knee ArthroplastyDocument3 pagesAdductor Canal Block For Total Knee ArthroplastyJessica CNo ratings yet
- (PAUTHORS), Journal of Emergencies, Trauma, and Shock (JETS)Document4 pages(PAUTHORS), Journal of Emergencies, Trauma, and Shock (JETS)Jessica CNo ratings yet
- Shout For Help/Activate Emergency Response: CPR StartDocument2 pagesShout For Help/Activate Emergency Response: CPR StartdavpierNo ratings yet
- Crochet Baby Booties Free PatternDocument8 pagesCrochet Baby Booties Free PatternJessica CNo ratings yet
- Renal Approach To Acid Base BalanceDocument12 pagesRenal Approach To Acid Base BalanceJessica CNo ratings yet
- Maintenance Intravenous Fluids in Acutely Ill PatientsDocument11 pagesMaintenance Intravenous Fluids in Acutely Ill PatientsKevin Mora BañosNo ratings yet
- Dural Tissue Trauma and Cerebrospinal Fluid Leak AfterDocument7 pagesDural Tissue Trauma and Cerebrospinal Fluid Leak AfterJessica CNo ratings yet
- Pooja Journal - pdf3 PDFDocument15 pagesPooja Journal - pdf3 PDFJessica CNo ratings yet
- Renal Approach To Acid Base BalanceDocument12 pagesRenal Approach To Acid Base BalanceJessica CNo ratings yet
- Pooja Journal - pdf2Document14 pagesPooja Journal - pdf2Jessica CNo ratings yet
- Medical ThesiasDocument360 pagesMedical ThesiasJessica CNo ratings yet
- Anesthesia and The Hepatobiliary SystemDocument35 pagesAnesthesia and The Hepatobiliary Systemakosijoshua100% (1)
- Normal Physiology of AgingDocument19 pagesNormal Physiology of AgingJessica CNo ratings yet
- NationalOverseasScholarshipFresh&Renewal2013 14Document6 pagesNationalOverseasScholarshipFresh&Renewal2013 14Jessica CNo ratings yet
- Capnography D. Gihan TarabihDocument46 pagesCapnography D. Gihan TarabihJessica CNo ratings yet
- Application Form For Fee RefundDocument2 pagesApplication Form For Fee RefundJessica CNo ratings yet
- Femoral Nerve Block - Landmark ApproachDocument12 pagesFemoral Nerve Block - Landmark ApproachJessica CNo ratings yet
- Regional Anesthesia for Hand Surgery: Bier Block LectureDocument28 pagesRegional Anesthesia for Hand Surgery: Bier Block LectureJessica CNo ratings yet
- Guidelines Coagulopathy and Regional AnaesthesiaDocument14 pagesGuidelines Coagulopathy and Regional AnaesthesiaJessica CNo ratings yet
- Vein Skin Vein Skin Guidewire Catheter AccessDocument1 pageVein Skin Vein Skin Guidewire Catheter AccessJessica CNo ratings yet
- General Anesthesia Cart ChecklistDocument1 pageGeneral Anesthesia Cart ChecklistyeepersNo ratings yet
- RegionalDocument40 pagesRegionalJessica CNo ratings yet
- Femoral Nerve Block - Landmark ApproachDocument12 pagesFemoral Nerve Block - Landmark ApproachJessica CNo ratings yet
- Interpleural Block - Part 1: ReviewarticleDocument11 pagesInterpleural Block - Part 1: ReviewarticleAlfredo Salinas CastilloNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Quality Control & Evaluation of Pharmaceutical Aerosols: Prepared By: Mahesh W. ThubeDocument20 pagesQuality Control & Evaluation of Pharmaceutical Aerosols: Prepared By: Mahesh W. ThubeDrSrujan Kumar ReddyNo ratings yet
- Forces Grade 2Document7 pagesForces Grade 2Ngọc Xuân BùiNo ratings yet
- Shell Corena S2 R 46-Locom Sarbesti PDFDocument3 pagesShell Corena S2 R 46-Locom Sarbesti PDFCorina StanculescuNo ratings yet
- Singly Reinforced BeamDocument3 pagesSingly Reinforced BeamriverieNo ratings yet
- OwennDocument7 pagesOwennOwenNo ratings yet
- MarineDocument10 pagesMarinewaseemNo ratings yet
- Experiment No: 1: Slotted Link Mechanism ExperimentDocument4 pagesExperiment No: 1: Slotted Link Mechanism ExperimentSamina TariqNo ratings yet
- Organic Resistive Switching Device Based On Cellulose Gelatine Microcomposite FibersDocument9 pagesOrganic Resistive Switching Device Based On Cellulose Gelatine Microcomposite FibersShuvam PawarNo ratings yet
- Atlas of Fatigue CurvesDocument534 pagesAtlas of Fatigue CurvesCristiana Costa100% (1)
- Reversible Kinetics and Thermodynamics of The Homopolymerization of - Lactide With 2-Ethylhexanoic Acid Tin (II) SaltDocument11 pagesReversible Kinetics and Thermodynamics of The Homopolymerization of - Lactide With 2-Ethylhexanoic Acid Tin (II) SaltMathilda PasaribuNo ratings yet
- Colloidal Silver Vs Silver Sol: What's The DifferenceDocument4 pagesColloidal Silver Vs Silver Sol: What's The DifferenceALKESWWNo ratings yet
- Protocol: Adult - Abdomen - ABD. SUP. RM1: Page 1 of 20Document20 pagesProtocol: Adult - Abdomen - ABD. SUP. RM1: Page 1 of 20Fábio Ricardo BarretoNo ratings yet
- Shear Wall ModellingDocument42 pagesShear Wall ModellingGopalAdhikariNo ratings yet
- Generation of Electricity Using Nitinol: S K Haaris G Madhu Murali Siran2Document3 pagesGeneration of Electricity Using Nitinol: S K Haaris G Madhu Murali Siran2Deepak BhopeNo ratings yet
- Physics Lab 1 - Triboelectric SeriesDocument5 pagesPhysics Lab 1 - Triboelectric SeriesshamNo ratings yet
- Assignment 2 - FramesDocument12 pagesAssignment 2 - FramesZazliana Izatti100% (1)
- 2017elisionaltechwe4t NiqueofplottingcampbelldiagramsDocument9 pages2017elisionaltechwe4t NiqueofplottingcampbelldiagramsSmileNo ratings yet
- Future of Nitinol TiresDocument5 pagesFuture of Nitinol TiresAmir Hossein ShahdadiNo ratings yet
- 2.1 Liquid Pressure 2021Document13 pages2.1 Liquid Pressure 2021GOH YIN XUEN MoeNo ratings yet
- WS1 - Phase Diag-Heating-Cooling CurveDocument2 pagesWS1 - Phase Diag-Heating-Cooling CurveNorman Jr. JazulNo ratings yet
- Basics Particle PhysicsDocument70 pagesBasics Particle PhysicsSurjit MukherjeeNo ratings yet
- Wang 2022 J. Electrochem. Soc. 169 031504Document9 pagesWang 2022 J. Electrochem. Soc. 169 031504laguna028No ratings yet
- Precipitacion Manabi RRDocument34 pagesPrecipitacion Manabi RRIkiki MejiaNo ratings yet
- Pipe Flow Software: Submerged Coils - Heat Transfer CoefficientsDocument6 pagesPipe Flow Software: Submerged Coils - Heat Transfer CoefficientspaldopalNo ratings yet
- 21 SOP For Vacuum PumpDocument6 pages21 SOP For Vacuum PumpAmit Biswas100% (1)
- Chapter 7 Ship VibrationDocument3 pagesChapter 7 Ship VibrationTara MurrayNo ratings yet
- Sintering Behavior of Nanocrystalline 8 mol% Yttria-Stabilized ZirconiaDocument6 pagesSintering Behavior of Nanocrystalline 8 mol% Yttria-Stabilized ZirconiaamirpouyanNo ratings yet
- Egatube ConduitDocument2 pagesEgatube ConduitAyu SitaNo ratings yet
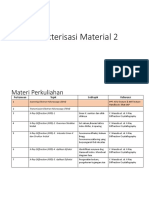
- Karakterisasi Material 2Document52 pagesKarakterisasi Material 2George Amos BastianNo ratings yet
- ASME 331.4 piping standardsDocument1 pageASME 331.4 piping standardsJoelHernandezGonzalezNo ratings yet