Professional Documents
Culture Documents
Sealing Performance of Resin Cements Before Andafter Thermal Cycling: Evaluation by Optical Coherence Tomography
Uploaded by
Neelima SonawaneOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sealing Performance of Resin Cements Before Andafter Thermal Cycling: Evaluation by Optical Coherence Tomography
Uploaded by
Neelima SonawaneCopyright:
Available Formats
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
Available online at www.sciencedirect.com
ScienceDirect
journal homepage: www.intl.elsevierhealth.com/journals/dema
Sealing performance of resin cements before and
after thermal cycling: Evaluation by optical
coherence tomography
Alaa Turkistani a,b,c , Alireza Sadr c, , Yasushi Shimada b , Toru Nikaido b ,
Yasunori Sumi d , Junji Tagami b,c
a
Operative Dentistry Division, Conservative Dental Sciences Department, Faculty of Dentistry,
King Abdulaziz University, Jeddah, Saudi Arabia
b Cariology and Operative Dentistry, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental
University, 1-5-45, Yushima, Bunkyo-ku, Tokyo 113-8549, Japan
c Global COE, International Research Center for Molecular Science in Tooth and Bone Diseases, Tokyo Medical and
Dental University, 1-5-45, Yushima, Bunkyo-ku, Tokyo 113-8549, Japan
d Division of Oral and Dental Surgery, Department of Advanced Medicine, National Center for Geriatrics and
Gerontology, National Hospital for Geriatric Medicine, 36-3, Gengo, Morioka, Obu, Aichi 474-8511, Japan
a r t i c l e
i n f o
a b s t r a c t
Article history:
Objectives. Self-adhesive resin cements have been recently introduced; however, there is
Received 25 December 2012
little data available on their long-term performance. In this in vitro study, swept-source
Received in revised form
optical coherence tomography (OCT) at 1310 nm center wavelength was used for monitoring
4 August 2013
adaptation of indirect resin restorations after thermal cycling.
Accepted 21 May 2014
Methods. Resin inlays were luted to class-I cavities of extracted human teeth using three
resin cements; Clearl SA Luting (SA; Kuraray), Bistite II DC or Multibond II (Tokuyama Dental). Each cement was applied with or without pre-coating of dentin by a self-etch adhesive
Keywords:
(Clearl SE Bond) and a low-viscosity microlled resin. OCT imaging was performed after
Resin inlay
24 h, after 2000 and after 10,000 thermocycles (n = 5). Selected samples were sectioned for
Resin cement
interfacial observation by confocal laser scanning microscope (CLSM). Floor adaptation (per-
Resin coating
centage) was analyzed by software on 20 B-scans throughout each specimen, and subjected
Adaptation
to statistical analysis by three-way ANOVA test at a signicance level of 0.05.
Optical coherence tomography
Results. Resin cement type, resin coating and thermal aging all signicantly affected
adaptation (p < 0.05). Initially, SA showed the highest adaptation; however, thermal aging signicantly affected its sealing. The best results for all the cements were consistently achieved
when the resin coating technique was applied where no deterioration of interfacial integrity
was observed in the coated groups. CLSM closely conrmed OCT ndings in all groups.
Signicance. OCT could be used for monitoring of composite inlays with several interfacial resin layers. The application of a direct bonding agent in the resin-coating technique
improved interfacial sealing and durability of all resin cements.
2014 Academy of Dental Materials. Published by Elsevier Ltd. All rights reserved.
Corresponding author. Tel.: +81 3 5803 2483; fax: +81 3 5803 0195.
E-mail address: alireza.ope@tmd.ac.jp (A. Sadr).
http://dx.doi.org/10.1016/j.dental.2014.05.010
0109-5641/ 2014 Academy of Dental Materials. Published by Elsevier Ltd. All rights reserved.
994
1.
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
Introduction
The aesthetic aspect of dental treatment has become increasingly popular in the recent years, especially with the
development of improved materials and adhesive techniques
using composite resins. The indirect composite resin restoration technique involves extra-oral fabrication of an inlay and
its placement with a resin cement. It has been reported that for
large cavities, indirect restorations bear advantages over direct
techniques such as improvements in anatomic form, contour, fracture resistance and wear resistance [1]. Furthermore,
extra-oral fabrication aids in the relief of residual stresses and
ensures that the negative effects of polymerization shrinkage
are conned to the thin layer of resin cement [2].
On the other hand, it is believed that the viscous resin
cements may not provide dentin bonding comparable to
dentin-bonding system (DBS) used for direct composite [35].
This may affect the sealing ability of these cements and lead
to lower penetration to tooth substrate and hence, lower bonding performances in comparison to DBS. Therefore, a resin
coating technique for indirect restorations was introduced in
which DBS and a low viscosity microlled resin are applied
to seal dentin surface after preparation, decreasing pulp
irritation and postoperative sensitivity and improving bond
strength [69]. Meanwhile, the effectiveness of this technique
for the newly introduced resin cement products (such as
self-adhesive resin cements) has not been investigated. The
self-adhesive resin cement is proposed to simplify the cementation procedure; it bonds to dentin in one step without the
need of conditioning or pre-treatment (priming) of the surface
[10,11].
Adhesion tests have been routinely used for laboratory
evaluation of these biomaterials. However, the success of
a restoration also greatly depends on its sealing ability of
the dental tissue in an actual cavity [12]. Different methods
are conventionally used to evaluate the marginal integrity
and sealing of restorations. The most common method is
detecting dye penetration depth under a stereoscopic microscope and/or scanning electron microscope (SEM). However,
these methods are considered as destructive methods since
they require sample sectioning, and may be subjective. More
recently, three-dimensional and in-depth imaging methods
have been introduced and utilized for characterization of
dental composites [1318]. Optical coherence tomography
(OCT) can provide noninvasive, high resolution cross-sectional
images for biologic microstructures and materials based on
light backscattering from within the structure. Dental composites and hard tissues are scattering media and therefore
can be suitable substrates for OCT imaging [1624]. Toothrestoration interface under direct resin restorations has been
investigated using this technique [18,19,21,25]; however, there
are few reports on evaluation of indirect restorations.
Thermal cycling procedure has been accepted as an effective means of articially aging composite restorations to study
their interfacial characteristics in the long-term. In this regard,
imaging of resin restorations by OCT before and after thermal
aging appears to be an attractive research method. Therefore,
the aim of this laboratory study was to evaluate the effect of
thermal cycling and resin coating technique on the adaptation
of indirect composite inlays luted with resin cements under
OCT, and conrmation of OCT ndings by cross-sectional confocal laser scanning microscopy (CLSM). The null hypotheses
tested were as follows: (1) there was no difference in the interfacial sealing of the composites inlays between different resin
cements; (2) the resin coating could not improve the interfacial integrity; and (3) There were no changes in the interfacial
integrity of different test groups after thermal aging.
2.
Materials and method
2.1.
Specimen preparation
For this study, thirty extracted human third molars, free
of cracks, caries and restorations were selected after the
patients informed consent, as approved by the Institutional
Review Board of Tokyo Medical and Dental University, Human
Research Ethics Committee, protocol no. 725. The root structure was removed below the cement-enamel junction and in
order to expose a at dentin substrate; the occlusal thirds were
removed by trimming the crowns at right angles to the long
axis of the teeth using a model trimmer (Y-230; Yoshida, Tokyo,
Japan). Round class I cavities were prepared on the at occlusal
surfaces by using a cylindrical diamond bur attached to a highspeed air turbine under water coolant (carborundum points,
50 m grain size, SHOFU, Kyoto, Japan). Finishing diamond
burs were used afterward to have a ne surface nish (SF114,
SHOFU, Kyoto, Japan). To maintain cutting efcacy, the bur
was replaced every ve preparations. The cavity was approximately 4 mm in width and 2 mm in depth. The teeth were
then randomly divided into two groups of fteen teeth each
according to the surface treatment. For the rst group (control
group), dentin surface was kept untreated. In the second group
(resin-coated group), the cavity surface was prepared using the
self-etching bonding system, Clearl SE Bond (Kuraray Noritake Dental, Tokyo, Japan) and a low viscosity microlled resin
(Clearl Protect Liner F, Kuraray Noritake Dental, Tokyo, Japan).
According to the manufacturers instructions, SE primer was
applied rst to the cavity for 20 s and gently air dried. Then,
SE bond was applied; mildly air dried and light cured for 20 s
using a conventional halogen light curing unit (Optilux 501,
Kerr, CA, USA; 550 mW/cm2 ). After that, Protect Liner F was
placed on the already cured adhesive surface with a brush and
light cured for 20 s.
The cavities in both groups were then lined (covered) with a
separating lm (Pechiney Plastic Packaging, Chicago, IL, USA),
lled with one increment of composite (Clearl Majesty Posterior, Kuraray Noritake Dental, Tokyo, Japan), and light cured
for 40 s using the light curing unit. After curing, the composite
inlays were carefully removed from the cavities and checked
for t. The resin inlays were monitored under OCT prior to
cementation and the defective ones were excluded and refabricated.
The prepared cavity surfaces in group 1 and the coated surfaces in group 2 were both temporized with a water-setting
non-eugenol temporary lling material (Caviton EX, GC, Japan)
and stored in an incubator at 37 C in a humid condition to
simulate the clinical situation for indirect composite restorations. After 24 h, the temporary lling material was carefully
995
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
removed with a spoon excavator and surface was wiped with
a cotton pellet containing ethanol for 10 s. The coated surfaces were then cleaned for 10 s using 37% phosphoric acid
gel, rinsed and dried in order to remove any debris.
The tting surfaces of the resin inlays were treated with
37% phosphoric acid gel for 15 s, rinsed with water and gently
air dried. Then, Tokuso Ceramic Primer (Tokuyama Dental)
was applied as a silane coupling agent to the surface and
air-dried.
Specimens from each group were further divided into three
subgroups according to the type of luting resin cement used.
Table 1 lists the materials used in this study while Fig. 1 shows
schematic drawing for the sample preparation.
The resin cements used in this study were the dual-cure
with self-etching primer Bistite II DC (Tokuyama Dental),
the self-adhesive Clearl SA Luting cement (Kuraray Noritake Dental, Tokyo, Japan) and the MMA-based self-etching
chemically-cured Multibond II (Tokuyama Dental). Each of the
three cements was applied according to the manufacturers
instructions.
2.2.
Thermocycling procedure
All specimens were then stored at 37 C in humid condition
for 24 h prior to the initial OCT imaging. Then, all the specimens were thermocycled for 10,000 cycles, which was roughly
estimated to represent one year of clinical function approximately [26]. They were fatigued between 5 C and 55 C with a
dwell time of 30 s in each temperature, and a transfer time of
2 s between baths (Cool Line CL200 and Cool Mate TE200, Yamato Scientic Co., Tokyo, Japan). The specimens were subjected
to OCT evaluation to detect any changes in the adaptation of
the resin restorations after 2000 cycles and after completing
10,000 cycles.
2.3.
OCT system
A swept-source OCT system (Santec OCT-2000, Santec Co.,
Komaki, Japan), was used in this study. The spectral bandwidth
of the optical source is over 100 nm centered at 1310 nm at a
20 kHz sweep rate. The probe power is within the safety limits
dened by American National Standard Institute. The sensitivity of this system and the shot-noise limited sensitivity are
106 and 119 dB, respectively. The axial resolution of the system
is 11 m in air, which corresponds to 7 m in tissue assuming
a refractive index of approximately 1.5. The lateral resolution
depends on the objective lens at the probe and was 17 m in
this study. Backscattered light carrying information about the
microstructure of the sample is collected, returned to the system, digitized in time scale and then analyzed in the Fourier
domain to reveal the depth information of the subject. The
system analyzes the frequency components of backscattered
light from the sample and creates real-time high resolution
2-D image.
2.4.
holes were drilled on the specimen surface to make sure that
specimens were placed at the same orientation as accurately
as possible.
In order to capture OCT image, the specimen was positioned on a metal stage with a 35 tilt to avoid peculiar
surface reections. The surface of the specimen was blot dried
using air duster to standardize the tooth surface hydration
condition [22]. Then, the focus light beam was projected onto
the tooth surface at 90 and scanned across the cavity in three
dimensions using OCT probe. In this manner, 20 serial 2D sections at 200 m interval were obtained. The size of each image
was 2000 1019 pixels corresponding to 5 mm 6.6 mm (x, z).
For the data analysis purpose, each of the 20 serial 2D sections
was digitally analyzed using ImageJ (ver. 1.42q, National Institutes of Health, Bethesda, MD, USA). A custom computer code
was developed as a plugin for ImageJ based on a binarization
process previously reported [13,21], to facilitate image analysis
procedure and distinguish pixel clusters with higher brightness indicating gap or unsealed interface at the cavity oor.
The total cavity adaptation (including resin cement and/or
coating interface) was calculated as
OCT imaging and analysis
Specimens were subjected to serial 2D scans 24 h after cementation, and after 2000 and 10,000 thermal cycles. To ensure the
repeatability of the OCT scans for the same specimen, small
Cavity adaptation%
2.5.
gap length at all cross-sections
cavity oor length at all cross-sections
100
Confocal laser scanning microscopy (CLSM)
To conrm the presence or absence of gap at tooth-restoration
interface, randomly selected specimens after thermal cycling
were sectioned with low-speed diamond saw (Isomet, Buehler,
Lake Bluff, IL, USA) and then polished using polishing machine
(ML-160 A, Maruto, Tokyo, Japan) with silicone carbide (SiC)
paper (Sankyo, Saitama, Japan) and diamond pastes with particle size down to 0.25 m. The same interfacial location in
a certain OCT cross-sectional slice was observed under CLSM
(1LM21H/W, Lasertec Co., Yokohama, Japan) with a He-Ne laser
source (632.8 nm) and 0.1 mW maximum output power at magnication levels of 5001250.
2.6.
Statistical analysis
For the statistical analysis of the adaptation, the data were
statistically analyzed with three-way ANOVA followed by multiple comparisons using t-tests with Bonferroni corrections as
post-hoc. The factors were resin cement type, resin coating
and thermal cycling. All the statistical procedures were performed at signicance level of = 0.05 with using Statistics
package (ver. 16 for windows; SPSS, Chicago, IL, USA).
3.
Results
Representative OCT images from each group after thermal
aging and their conrmatory CLSM images with A-scan
(SS-OCT signal intensity) proles plotted against selected
areas in the same cross-sections are shown in Figs. 24 for
BT, SA and MB respectively. There was a considerable loss of
996
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
Table 1 Materials used in this study.
Material
(Abbreviation)
Manufacturer
Lot no.
Dentin bonding system
Clearl SE Bond
(SE)
Kuraray Noritake Dental
011595
Low-viscosity microlled resin
Protect Liner F
(PLF)
Kuraray Noritake Dental
0074DA
Resin cements
Bistite II DC
(BT)
Tokuyama Dental
028012
Clearl SA Luting
(SA)
Kuraray Noritake Dental
0141AA
Multibond II
(MB)
Tokuyama Dental
0780Z1
Indirect resin composite
Clearl Majesty Posterior
(MP)
Kuraray Noritake Dental
00111A
Procedure
Composition
Primer: MDP, HEMA, hydrophilic dimethacrylate,
dl-camphorquinone, N,N-diethanol-p-toluidine,
water.
Bond: MDP, Bis-GMA, HEMA, hydrophobic
dimethacrylate, dl-camphorquinone,
N,N-diethanol-p-toluidine, silanated colloidal
silica.
Apply the primer for 20 s.
Mild air blow.
Apply adhesive and air blow gently.
Light cure for 10 s.
Bis-GMA, TEGDMA, uoride-methyl
methacrylate, camphorquinone, silanized
colloidal silica, pre-polymerized organic ller.
Apply in a thin layer, light cure for 20 s.
Primer 1 (A and B): phosphoric acid monomer,
acetone, alcohol, water, initiator.
Primer 2: HEMA, acetone, initiator.
Resin cement pastes:
Paste-A: NPGDMA, Bis-MPEPP, silica-zirconia
ller.
Paste-B: MAC-10, silica-zirconia ller,
benzoylperoxide, photo-initiator.
Paste A: Bis-GMA, TEGDEMA, MDP, hydrophobic
aromatic dimethacrylate, silanated barium glass
ller, silanated colloidal silica,
dl-camphorquinone, benzoyl peroxide, initiator.
Paste B: Bis-GMA, hydrophobic aromatic
dimethacrylate, hydrophobic aliphatic
dimethacrylate, silanated barium glass ller,
silanated colloidal silica, surface treated sodium
uoride, accelerators, pigments.
Primer: phosphoric acid monomer, water,
acetone, UDMA, co-activator.
liquid: MMA, UDMA, HEMA, MTU-6, borate
catalyst.
powder: PMMA, co-activator.
Apply primer 1A + 1B, leave for 30 s, air dry, apply
primer 2, leave for 20 s, air-dry, place mixed
paste A + B, light cure for 20 s.
Silanated glass ceramics, silanted silica ller,
surface treated alumina microller, Bis-GMA,
TEGDMA, hydrophobic aromatic dimethacrylate,
dl-camphorquinone.
Apply the cement paste mix to the restoration,
place the restoration.
Light cure for 25 s, and then remove the excess
cement.
Light cure for 20 s.
Apply primer for 20 s and gently air dry for 10 s.
Powder: liquid: 1:3
Mix for 5 s, apply to dentin surface.
Bulk lling and light cure for 40 s.
Abbreviations: MDP: 10-methacryloyloxydecyl dihydrogen phosphate, HEMA: 2-hydroxyethyl methacrylate, Bis-GMA: bisphenol-A diglycidyl
ether dimethacrylate, TEGDMA: triethyleneglycol dimethacrylate, MAC-10: methacryloyloxundecane dicarboxylic acid, MMA: methyl methacrylate, PMMA: poly methyl methacrylate, UDMA: urethane dimethacrylate, MTU-6: 6-methacryloxyhexyl 2-thiouracil-5-carboxylate.
signal intensity through the composite inlay as clearly seen
in the A-scan proles in Figs. 2e and f, 3e and f and 4e and f,
which were drawn by averaging the OCT signal intensity over
an area of 150 m. Despite this attenuation, the peak caused
by interfacial gaps was easily detectable in Figs. 2e, 3e and 4e;
while in other areas (with no gap), no such peak was seen
(Figs. 2f, 3f and 4e and f). A bright area in the OCT image
indicates gap due to the presence of optical variation between
restorative material, air in the gap and tooth structure leading
to light reection [16]; areas with increased brightness on
OCT images were conrmed as gap by CLSM examination in
Figs. 2c, 3c and 4c. Resin coating resulted in a layer approximately 100 m in thickness and improved adaptation as
conrmed by the CLSM images in Figs. 2d, 3d and 4d. After
thermal cycling, most of the non-coated specimens showed
high backscattering from the resin-dentin interface regardless
of the type of cement as shown in Figs. 2a, 3a and 4a. In some
specimens, the bright area extended throughout the cavity
bottom indicating complete loss of seal (Fig. 3a); while in
others, the gap was formed only at a part of the specimen
(Fig. 4a). On the other hand, most of the specimens in the
resin-coated groups showed little or no detectable reection
from the interface (Figs. 2b, 3b and 4b).
The mean adaptation percentage of the three different
resin cements to dentin with or without resin coating and
standard deviation for each group are listed in Table 2 and
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
997
Fig. 1 Schematic view of study method; resin inlays were cemented in round cavities using a resin cement with or without
resin coating, and subjected to OCT observation at baseline and after thermal cycling. CLSM was used for conrmation of
OCT ndings after cutting the specimens. SE: dentin-bonding system Clearl SE Bond; PLF: Protect liner F; BT: Bistite II DC;
BT-NC: Non-Coated Bistite II DC; BT-C: Coated Bistite II DC; SA: Clearl SA Luting; SA-NC: Non-Coated SA Luting; SA-C:
Coated SA Luting; MB; Multibond II; MB-NC: Non-Coated Multi bond II; MB-C: Coated Multibond II.
presented as bar graphs in Fig. 5. ANOVA test demonstrated
a signicant effect of resin coating, cement type and thermal
cycling on gap formation in the cavity oor (p < 0.05). The
interaction between these three factors was also signicant
(p < 0.05). The application of resin coating of SE and PLF
signicantly improved the adaptation of resin inlays to
dentin (p < 0.05) regardless the type of cement or sample
age. Without resin coating, SA signicantly showed better
Fig. 2 Representative cross-sectional OCT images and signal intensity proles of BT-NC and BT-C groups after 10,000
thermal cycles and corresponding CLSM images of the same cross-sections. (a) B-scan and binary image of the interface of a
resin inlay cemented with BT showing an increase in the signal intensity at the cavity oor. (b) B-scan and its binarization
from BT-C group showing an improved adaptation of the resin inlay after resin coating. (c and d) CLSM images from the
same sections at 500 and 1250 magnication conrming the OCT ndings. The gap under BT-NC specimen in (c) appears
to have occurred at the resin cement primer and dentin interface (blank arrow). (e and f) A-scans (SS-OCT signal intensity)
plotted over selected areas (indicated by lines) in the same cross-sections. Note the peak in backscatter signal (arrow) in (e)
caused by Fresnel reection due to contrast in refractive index between restorative material and air at the interfacial gap
while in (f), no detectable change in signal intensity can be observed when the interface is sealed. In: resin inlay; Ce: resin
cement; RC: resin coat; D: dentin.
998
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
Fig. 3 Images obtained from specimens luted using SA with and without resin coating after 10,000 thermal cycles. (a)
B-scan and binary image of the selected interface from a SA-NC sample showing an increase in the signal intensity at the
cavity oor. (b) No gap was detected in B-scan and binary image of this SA-C specimen. (c) CLSM images from the same
section as in (a) at 500 and 1250 magnication showing gap between SA and dentin in the cavity oor. (d) Conrmatory
CLSM image of the same section presented in (b). (e and f) A-scans plotted along the designated lines shown in (a and b).
Arrow in (e) indicates the high intensity in backscatter signal caused by air lled gap in the interface. In: resin inlay; Ce:
resin cement; RC: resin coat; D: dentin.
sealing compared to BT and MB. However, there was no
signicant difference in the adaptation between BT and
MB (p > 0.05). In the non-coated specimens, thermal cycling
regimens caused signicant decrease (p < 0.05) in the cavity
adaptation percentage of BT and SA only after 2000 cycles.
However, when MB was used as a cement, the adaptation
percentage increased non-signicantly (p > 0.05). On the other
hand, the coated specimens showed no signicant (p < 0.05)
change in adaptation after thermal cycling with all cement
materials.
Table 2 Cavity adaptation percentage (standard deviation) in each group.
Group
Baseline
2,000 Thermocycles
10,000 Thermocycles
Non-coated
Bistite II DC (BT-NC)
Multi bond II (MB-NC)
SA Luting (SA-NC)
72.4 (14.6)aA
68.0 (17.1) aC
85.2 (14.1) bD*
65.5 (16.7) dA
74.5 (15.5) eC
71.3 (20.0) eE
56.5 (17.0) hB
75.0 (15.7) iC
58.5 (20.0) hF
Coated
Bistite II DC (BT-C)
Multibond II (MB-C)
SA Luting (SA-C)
92.3 (7.5)cG
88.8 (8.5) cH
99.4 (2.0)bI*
91.1 (7.05) fG
90.4 (11.7) fH
98.1 (2.3) gI
89.0 (8.0) jG
90.5 (9.0) jH
97.5 (2.8) kI
In each column, values marked by similar lowercase letters are not signicantly different. In each row, values marked by similar uppercase
letters are not signicantly different. (*) indicates no signicant difference between coated and non-coated groups (three-way ANOVA multiple
comparisons by Bonferroni post-hoc).
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
999
Fig. 4 SS-OCT 2D images, signal proles and conrmatory CLSM images of the same cross-sections for selected specimens
from MB-NC and MB-C groups after 10,000 thermal cycles. (a) B-scan and binary image of the interface for a MB-NC
specimen showing some microgaps at the cavity oor indicated by bright pixels. (b) B-scan and its binarization for MB-C
specimen showing good adaptation. (c) CLSM under 500 and 1250 magnication conrm gap locations identied by OCT
in (a). (d) CLSM of the same section as in (b) shows good sealing in the resin-coated group. (e) A-scan of two different
locations on the same cross-section to show the difference in backscatter signal of areas with (dashed line) and without gap
(solid line). The signal from unsealed interface shows sudden increase in the intensity compared to uniform gradual
attenuation in case of good sealing. (f) A-scan plotted along the line in cross-section (b). The decrease in signal intensity
indicated by blank arrow is caused by low backscattering of light from MB compared to resin composite. In: resin inlay; Ce:
resin cement; RC: resin coat; D: dentin.
4.
Discussion
In this study, OCT was used to detect gaps in tooth-restoration
interface. OCT is a non-invasive diagnostic imaging technique that can give real time, high resolution images using
a safe broadband light source. Nowadays, OCT is being used
in various biomedical applications including dentistry. Previous dental studies had showed the ability of OCT to evaluate
margins of composite restorations without cutting the sample
or using ionizing radiations [21]. OCT is an objective method
that allows evaluation of the same section at different times
in a long-term study.
During the evaluation of tooth-restoration interface, different interfaces were located including dentin-resin coat, resin
coat-cement and cement-inlay interfaces in the coated samples and dentin-cement and cement-inlay interfaces in the
non-coated samples. Among these, the cement-inlay interface was not included in the process of image analysis in this
study. Occasional gaps at this interface were considered to be
internal resin defects.
In this study, image analysis was conducted on 2D images
to provide data through the whole cavity as presented in
Figs. 24. As the light propagates through the sample, it passes
through different materials, undergoing refraction and partial reection. The reection of light as it passes between
two media with different refractive indices (Fresnel reection)
result in a peak in the backscatter signal (A-scan) forming a
bright area in 2D OCT image. The refractive index of a composite resin is dependent on its composition and can be variable
among different materials. According to the GladstoneDale
relation [20], index of refraction can be related to the ratio
and optical constants of the ingredients, which are mainly the
resin matrix and the llers. For example MP has a ller vol% of
82% according to manufacturer, and contains alumina llers
with a high refractive index (n = 1.75), while other composites
with lower ller load contain barium glass ller that has a
lower refractive index (n = 1.52). Moreover, methacrylate resins
1000
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
Fig. 5 Bar graph representing cavity adaptation percentage and standard deviation of each group at baseline (24 h after
cementation), after 2000 thermal cycles and after 10,000 thermal cycles.
Table 3 Measured refractive indices for materials used
in study.
Material
MP
SE + PLF (resin coat)
BT
SA
MB
1.58
1.55
1.50
1.51
1.48
generally have a refractive index of 1.491.55 (for, TEGDMA:
triethyleneglycol dimethacrylate and Bis-GMA: bisphenol-A
diglycidyl ether dimethacrylate, respectively) and PMMA (poly
methyl methacrylate) has a refractive index of 1.48, according
to various technical reports.
Refractive indices of different materials used in this study
were measured following the methodology explained in
details elsewhere [17,20]. Briey, a thin slice of each material
(approximately 300 m) is prepared and imaged by OCT while
placed over a reective metal stage. The refractive index is
then calculated by measuring the ratio of optical path length
through the material to the actual thickness of the slice. The
results from at least 3 measurements were in the range of
1.481.58 as presented in Table 3. These refractive index values
are close to those of dentin [20].
In order to conrm the assumption that an increased signal
intensity at the interface indicated gap due to the refractive index contrast between the material and a low-refractive
index medium such as air (n = 1.0), further investigation was
carried out by imaging the specimens after each step of the
inlay placement. Representative OCT images of the specimen
after DBS was applied and following placement of the PLF are
shown in Fig. 6a and c, that suggest the surface of the applied
coating is highly reective while little additional reection
is rising from the underlying dentin interface showing good
initial adaptation of the resin coating to the surface of dentin.
The composite inlays were fabricated on the prepared cavity after using a plastic parafn lm separator mold into the
cavity. It should be mentioned that replacing the impression
step of an indirect technique by this method shortened the
fabrication time but could also have yielded a thicker resin
cement layer. An OCT image of an inlay placed without any
resin cement to check its t is presented in Fig. 6e. As clearly
indicated by the signal intensity prole (Fig. 6f), absence of any
intermediate cement layer leads to high light reection from
the border of composite and dentin resulting in the appearance of a double-reection peak where the distance between
two surfaces (i.e. inlay bottom and dentin surface) is wide
enough. It was previously reported that since the reections
are resulting from the double refraction at the borders of the
defect, the vertical dimension of the target pixels may not indicate the vertical dimension of the gap between two interfaces
under this experiment setup, while the horizontal dimension correlated well with the extent of the unsealed portion
of the interface [21]. Therefore, the percentage of gap in this
study was calculated as the total horizontal length of the target pixels in the selected interface after removing the noise
by a median lter. The custom software was used to detect
bright clusters indicating increase in the signal intensity in
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
1001
Fig. 6 (a) Cross-sectional OCT image showing prepared cavity after application of DBS (SE). (b) Signal intensity prole along
the designated line in (a). Note that it may be difcult to characterize the thin bonding layer (approximately 10 m; which is
close to the axial resolution of OCT). (c) OCT image after the application of low viscosity microlled resin (PLF) to form the
resin coat; blank arrow indicates pulp horn. Note that the resin has been applied twice to result in a thicker layer for the
purpose of OCT imaging. Corresponding A-scan in (d) indicates good sealing of the resin coat with no increase in
backscatter signal intensity. (e) OCT image showing the inlay inserted into a prepared cavity with no cement or resin coat to
check for t. Note the clear reections from the boundary of the cavity. (f) Double peak in signal intensity prole caused by
the boundaries of air-lled space, the inlay (top boundary, rst bold arrow) and dentin (lower boundary, second bold arrow).
(g) In the left image, previously cured layer of the resin placed over dentin shows a strong reection from the interface; the
intensity peak indicated by bold arrow in (h) conrms the gap, which can not be seen in the right image where the resin
cement was adequately pushed against the dentin surface prior to light-curing. The blank arrow in (h) shows signal peak
caused by surface reection from the resin cement due to its contrast in refractive index with air.
restoration interface [13]. This software requires the user to
determine an intensity limit to detect the target pixels in the
area of interest that includes the resin interface in this study.
The target pixels are those with high brightness in a binarized
image.
To further rule out the possibilities of bias in the detection of gaps, OCT images of the resin cement layer (without
inlay) placed over dentin are presented in Fig. 6g and h. A
gap between the cement and dentin was simply created by
curing the resin cement as a separate layer on a glass slide
and then placing the cured cement layer over dentin. In this
case, a strong reection from the interface is evidently indicating the gap. On the other hand, when the resin cement was
adequately pushed against the dentin surface and then lightcured, no intensity peak was detected at the interface. Some
previous studies have suggested the application of metallic
colloids that would highly backscatter the OCT light as a contrast agent applied after placement of the restoration (as in dye
penetration tests) [18]. Others have suggested that the metallic particles should be incorporated into the dentin bonding
agents [27]. However, the results obtained from a series of
research works suggest that such an increased contrast may
not be necessary for assessment of a wide range of resin composites investigated under OCT [12,13,1618,21].
The round cavities were prepared 2 mm in depth [13,18].
It has also been shown that OCT signal attenuation through
composites depends on various compositional factors [28].
In the current study, a posterior composite was selected
and used to fabricate resin inlays; this composite showed
a low attenuation effect and small signal loss through the
2 mm thickness. Nevertheless, bright lines were occasionally
observed within composite inlays. These micro defects are
thought to be produced during the manipulation of the
highly viscous composite [29]. Such scattering in the superior
structures may affect the penetration depth immediately
beneath them [30]. Therefore, the fabricated inlays were
monitored using OCT before cementation to exclude those
with structural voids or defects [31].
The resin coating technique allows for protection and
coverage of the prepared dentin immediately after cavity
preparation reducing postoperative sensitivity and providing
good interfacial adaptation and marginal seal. It was also
shown that in a mechanism essentially similar to direct bonding, a reliable hybrid layer is produced [8,32]. Furthermore,
resin coating enhanced the bond strength of indirect composite cores to pulpal oor dentin in endodontically treated teeth
[33]. The combination of the two-step self-etch adhesive and a
low-viscosity resin, which was employed in the current work,
could provide the highest bond strength of cement to dentin
[32,34]. The resin coating shifted the failure mode from adhesive failure to cohesive failure within the cement [33]. This
points out the clinical signicance of resin coating on sealing of dentin; as even if the restoration fractures, the dentin
remains protected in both vital and non-vital teeth [33].
In this study, the application of resin coating on dentin
resulted in a statistically signicant increase in the adaptation
of the resin cement to dentin (Table 2 or Fig. 5). The additional application of a low-viscosity microlled resin protects
DBS from tearing during removal of temporary restoration. It
also enhances the adhesive polymerization through the diffusion of its free radicals that polymerize uncured resin in the
oxygen inhibited layer [32,35]. Moreover, the resin composite
layer in the coating technique would prevent possibly adverse
interactions that have been reported to occur between residual uncured acidic monomers within the self-etch adhesive
and the aromatic tertiary amine derived from chemical- and
1002
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
dual-cured resin composites. In addition, the low-viscosity
microlled resin with lower ller content combined with a
bonding agent with low modulus of elasticity form a stressbreaking resin layer relieving the polymerization stresses of
cement and leading to better adaptation of the resin inlays
[35]. The association of these factors may have contributed
toward the signicantly higher adaptation percentage of resin
cement to dentin when the surface was coated with DBS and
PLF in comparison with non-coated samples.
Before thermal cycling, SA-NC showed only scarce
unsealed areas indicating good initial seal. MB-NC showed
slightly more unsealed areas in the interface compared to
BT-NC. However, no statistically signicant difference was
observed.
SA is a self-adhesive resin cement; it is known to adhere
to tooth structure without the need of a separate adhesive or etchant. The cement utilizes 10-methacryloxydecyl
dihydrogen phosphate (MDP) functional monomer to achieve
demineralization and bonding to the tooth surface. MDP is
known to have a high chemical bonding potential to hydroxyapatite forming a very stable bond and excellent water
resistance conrmed by the low dissolution rate of its calcium salt in water [3638]. In fact, the acidic monomer is also
included in the primer agent of the DBS, which conditions
the surface by dissolving the smear layer and demineralizing
dentin surface.
BT is a dual-cured resin cement that needs pretreatment
with two different primers. Its optical adaptation was lower
than SA. One reason may be the high ller content and the viscosity of the mixed cement, which may decreased the depth
of penetration into the primed dentin. Other factors related
to application method should be taken into consideration.
Also, residual solvents from primer may create leakage pathway and interfere with monomer polymerization and reduce
mechanical properties leading to poor bonding performance.
After the specimens were subjected to thermal cycling, SANC and BT-NC showed signicant decrease in the adaptation
percentage. This may be related to the difference in thermal
expansion coefcients between cement material and dentin
leading to gap formation or by accelerated hydrolytic degeneration of the cement material [39].
MB is an MMA-based powder-liquid resin cement with a
single-bottle self-etching primer. The primer contains phosphoric acid monomer and borate derivative as a surface
activator. It had the lowest adaptation performance which
may be contributed to the slow rate of its setting chemical
polymerization, and hydrophilic nature of the water-based
primer [40]. However, MB-NC showed no decrease in adaptation after thermal cycling. The heat during thermal aging
may enhance the chemical polymerization of the cement and
stimulate completion of its setting reaction. In addition, water
uptake by the resin cement may result in expansion of the
layer and closure of some microgaps [41,42]. It has been shown
that the water sorption by resin containing hydrophilic components is intense in the rst days after coming to contact
with water, and then gradually plateaus depending on the
composition of the resin [43].
In the coated groups, on the other hand, thermal cycling
did not signicantly inuence the restoration adaptation. This
should be attributed to the reliability of the direct bonding
system used for resin coating in penetrating into dentin and
sealing the interface. SE bond has exhibited good long-term
clinical results and high hydrolytic stability; giving it an edge
over any of the resin cements used alone in this study.
The difference in adaptation among the coated groups
is worth attention, since the same coating was used in all
groups. The nding was attributed to the defects at resin
coat-cement interface, which reects the differences among
the resin cements, such as contraction stresses that develop
under the constrained polymerization condition of the resin
cement [44]. However, since these defects were predominantly
observed in BT-C and MB-C groups, other factors should be
considered. During cementation, each cement was applied
according to the manufactures instructions where primers
were applied as well; the application of the water-based primer
may interfere with polymerization of the hydrophobic cement
and bonding to the resin coat surface. In this context, it is
recommended that for cementation of inlays in the resin coating technique, a water-free resin cement system should be
applied.
In short, the null hypotheses of the study were rejected,
as there were signicant differences in sealing between resin
cements. The use of resin coating technique improved overall interfacial sealing of the resin cements. Thermal aging
affected the interfacial integrity depending on the resin
cement type and coating.
5.
Conclusion
Within the limitation of this in vitro study, the following can
be concluded that OCT is a high-speed imaging technique to
study tooth-indirect composite restoration interface without
the difculties of common leakage tests. Treatment of dentin
surface with resin coating before cementation improves longterm interfacial sealing of indirect restorations placed with
resin cements.
Acknowledgments
This research was supported in part by the Global Center of
Excellence Program, International Research Center for Molecular Science in Tooth and Bone Diseases at Tokyo Medical
and Dental University, partly by grants-in-aid for scientic
research no. 24792019 from the Japan Society for the Promotion of Science and partly by King Abdulaziz University.
references
[1] Wassell RW, Walls AW, McCabe JF. Direct composite inlays
versus conventional composite restorations: three-year
clinical results. Br Dent J 1995;179:3439.
[2] Hickel R, Manhart J. Longevity of restorations in posterior
teeth and reasons for failure. J Adhes Dent 2001;3:4564.
[3] Nikaido T, Nakaoki Y, Ogata M, Foxton R, Tagami J. The
resin-coating technique. Effect of a single-step bonding
system on dentin bond strengths. J Adhes Dent
2003;5:293300.
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
[4] Furukawa K, Inai N, Tagami J. The effects of luting resin
bond to dentin on the strength of dentin supported by
indirect resin composite. Dent Mater 2002;18:13642.
[5] Burrow MF, Nikaido T, Satoh M, Tagami J. Early bonding of
resin cements to dentineffect of bonding environment.
Oper Dent 1996;21:196202.
[6] Momoi Y, Akimoto N, Kida K, Yip KH, Kohno A. Sealing
ability of dentin coating using adhesive resin systems. Am J
Dent 2003;16:10511.
[7] Jayasooriya PR, Pereira PN, Nikaido T, Burrow MF, Tagami J.
The effect of a resin coating on the interfacial adaptation of
composite inlays. Oper Dent 2003;28:2835.
[8] Nikaido T, Kitasako Y, Burrow MF, Umino A, Maruoka R,
Ikeda M, et al. Effect of resin coating on dentin bond
durability of a resin cement over 1 year. Am J Dent
2008;21:648.
[9] Kitasako Y, Burrow MF, Nikaido T, Tagami J. Effect of
resin-coating technique on dentin tensile bond strengths
over 3 years. J Esthet Restor Dent 2002;14:11522.
[10] Ibarra G, Johnson GH, Geurtsen W, Vargas MA. Microleakage
of porcelain veneer restorations bonded to enamel and
dentin with a new self-adhesive resin-based dental cement.
Dent Mater 2007;23:
21825.
[11] Ferracane JL, Stansbury JW, Burke FJ. Self-adhesive resin
cements chemistry, properties and clinical considerations.
J Oral Rehabil 2011;38:295314.
[12] Bakhsh TA, Sadr A, Shimada Y, Mandurah MM, Hariri I,
Alsayed EZ, et al. Concurrent evaluation of composite
internal adaptation and bond strength in a class-I cavity. J
Dent 2013;41:6070.
[13] Bista B, Sadr A, Nazari A, Shimada Y, Sumi Y, Tagami J.
Nondestructive assessment of current one-step self-etch
dental adhesives using optical coherence tomography. J
Biomed Opt 2013;18:076020.
[14] Sun J, Eidelman N, Lin-Gibson S. 3D mapping of
polymerization shrinkage using X-ray micro-computed
tomography to predict microleakage. Dent Mater
2009;25:31420.
[15] De Santis R, Mollica F, Prisco D, Rengo S, Ambrosio L,
Nicolais L. A 3D analysis of mechanically stressed
dentin-adhesive-composite interfaces using X-ray micro-CT.
Biomaterials 2005;26:25770.
[16] Sadr A, Shimada Y, Mayoral JR, Hariri I, Bakhsh TA, Sumi Y,
et al. Swept source optical coherence tomography for
quantitative and qualitative assessment of dental composite
restorations. Proc. SPIE 2011;7884:78840C.
[17] Nazari A, Sadr A, Shimada Y, Tagami J, Sumi Y. 3D
assessment of void and gap formation in owable resin
composites using optical coherence tomography. J Adhes
Dent 2013;15:23743.
[18] Makishi P, Shimada Y, Sadr A, Tagami J, Sumi Y.
Non-destructive 3D imaging of composite restorations using
optical coherence tomography: marginal adaptation of
self-etch adhesives. J Dent 2011;39:31625.
[19] Sinescu C, Negrutiu ML, Todea C, Balabuc C, Filip L, Rominu
R, et al. Quality assessment of dental treatments using
en-face optical coherence tomography. J Biomed Opt
2008;13:054065.
[20] Hariri I, Sadr A, Nakashima S, Shimada Y, Tagami J, Sumi Y.
Estimation of the enamel and dentin mineral content from
the refractive index. Caries Res 2013;47:1826.
[21] Bakhsh TA, Sadr A, Shimada Y, Tagami J, Sumi Y.
Non-invasive quantication of resin-dentin interfacial gaps
using optical coherence tomography: validation against
confocal microscopy. Dent Mater 2011;27:91525.
[22] Nazari A, Sadr A, Campillo-Funollet M, Nakashima S,
Shimada Y, Tagami J, et al. Effect of hydration on assessment
[23]
[24]
[25]
[26]
[27]
[28]
[29]
[30]
[31]
[32]
[33]
[34]
[35]
[36]
[37]
[38]
[39]
[40]
1003
of early enamel lesion using swept-source optical coherence
tomography. J Biophotonics 2013;6:1717.
Nakagawa H, Sadr A, Shimada Y, Tagami J, Sumi Y.
Validation of swept source optical coherence tomography
(SS-OCT) for the diagnosis of smooth surface caries in vitro. J
Dent 2013;41:809.
Imai K, Shimada Y, Sadr A, Sumi Y, Tagami J. Noninvasive
cross-sectional visualization of enamel cracks by optical
coherence tomography in vitro. J Endod 2012;38:126974.
de Melo LS, de Araujo RE, Freitas AZ, Zezell D, Vieira ND,
Girkin J, et al. Evaluation of enamel dental restoration
interface by optical coherence tomography. J Biomed Opt
2005;10:064027.
Gale MS, Darvell BW. Thermal cycling procedures for
laboratory testing of dental restorations. J Dent
1999;27:8999.
Braz AK, de Araujo RE, Ohulchanskyy TY, Shukla S, Bergey
EJ, Gomes AS, et al. In situ gold nanoparticles formation:
contrast agent for dental optical coherence tomography. J
Biomed Opt 2012;17:066003.
Lammeier C, Li Y, Lunos S, Fok A, Rudney J, Jones R.
Inuence of dental resin material composition on
cross-polarization-optical coherence tomography imaging. J
Biomed Opt 2012;17:106002.
Al-Sharaa KA, Watts DC. Stickiness prior to setting of some
light cured resin-composites. Dent Mater 2003;19:
1827.
Wang RK. Signal degradation by multiple scattering in
optical coherence tomography of dense tissue: a Monte
Carlo study towards optical clearing of biotissues. Phys Med
Biol 2002;47:228199.
Nazari A, Sadr A, Saghiri MA, Campillo-Funollet M, Hamba
H, Shimada Y, et al. Non-destructive characterization of
voids in six owable composites using swept-source optical
coherence tomography. Dent Mater 2013;29:27886.
Jayasooriya PR, Pereira PN, Nikaido T, Tagami J. Efcacy of a
resin coating on bond strengths of resin cement to dentin. J
Esthet Restor Dent 2003;15:10513.
Ariyoshi M, Nikaido T, Foxton RM, Tagami J. Microtensile
bond strengths of composite cores to pulpal oor dentin
with resin coating. Dent Mater J 2008;27:4007.
Nikaido T, Cho E, Nakajima M, Tashiro H, Toba S, Burrow MF,
et al. Tensile bond strengths of resin cements to bovine
dentin using resin coating. Am J Dent 2003;16(Spec
No):41A6A.
Belli S, Inokoshi S, Ozer F, Pereira PN, Ogata M, Tagami J. The
effect of additional enamel etching and a owable
composite to the interfacial integrity of Class II adhesive
composite restorations. Oper Dent 2001;26:705.
Inoue S, Koshiro K, Yoshida Y, De Munck J, Nagakane K,
Suzuki K, et al. Hydrolytic stability of self-etch adhesives
bonded to dentin. J Dent Res 2005;84:11604.
Yoshida Y, Nagakane K, Fukuda R, Nakayama Y, Okazaki M,
Shintani H, et al. Comparative study on adhesive
performance of functional monomers. J Dent Res
2004;83:4548.
Van Landuyt KL, Yoshida Y, Hirata I, Snauwaert J, De Munck
J, Okazaki M, et al. Inuence of the chemical structure of
functional monomers on their adhesive performance. J Dent
Res 2008;87:75761.
Piwowarczyk A, Bender R, Ottl P, Lauer HC. Long-term bond
between dual-polymerizing cementing agents and human
hard dental tissue. Dent Mater 2007;23:2117.
Nurrohman H, Nikaido T, Takagaki T, Sadr A, Waidyasekera
K, Kitayama S, et al. Dentin bonding performance and ability
of four MMA-based adhesive resins to prevent
demineralization along the hybrid layer. J Adhes Dent
2012;14:33948.
1004
d e n t a l m a t e r i a l s 3 0 ( 2 0 1 4 ) 9931004
[41] Nurrohman H, Nikaido T, Sadr A, Takagaki T, Kitayama S,
Ikeda M, et al. Long-term regional bond strength of three
MMA-based adhesive resins in simulated vertical root
fracture. Dent Mater J 2011;30:65563.
[42] Bitter K, Meyer-Lueckel H, Priehn K, Kanjuparambil JP,
Neumann K, Kielbassa AM. Effects of luting agent and
thermocycling on bond strengths to root canal dentine. Int
Endod J 2006;39:80918.
[43] Takahashi M, Nakajima M, Hosaka K, Ikeda M, Foxton RM,
Tagami J. Long-term evaluation of water sorption and
ultimate tensile strength of HEMA-containing/-free one-step
self-etch adhesives. J Dent 2011;39:50612.
[44] Feilzer AJ, De Gee AJ, Davidson CL. Increased wall-to-wall
curing contraction in thin bonded resin layers. J Dent Res
1989;68:4850.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- 2012 AICPA Financial QuestionsDocument59 pages2012 AICPA Financial QuestionsJimsy AntuNo ratings yet
- By Emile Alline: Technical Art by Fred WolffDocument4 pagesBy Emile Alline: Technical Art by Fred WolffJim100% (3)
- CD1 ISO/IEC 17000 Conformity Assessment - Vocabulary and General PrinciplesDocument26 pagesCD1 ISO/IEC 17000 Conformity Assessment - Vocabulary and General PrinciplesMAC CONSULTORESNo ratings yet
- Tailwind OperationsDocument3 pagesTailwind Operationsiceman737No ratings yet
- Crafting and Executing StrategyDocument33 pagesCrafting and Executing Strategyamoore2505No ratings yet
- Siart, Et. Al (2018) Digital GeoarchaeologyDocument272 pagesSiart, Et. Al (2018) Digital GeoarchaeologyPepe100% (2)
- Production of Formaldehyde From MethanolDocument200 pagesProduction of Formaldehyde From MethanolSofia Mermingi100% (1)
- Correlation Between Polymerization Stress and Interfacial Integrity of Composites Restorations Assessed by Different in Vitro TestsDocument9 pagesCorrelation Between Polymerization Stress and Interfacial Integrity of Composites Restorations Assessed by Different in Vitro TestsNeelima SonawaneNo ratings yet
- Application Form: Student SSC DetailsDocument3 pagesApplication Form: Student SSC DetailsShrikrishna BirajdarNo ratings yet
- Chocolate IndustryDocument71 pagesChocolate IndustryHem Thapar50% (8)
- Diploma New Admission FormDocument3 pagesDiploma New Admission FormNeelima SonawaneNo ratings yet
- Annual Report 2007 2008Document84 pagesAnnual Report 2007 2008Neelima SonawaneNo ratings yet
- Application DetailsDocument2 pagesApplication DetailsNeelima SonawaneNo ratings yet
- Case Study - Jamie Turner at MLI Inc.Document11 pagesCase Study - Jamie Turner at MLI Inc.Neelima Sonawane50% (2)
- MBA CET 2013-2015 Model Question Paper For Offline ExamDocument6 pagesMBA CET 2013-2015 Model Question Paper For Offline ExamNeelima SonawaneNo ratings yet
- Holacracy FinalDocument24 pagesHolacracy FinalShakil Reddy BhimavarapuNo ratings yet
- ADL MATRIX STRATEGY FOR BPCL'S GROWTHDocument17 pagesADL MATRIX STRATEGY FOR BPCL'S GROWTHSachin Nagar100% (1)
- E 74 - 06 - For Force Measuring InstrumentsDocument12 pagesE 74 - 06 - For Force Measuring InstrumentsSarvesh MishraNo ratings yet
- DrdoDocument2 pagesDrdoAvneet SinghNo ratings yet
- E Requisition SystemDocument8 pagesE Requisition SystemWaNi AbidNo ratings yet
- Critical Thinking Essay-Animal Testing: Rough DraftDocument10 pagesCritical Thinking Essay-Animal Testing: Rough Draftjeremygcap2017No ratings yet
- Quiz 1Document3 pagesQuiz 1JULIANNE BAYHONNo ratings yet
- Philippine Popular Culture in HEIsDocument9 pagesPhilippine Popular Culture in HEIsNokie TunayNo ratings yet
- 21st Century Literature Exam SpecsDocument2 pages21st Century Literature Exam SpecsRachel Anne Valois LptNo ratings yet
- Gentle Classical Nature Sample - Units1 and 2Document129 pagesGentle Classical Nature Sample - Units1 and 2Carita HemsleyNo ratings yet
- J05720020120134026Functions and GraphsDocument14 pagesJ05720020120134026Functions and GraphsmuglersaurusNo ratings yet
- Dewatering Well PointsDocument4 pagesDewatering Well Pointssalloum3No ratings yet
- 1993 - Kelvin-Helmholtz Stability Criteria For Stratfied Flow - Viscous Versus Non-Viscous (Inviscid) Approaches PDFDocument11 pages1993 - Kelvin-Helmholtz Stability Criteria For Stratfied Flow - Viscous Versus Non-Viscous (Inviscid) Approaches PDFBonnie JamesNo ratings yet
- PMMAEE Application FormDocument2 pagesPMMAEE Application Formshiero501100% (15)
- University Reserch Worksheet PDFDocument7 pagesUniversity Reserch Worksheet PDFapi-410567922No ratings yet
- Calculating Molar MassDocument5 pagesCalculating Molar MassTracy LingNo ratings yet
- HRM Assignment Final - Case StudyDocument7 pagesHRM Assignment Final - Case StudyPulkit_Bansal_2818100% (3)
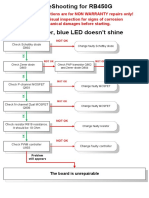
- RB450G Trouble ShootingDocument9 pagesRB450G Trouble Shootingjocimar1000No ratings yet
- GCSE H3 02g4 02 3D TrigonometryDocument2 pagesGCSE H3 02g4 02 3D TrigonometryAndrei StanescuNo ratings yet
- Catalogue: Product Offering 51Document56 pagesCatalogue: Product Offering 51Bruno MartinsNo ratings yet
- Click To Edit Master Title Style: Uggas, Heinz Gerhard A. Sabroso, Dionisio Jr. L. Reyes, Jeboy ODocument21 pagesClick To Edit Master Title Style: Uggas, Heinz Gerhard A. Sabroso, Dionisio Jr. L. Reyes, Jeboy ODionisio SabrosoNo ratings yet
- Use DCP to Predict Soil Bearing CapacityDocument11 pagesUse DCP to Predict Soil Bearing CapacitysarvaiyahimmatNo ratings yet
- Vega Plus 69Document3 pagesVega Plus 69yashNo ratings yet
- The Critical Need For Software Engineering EducationDocument5 pagesThe Critical Need For Software Engineering EducationGaurang TandonNo ratings yet