Professional Documents
Culture Documents
2009 Improving Poststroke Recovery, Neuroplasticity and Task-Oriented Training
Uploaded by
Ani Fran SolarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2009 Improving Poststroke Recovery, Neuroplasticity and Task-Oriented Training
Uploaded by
Ani Fran SolarCopyright:
Available Formats
Improving Poststroke Recovery:
Neuroplasticity and
Task-Oriented Training
Richard L. Harvey, MD
Corresponding author
Richard L. Harvey, MD
Stroke Rehabilitation Center, The Rehabilitation Institute of Chicago,
345 East Superior Street, Chicago, IL 60611, USA.
E-mail: rharvey@ric.org
Current Treatment Options in Cardiovascular Medicine 2009, 11:251259
Current Medicine Group LLC ISSN 1092-8464
Copyright 2009 by Current Medicine Group LLC
Opinion statement
Neurorehabilitation is a critical part of the overall process to achieve optimal
outcome after stroke. Presently, the eld of neurorehabilitation is in transition.
New research suggesting novel approaches to optimize functional recovery after
stroke is on the horizon, but clear knowledge of the underlying mechanisms of
this recovery is still being unraveled. In practice, many rehabilitation centers continue to provide traditional compensatory rehabilitation training while many others are practicing newer, task-oriented approaches. A few centers are incorporating new technology, such as computer-based training devices or robotics, into
rehabilitation care. This transition is happening because neuroscientic research
has shown that neuroplastic changes in the cerebral cortex and in other parts of
the central nervous system (CNS) are necessarily linked to motor skill retraining
in the affected limbs. Task-oriented training that focuses on the practice of skilled
motor performance is the critical link to facilitating neural reorganization and
rewiring in the CNS. Therefore, whenever possible, task-oriented training at an
intense level should be incorporated into the rehabilitation program of any patient
with stroke-related motor decits. Two such task-oriented therapies that should
be available at all neurorehabilitation centers are constraint-induced movement
therapy and body weightsupported treadmill training. The optimal intensity of
training (frequency and duration) is still not clear but is certainly greater than that
available in clinical programs. Therefore, the incorporation of automated training
devices will be necessary in the future. However, the engineering necessary to
make these devices effective, easy to use, affordable, and portable remains a challenge for the next decade of neurologic bioengineering research.
Introduction
With improved acute stroke care and secondary prevention,
people with stroke can expect to live longer. There now
are approximately 5.8 million people living with stroke in
the United States, and this prevalence keeps growing [1].
Although 90% of stroke survivors will walk again, with or
without a device, many are challenged because of problems
with balance, motor control, and slow walking speed [2].
Only 50% of people with hemiplegia regain functional
arm use, and fewer than 20% achieve good arm and hand
recovery [3]. Early approaches to addressing the functional
problems of stroke survivors with hemiplegia focused primarily on compensatory training. Thus, persons who had
difficulty dressing because of hemiplegia were trained to
put on clothes, button shirts, and tie shoes with one hand.
Ambulation training involved assistive devices, the use of
ankle orthotics, extensive work on trunk posture, control
of limb dystonia, and careful transition to standing and
weight bearing on the weak lower limb.
These techniques are still common and important
aspects of comprehensive physical rehabilitation post
252 Cerebrovascular Disease and Stroke
stroke. However, today there also is a growing interest in the phenomenon of neuroplasticity following
central nervous system (CNS) injury and its critical
link to task-oriented training. Neuroplasticity is the
capacity of the CNS to modulate its physiology and
anatomy at the cellular level in response to several
internal and external events. Behavioral experience
has been shown to be a potent trigger to neuroplastic change, most notably in the cerebral cortex [47].
Task-oriented training is a form of motor learning that
focuses on skill acquisition in the context of a particular functional activity. Skill is the ability to achieve
a goal with consistency, flexibility, and efficiency [8].
Following stroke, task-oriented training results in
motor relearning by enhancing skill in meaningful
functional activities and is associated with presumably
adaptive neuroplastic changes in the cerebral cortex,
brainstem, cerebellum, and spinal cord [4,5,7,9].
This article describes several novel rehabilitation
techniques that improve motor function in patients
with hemiplegia and proposes a theoretical framework
for motor recovery after stroke. It also discusses functional relearning in the upper limb and the recovery of
walking ability.
Task-oriented training
Task-oriented training in the hemiplegic upper limb
In 1949, psychologist Donald O. Hebb [10] described learning as a
neural process whereby if one cell repeatedly assists in firing another, the axon of the first cell develops synaptic knobs (or enlarges them
if they already exist) in contact with the soma of the second cell.
This concept, later described as Hebbian learning, was scientifically
proven in 1979 by Bliss and Lomo [11,12] in rat hippocampus, in
which they demonstrated that repeated stimulation of the perforant
pathway fibers that innervate the granule cells of the dentate area
results in long-term potentiation (LTP) in response to a single stimulus. LTP also occurs in the premotor and primary motor cortex (M1)
in response to an increase in neural activity and is an essential part
of motor learning and cortical remodeling [13,14]. The strengthening
of synaptic connectivity, especially between intracortical interneurons, and the expansion of movement representations in the motor
cortex occur in response to motor learning, in both the intact and the
injured brain [1416].
A prime example of neuroplasticity and its connection to motor relearning was demonstrated by Nudo and Milliken [16] in 1996 using
intracortical microstimulation to map out hand representation in the
M1 cortex of nonhuman primates (squirrel monkeys). The monkeys
were trained using their dominant upper limb in a skilled reaching and
grasping task that required digital manipulation. After inducing lesions
in the M1 cortex hand region, the researchers found that monkeys
forced to retrain in the task showed reorganization within the remaining movement representation surrounding the lesion site. Those not
trained showed a loss of hand representation. Motor relearning required
the application of a restraint to the nondominant upper limb to prevent
practice with the unimpaired hand, thus constraining the monkeys to
practice repetitively with the impaired limb.
Also, beginning in 1993, Taub et al. [17,18] ran a series of studies
evaluating the use of constraint-induced movement therapy (CIMT) to
improve motor relearning in adults with chronic stroke-related upper
limb hemiplegia. In these experiments, subjects wore a restraint on their
unimpaired upper limb for 90% of waking hours over a 2-week period.
During that time, the subjects also participated in rehabilitation therapy
6 hours a day over the 10 working days of the 2-week trial. Those who
participated in CIMT improved in functional hand use on standardized
laboratory tests and in real-world hand use, and they retained these
skills for up to 2 years post treatment.
Improving Poststroke Recovery: Neuroplasticity and Task-Oriented Training
Harvey
253
Recently, the Extremity Constraint-Induced Therapy Evaluation (EXCITE)
trial, a large randomized controlled clinical trial with 1-year follow-up,
confirmed the efficacy of CIMT in subacute patients who were 3 to 9
months post stroke [19]. The subjects had to have at least 10 of active
wrist and finger/thumb extension. Those in the investigational group wore
a restraint mitt on the unimpaired upper limb over a 2-week period and
were given the signature CIMT therapy protocol as described previously.
The control subjects received only usual care. Again, the investigational
subjects showed significant improvement in hemiplegic upper limb use
following the 2-week treatment, whereas control subjects did not. Differences in functional use were maintained throughout the 1-year follow-up.
Variations in CIMT have been studied as well. Providing therapy for 3
hours instead of 6 also results in significantly improved functional use, but
not to the extent of that seen with the longer treatment day [20]. Providing
an equivalent dose of CIMT distributed over several weeks rather than
intensively over a 2-week period also shows promise and fits better with
the distribution of therapy typically seen in an outpatient setting [21,22].
Whether CIMT provided in the very early acute rehabilitation setting after
stroke improves motor recovery is still being investigated [23].
In patients who do not meet the criterion for CIMTthat is, those who
lack active hand movementthere is some evidence that neuromuscular
electrical stimulation (NMES) to the wrist and fingers may have some
efficacy in improving hand movement; however, this therapy seems to be
more effective in those with the least neurologic impairment [24,25]. There
presently is no clear evidence that therapy with NMES can improve functional arm use after stroke [26]. Functional hand training with the use of a
neuroprosthesis that is easily applied to the hemiplegic wrist and hand and
inducing hand opening with NMES have shown some short-term efficacy
[27], especially during the acute phase of stroke recovery [28], and may be
beneficial in patients with minimal wrist or finger movement [29].
Another new method of forced-use training of the hemiplegic upper limb is
the application of robotics and other mechanical devices. The advantage of
these devices is that intensive repetitive arm training can be provided to the
patient with very little supervision from the therapist. These devices do not
fatigue during intensive training as a therapist might, may cost less per hour
of use, and potentially measure improvement in skill very accurately [30].
The MIT-Manus (InMotion2 robot; Interactive Motion Technologies, Inc.,
Cambridge, MA) can provide shoulder and elbow training when the patients
forearm and hand are attached to the robots arm. Exercises are performed
in the horizontal plane with an interactive computer screen as the patient
reaches for targets. This device can facilitate improved arm movement and
strength [31,32]. Another robot, called the Mirror Image Movement Enabler,
can provide assisted and resisted arm movements in multiple planes and
is more effective than conventional therapy in improving free arm movement [33]. Other robotic devices include the Assisted Rehabilitation and
Measurement Guide [34] and a bimanual training robot [35]. Hemiplegic
arm training also has been tested using a computer gaming system (virtual
reality) with a device called the T-WREX (Training-Wilmington Robotic
Exoskeleton), which provides an adjustable exoskeletal arm that passively
counterbalances the weight of the arm with elastic bands. This device, now
available commercially as Armeo (Hocoma Inc., Rockland, MA), has shown
some efficacy and is quite motivating for patients to use as they practice arm
movements while a virtual hand performs tasks on the computer screen [36].
Although robotic and virtual reality systems may have efficacy for upper
limb motor relearning, their use is limited by their cost. Additionally, robotic
training of digit manipulation and precision hand function is not yet feasible.
254 Cerebrovascular Disease and Stroke
These novel interventions for task-oriented motor relearning demonstrate that with intensive repetitive skill training, patients with acute and
chronic upper limb hemiplegia can regain and maintain some potentially
functional movement of the hemiplegic arm. Future research will explore
the most practical ways to facilitate this type of training using combinations of CIMT techniques, NMES, robotic devices, and virtual reality.
Task-oriented gait training and the recovery of walking after stroke
Following stroke, there are neurologic changes in the hemiplegic lower limb
that disrupt gait function. In addition to weakness, the essential problem in
hemiplegic gait is the abnormal timing of muscle contraction and relaxation
throughout the gait cycle [37]. Most simply, the quadriceps muscles remain
active through most of the gait cycle, including the swing phase, when the
limb is advanced toward the next step. In addition, the gastrocnemiussoleus complex and ankle inverters turn on during the swing phase but often
fail to provide stability during the stance phase of gait. If the patient does
not have a severe problem with dynamic standing balance, these muscle
timing problems typically do not prevent walking, but they do cause a slow,
stiff-kneed, asymmetric gait that does not accommodate well to perturbations or uneven walking surfaces [38]. The best rehabilitation technique
for walking after stroke is to walk, but the practice of walking over ground
often is hampered by the patients unwillingness to bear much weight on
the hemiplegic lower limb, his or her own fear of falling, and the real safety
concern of having a patient walk at a faster pace.
In the past decade, there has been increasing interest in the use of several
treadmill systems to safely improve walking in patients with hemiplegia.
The most common gait restoration system available in physical therapy
clinics is body weightsupported treadmill training (BWSTT). The practice of gait training on a treadmill with a body weight support system
was first described by Finch and Barbeau [39] in 1985 and first tested
as a gait restoration therapy for stroke by Hesse et al. [40] in 1994.
The concept of restoring walking ability using BWSTT originated from
studies examining preserved locomotor function in spinalized cats [4].
Paraplegic cats with spinal cord lesions maintain stepping ability when
placed on a treadmill. This locomotor ability is supported by presumed
spinal circuitry called the spinal central pattern generator, described by
Grillner and Wallen [41] and verified in lower vertebrate models [7].
BWSTT uses a standard treadmill and an overhead counterweighted
cable system with a rock climbingstyle harness (Fig. 1). Patients with
stroke-related hemiplegia can be placed in the harness with overhead
support while standing on the treadmill. The counterweighting system
can unload up to 40% of the patients weight. With the treadmill in
motion, the patient can then practice a reciprocal walking pattern. To
avoid dragging the hemiplegic leg, the therapist may need to assist in
advancing the weak limb through the gait cycle. As training proceeds,
the therapist can withdraw assistance to the hemiplegic leg, progressively
reduce body support down to 0%, and increase the treadmill speed.
Gait retraining using BWSTT has shown efficacy. It clearly is superior
to traditional rehabilitation therapies for stroke, such as neurodevelopmental techniques in which patients practice balance and weight bearing before stepping and walking [42]. Patients who train with BWSTT
also achieve better gait speed, improve balance, and have better motor
recovery than patients trained with over-ground walking, resistive leg
cycling, or treadmill walking without body weight support [43,44].
Improving Poststroke Recovery: Neuroplasticity and Task-Oriented Training
Harvey
255
Figure 1. Body weightsupported treadmill
training. The patient has up to 40% of load
off his body weight with a counterweight
system and harness. The treadmill speed can
be adjusted over time. The therapist often
must assist in advancing the hemiplegic leg
with every step.
A recent study indicates that the addition of timed electrical stimulation of the hemiplegic lower limb muscles during BWSTT may further
facilitate recovery of over-ground walking [45].
Unfortunately, the amount of time a patient can use BWSTT is limited by
the amount of physical effort the therapist can tolerate in a session during
which he or she provides assistance in advancing the weak leg. In practice,
therapists fatigue after 15 to 20 minutes. To resolve this problem, there have
been efforts to design robotic systems to replace the need for physical assistance from the clinician. One such system, called the Lokomat (Hocoma
Inc., Rockland, MA), is a treadmill with a counterbalanced harness system
256 Cerebrovascular Disease and Stroke
Table 1. Six principles of task-oriented motor training necessary to
achieve improved motor skill and perhaps function
Specicity of training
Constrained use of the impaired limbs
Mass practice (repetition)
Shaping of skill
Saliency of task
Knowledge of performance and results
plus a motor-driven leg orthosis that produces a reciprocal walking pattern
timed with the motion of the treadmill belt. Thus, it can produce a near-normal walking pattern, even in nonambulatory patients and without human
assistance. The Lokomat has been tested in patients with stroke, demonstrating efficacy equivalent to that of the neurodevelopmental technique
described earlier [46], but it is inferior to therapist-assisted BWSTT without
the robot [47]. The likely reason that Lokomat fails in comparison with
BWSTT is that the robot does not challenge the patient to put any effort
into walking during training, whereas in BWSTT, the therapist plays a key
role in progressively removing supportive assistance.
Most stroke patients will practice walking over ground once they can
do so safely. However, there is still a role for treadmill walking without
body weight support in patients who are functional ambulators. Treadmill exercise enhances gait speed and aerobic capacity in patients with
stroke and can facilitate gait-related neuroplastic changes based on functional MRI [48]. Structured episodic speed training on the treadmill
also may improve over-ground walking speed significantly [49].
The principles of task-oriented training after stroke
The preceding examples of task-oriented motor training highlight certain principles that likely apply to any intervention that may be expected
to improve motor control and function after stroke [50]. These principles are listed in Table 1. First, task-oriented training must focus on
the task being learned. Thus, there is specificity in motor learning. For
example, walking skill is best achieved by treadmill training, then by leg
cycling or merely strengthening the lower limbs [43].
Second, as highlighted by CIMT, the patient must be constrained to
perform the functional task during training with the impaired limbs.
In addition, the patient should not be able to perform compensatory
techniques to achieve the therapeutic goal. For example, in CIMT, the
patients unimpaired hand is restrained so that it does not inadvertently
assist the impaired hand while performing training tasks. In BWSTT, the
patient is in a supported harness with feet on the treadmill while the belt
is running, which constrains the patient to walk. The therapist assists
only to assure proper advancement of the impaired leg.
Third is the principle of mass practice, described by Taub et al. [51] in
the context of CIMT. Repetition of training facilitates learning. The
intensity of multiple repetitions of a task solidifies neuroplastic changes
in the CNS and improves performance.
The fourth principle, shaping, a term from behavioral psychology, is
the process of progressively increasing the complexity of a functional
task by successive approximations over time. Patients with stroke, when
attempting a novel task, will be frustrated easily if it is too difficult. By
Improving Poststroke Recovery: Neuroplasticity and Task-Oriented Training
Harvey
257
breaking the task down into parts and starting with the simplest motor
tasks first, the therapist can increase the complexity over time until the
patient can complete the functional skill, always challenging the patient
within tolerable limits.
Fifth, the tasks being learned should be salient to the patient. The relative importance of a functional task to the patient stimulates motivation
to learn and practice. Walking is a vital task for most stroke patients,
and motivation for training is always high. For upper limb training,
making a meal may be important to one patient but not to another.
Playing cards may be essential to a patient whose social life is structured
around playing bridge with friends. The tasks used to train a patient
should be selected based on the patients goals and personal needs.
Finally, knowledge of performance and results is well known to be
important in motor learning [52]. For example, it would be difficult to
learn how to serve a tennis ball if one never saw where the ball landed
following an attempted serve. Good coaching and feedback on the
serving technique may be vital to achieving a high-quality serve. Feedback also is critical in motor learning after stroke. In most cases, this
is provided directly by the therapist, but there is growing interest in
enhancing sensory feedback during motor training to improve learning
and outcome [53]. The best means for providing enhanced sensorimotor
feedback remains under investigation.
Disclosure
No potential conflict of interest relevant to this article was reported.
References and Recommended Reading
Papers of particular interest, published recently,
have been highlighted as:
Of importance
Of major importance
1.
2.
3.
4.
5.
6.
7.
Rosamond W, Flegal K, Furie K, et al.: Heart disease
and stroke statistics2008 update: a report from the
American Heart Association Statistics Committee and
Stroke Statistics Subcommittee. Circulation 2008, 117:
e25e146.
Reding MJ, Potes E: Rehabilitation outcome following initial
unilateral hemispheric stroke. Stroke 1988, 19:13541358.
Kwakkel G, Kollen BJ, van der Grond J, Prevo AJH:
Probability of regaining dexterity in the flaccid upper limb:
impact of severity of paresis and time since onset in acute
stroke. Stroke 2003, 34:21812186.
Edgerton VR, Tillakaratne NJK, Bigbee AJ, et al.: Plasticity
of the spinal neural circuitry after injury. Ann Rev Neurosci
2004, 27:145167.
Nudo RJ, Milliken GW, Jenkins GW, Merzenich MM:
Use-dependent alterations of movement representations in
primary motor cortex of adult squirrel monkeys. J Neurosci
1996, 16:785807.
Rosenkranz K, Kakar A, Rothwell JC: Differential modulation of motor cortical plasticity and excitability in early
and late phases of human motor learning. J Neurosci 2007,
27:1205812066.
Wolpaw JR, Tennissen AM: Activity-dependent spinal cord
plasticity in health and disease. Ann Rev Neurosci 2001,
24:807843.
8.
9.
10.
11.
12.
13.
14.
15.
Winstein CJ, Wolf SL: Task-oriented training to promote upper extremity recovery. In Stroke Recovery and
Rehabilitation. Edited by Stein J, Harvey RL, Macko RF,
et al. New York: Demos Medical; 2008:267290.
Nudo RJ: Postinfarct cortical plasticity and behavioral
recovery. Stroke 2007, 38:840845.
Hebb DO: The Organization of Behavior. New York:
Wiley; 1949.
Bliss TVP, Collingridge GL: A synaptic model of memory:
long-term potentiation in the hippocampus. Nature 1993,
361:3139.
Bliss TVP, Lomo T: Long-lasting potentiation of synaptic
transmission in the dentate area of the anaesthetized rabbit
following stimulation of the perforant path. J Physiol 1973,
232:331356.
Hess G: Synaptic plasticity of local connections in rat motor
cortex. Acta Neurobiol Exp (Wars) 2003, 63:271276.
Monofils MH, VandenBerg PM, Kleim JA, Teskey GC:
Long term potentiation induces expanded movement
representations and dendritic hypertrophy in layer V of rat
sensorimotor neocortex. Cerebral Cortex 2004, 14:586593.
Kleim JA, Barbay S, Cooper NR, et al.: Motor learning-dependent synaptogenesis is localized to functionally reorganized
motor cortex. Neurobiol Learning Mem 2002, 77:6377.
258 Cerebrovascular Disease and Stroke
16.
Nudo RJ, Milliken GW: Reorganization of movement
representations in primary motor cortex following focal
ischemic infarcts in adult squirrel monkeys. J Neurophysiol
1996, 75:21442149.
17.
Taub E, Miller NE, Novack TA, et al.: Technique to
improve chronic motor deficit after stroke. Arch Phys Med
Rehabil 1993, 74:347354.
18.
Taub E, Uswatte G, King DK, et al.: A placebo-controlled
trial of constraint-induced movement therapy for upper
extremity after stroke. Stroke 2006, 37:10451049.
19. Wolf SL, Winstein CJ, Miller JP, et al.: Effect of constraintinduced movement therapy on upper extremity function 3-9
months after stroke: The EXCITE randomized clinical trial.
JAMA 2006, 296:20952104.
This is a report of a randomized controlled trial of 222 patients with
subacute stroke who received 2 weeks of CIMT or usual care. Subjects receiving the intensive task-oriented training made signicant
improvements in hemiplegic hand use, which were retained for up to
1 year following treatment.
20.
Sterr A, Elbert T, Berthold I, et al.: Longer versus shorter
daily constraint-induced movement therapy of chronic
hemiparesis: an exploratory study. Arch Phys Med Rehabil
2002, 83:13741377.
21.
Dettmers C, Teske U, Hamzei F, et al.: Distributed form of
constraint-induced movement therapy improves functional
outcome and quality of life after stroke. Arch Phys Med
Rehabil 2005, 86:204209.
22.
Page SJ, Sisto S, Levine P, McGrath RE: Efficacy of modified
constraint-induced movement therapy in chronic stroke:
a single blinded randomized control trial. Arch Phys Med
Rehabil 2004, 85:1418.
23.
Dromerick AW, Edwards DF, Hahn EM: Does the application of constraint-induced movement therapy during acute
rehabilitation reduce arm impairment after ischemic stroke?
Stroke 2000, 31:29842988.
24.
Cauraugh JH, Light K, Kim S, et al.: Chronic motor dysfunction after stroke: recovering wrist and fi nger extension
by electromyography-triggered neuromuscular stimulation.
Stroke 2000, 31:13601364.
25.
Kimberely TJ, Lewis SM, Auerbach EJ, et al.: Electrical
stimulation driving functional improvements and cortical changes in subjects with stroke. Exp Brain Res 2004,
154:450460.
26.
de Kroon JR, van der Lee JH, Ijzerman MJ, Lankhorst
GJ: Therapeutic electrical stimulation to improve motor
control and functional abilities of the upper extremity
after stroke: a systematic review. Clin Rehabil 2002,
16:350 360.
27.
Alon G, Ring H: Gait and hand function enhancement
following training with a multisegment hybrid orthosis
stimulation system in stroke patients. J Stroke Cerebrovasc
Dis 2003, 12:209216.
28.
Popovic DB, Popovic MB, Sinkjaer A, Schwirtlich L:
Therapy of paretic arm in hemiplegic subjects augmented
with a neural prosthesis: a cross-over study. Can J Phys
Pharm 2004, 82:749756.
29.
Dunning K, Berberich A, Albers B, et al.: A four-week,
task-specific neuroprosthesis program for a person with no
active wrist or fi nger movement because of chronic stroke.
Phys Ther 2008, 88:397405.
30.
Stein J, Hughes R, Fasoli SE, et al.: Technological aids for
motor recovery. In Stroke Recovery and Rehabilitation.
Edited by Stein J, Harvey RL, Macko RF, et al. New York:
Demos Medical; 2008.
31.
Fasoli SE, Krebs HI, Stein J: Effects of robotic therapy on
motor impairment and recovery in chronic stroke. Arch
Phys Med Rehabil 2003, 84:477482.
32.
Volpe BT, Krebs HI, Hogan N, et al.: A novel approach to
stroke rehabilitation: robot-aided sensorimotor stimulation.
Neurology 2000, 54:19381944.
33.
Lum PS, Burgar CG, Shor PC, et al.: Robot-assisted
movement training compared with conventional therapy
techniques for the rehabilitation of upper-limb motor
function after stroke. Arch Phys Med Rehabil 2002,
83:952959.
34.
Kahn LE, Lum PS, Rymer WZ, Reinkensmeyer DJ: Robot
assisted movement training for the stroke-impaired arm:
does it matter what the robot does? J Rehab Res Dev 2006,
43:619630.
35.
Hesse S, Werner C, Pohl M, et al.: Computerized arm
training improves the motor control of the severely affected
arm after stroke: a single blinded randomized trial in two
centers. Stroke 2005, 36:19601966.
36.
Sanchez RJ, Liu J, Rao S, et al.: Automating arm movement
training following severe stroke: functional exercises with
quantitative feedback in a gravity-reduced environment.
IEEE Trans Neural Syst Rehabil Eng 2006, 14:378389.
37.
Kautz SA, Brown DA: Relationships between timing of
muscle excitation and impaired motor performance during
cyclical lower extremity movement in post-stroke hemiplegia. Brain 1998, 121:515526.
38.
Knutsson E, Richards C: Different types of disturbed
motor control in gait of hemiparetic patients. Brain 1979,
102:405430.
39.
Finch L, Barbeau H: Hemiplegic gait: new treatment
strategies. Physiother Can 1985, 38:3641.
40.
Hesse S, Bertelt C, Schaffrin A, et al.: Restoration of gait in
nonambulatory hemiparetic patients by treadmill training
with partial body-weight support. Arch Phys Med Rehabil
1994, 75:10871093.
41.
Grillner S, Wallen P: Central pattern generators for
locomotion, with special reference to vertebrates. Ann Rev
Neurosci 1985, 8:233261.
42.
Hesse S, Bertelt C, Jahnke MT, et al.: Treadmill training
with partial body weight support compared with physiotherapy in nonambulatory hemiparetic patients. Stroke
1995, 26:976981.
43.
Sullivan KJ, Brown DA, Klassen T, et al.: Effects of taskspecific locomotor and strength training in adults who were
ambulatory after stroke: results of the STEPS randomized
clinical trial. Phys Ther 2007, 87:15801602.
44.
Visintin M, Barbeau H, Korner-Bitensky N, Mayo NE: A
new approach to retrain gait in stroke patients through
body weight support and treadmill stimulation. Stroke
1998, 29:11221128.
45.
Lindquist ARR, Prado CL, Barros RML, et al.: Gait training combining partial body weight support, a treadmill,
and functional electrical stimulation: effects on poststroke
gait. Phys Ther 2007, 87:11441154.
46.
Husemann B, Muller F, Krewer C, et al.: Effects of
locomotion training with assistance of a robot-driven gait
orthosis in hemiparetic patients after stroke: a randomized
controlled pilot study. Stroke 2007, 38:349354.
47. Hornby TG, Campbell DD, Kahn JH, et al.: Enhanced
gait-related improvements after therapist- versus roboticassisted locomotor training in subjects with chronic stroke:
a randomized controlled study. Stroke 2008, 39:17861792.
This randomized controlled trial evaluated the efcacy of
robot-driven gait training versus therapist-assisted BWSTT. Therapistassisted training was likely superior because subjects were more
challenged in standard BWSTT than in the robotic training.
48. Luft AR, Macko RF, Forrester LW, et al.: Treadmill exercise
activates subcortical neural networks and improves walking
after stroke: a randomized controlled trial. Stroke 2008,
39:33413350.
This study showed that treadmill exercise in ambulatory stroke
patients results in improved over-ground walking velocity and aerobic tness. In addition, trained subjects showed increased cerebellum
and midbrain activation on functional MRI during leg movements
compared with the control group.
Improving Poststroke Recovery: Neuroplasticity and Task-Oriented Training
49.
50.
51.
Pohl M, Mehrholz J, Ritschel C, Ruckriem S: Speed-dependent
treadmill training in ambulatory hemiparetic stroke patients: a
randomized controlled trial. Stroke 2005, 33:553558.
Harvey RL: Motor recovery after stroke: new directions
in scientifi c inquiry. Phys Med Rehabil Clin N Am 2003,
14:S1S5.
Taub E, Uswatte G, Morris DM: Improved motor recovery
after stroke and massive cortical reorganization following
constraint-induced movement therapy. Phys Med Rehabil
Clin N Am 2003, 14:S77S91.
52.
53.
Harvey
259
Winstein CJ, Pohl PS, Lewthwaite R: Effects of physical
guidance and knowledge of results on motor learning: support for the guidance hypothesis. Res Q Exerc Sport 1994,
65:316323.
Cirstea MC, Levin MF: Improvement of arm movement
patterns and endpoint control depends on type of feedback
during practice in stroke survivors. Neurorehabil Neural
Repair 2007, 21:398411.
You might also like
- Bilateral UL Movt TrainingDocument4 pagesBilateral UL Movt TraininggfdggNo ratings yet
- PANat - Thetrical - Air Splints - Talas Pneumaticas Margaret JohnstoneDocument44 pagesPANat - Thetrical - Air Splints - Talas Pneumaticas Margaret JohnstonePedro GouveiaNo ratings yet
- Module 10 Upper Extremity FINAL 16edDocument163 pagesModule 10 Upper Extremity FINAL 16edgialinuNo ratings yet
- Chapter 10 Upper Extremity Interventions PDFDocument208 pagesChapter 10 Upper Extremity Interventions PDFRonny Méndez VasconcellosNo ratings yet
- Rheumatology Practice in Occupational Therapy: Promoting Lifestyle ManagementFrom EverandRheumatology Practice in Occupational Therapy: Promoting Lifestyle ManagementLynne GoodacreNo ratings yet
- Occupation Analysis in PracticeFrom EverandOccupation Analysis in PracticeLynette MackenzieNo ratings yet
- Movement Difficulties in Developmental Disorders: Practical Guidelines for Assessment and ManagementFrom EverandMovement Difficulties in Developmental Disorders: Practical Guidelines for Assessment and ManagementNo ratings yet
- TyrosolutionDocument20 pagesTyrosolutioneva5ochabauerNo ratings yet
- OT 460 Intervention Kit AssignmentDocument2 pagesOT 460 Intervention Kit AssignmentMegan McCarthyNo ratings yet
- Physical Therapy Tests in Stroke RehabilitationDocument22 pagesPhysical Therapy Tests in Stroke Rehabilitationmehdi.chlif4374No ratings yet
- Motor and Proprioception Deficits in Post Rehab StrokeDocument21 pagesMotor and Proprioception Deficits in Post Rehab StrokeApril Bramhall EddyNo ratings yet
- Your Guide To Exercise After A Stroke 2017Document51 pagesYour Guide To Exercise After A Stroke 2017Georgina CorfieldNo ratings yet
- GMFM (GMFM-66 & GMFM-88) User's Manual, 2nd editionFrom EverandGMFM (GMFM-66 & GMFM-88) User's Manual, 2nd editionRating: 1 out of 5 stars1/5 (1)
- EBRSR Handbook Chapter 4 - Upper Extremity Post Stroke - MLDocument60 pagesEBRSR Handbook Chapter 4 - Upper Extremity Post Stroke - MLanjelikaNo ratings yet
- Malignant Spinal Cord Compression - Dealing The Most Common - MetsDocument60 pagesMalignant Spinal Cord Compression - Dealing The Most Common - MetsDr Sasikumar Sambasivam100% (2)
- Early Detection and Early Intervention in Developmental Motor Disorders: From Neuroscience to ParticipationFrom EverandEarly Detection and Early Intervention in Developmental Motor Disorders: From Neuroscience to ParticipationNo ratings yet
- Task-Specific TrainingDocument16 pagesTask-Specific Trainingapi-293223028No ratings yet
- Nuero RehabDocument14 pagesNuero RehabLINDSLEY GONo ratings yet
- Classification of Upper Limb OrthosesDocument16 pagesClassification of Upper Limb Orthoseszoha hassanNo ratings yet
- Scales To Assess Gross Motor Function in Stroke Patients: A Systematic ReviewDocument10 pagesScales To Assess Gross Motor Function in Stroke Patients: A Systematic ReviewAngie TarazonaNo ratings yet
- Pediatric Outcome MeasuresDocument40 pagesPediatric Outcome MeasuresMaybelle Anne ZamoraNo ratings yet
- Role of Physiotherapy in Neurological RehabilitationDocument17 pagesRole of Physiotherapy in Neurological RehabilitationMaheen AnwaarNo ratings yet
- Introduction To MovementsDocument42 pagesIntroduction To MovementsRamalingam KanagarajNo ratings yet
- Muscle Grading and Testing ProceduresDocument5 pagesMuscle Grading and Testing Proceduresshodhganga100% (1)
- Emerging Therapies in NeurorehabilitationDocument15 pagesEmerging Therapies in NeurorehabilitationAnonymous xehY8oFgYNo ratings yet
- The Effectiveness of Trunk Training On Trunk Control, Sitting and Standing Balance and Mobility Post-Stroke: A Systematic Review and Meta-AnalysisDocument11 pagesThe Effectiveness of Trunk Training On Trunk Control, Sitting and Standing Balance and Mobility Post-Stroke: A Systematic Review and Meta-AnalysisMarcela NunesNo ratings yet
- Occupational Therapy After StrokeDocument6 pagesOccupational Therapy After StrokeSheel GuptaNo ratings yet
- Mobilization and Stimulation of Neuromuscular Tissue (MaSoNT)From EverandMobilization and Stimulation of Neuromuscular Tissue (MaSoNT)No ratings yet
- Neurological Assessment in the First Two Years of LifeFrom EverandNeurological Assessment in the First Two Years of LifeGiovanni CioniNo ratings yet
- Instrumental Activities Daily Living: Try ThisDocument11 pagesInstrumental Activities Daily Living: Try ThisbalryoNo ratings yet
- JOSPT Shoulder Pain and Mobility Deficitis Adhesive Capsulitis PDFDocument33 pagesJOSPT Shoulder Pain and Mobility Deficitis Adhesive Capsulitis PDFAbdul Wahid ShaikhNo ratings yet
- Unlocking Pathways of Pain: Stories of Innovative Treatments and How They WorkFrom EverandUnlocking Pathways of Pain: Stories of Innovative Treatments and How They WorkNo ratings yet
- ApproachDocument37 pagesApproachAshu AshNo ratings yet
- A Practical Guide to the Self-Management of Lower Back Pain: A Holistic Approach to Health and FitnessFrom EverandA Practical Guide to the Self-Management of Lower Back Pain: A Holistic Approach to Health and FitnessNo ratings yet
- Sensory Re-Education: Hand Physiotherapy DepartmentDocument2 pagesSensory Re-Education: Hand Physiotherapy DepartmentEmanuel George StoenescuNo ratings yet
- Doyon 2005. Reorganization and Plasticity in The Adult Brain During Learning of Motor SkillsDocument7 pagesDoyon 2005. Reorganization and Plasticity in The Adult Brain During Learning of Motor SkillsenzoverdiNo ratings yet
- LOTCA Assessment ReviewDocument10 pagesLOTCA Assessment ReviewManik MishraNo ratings yet
- Amputee Activity Score PDFDocument5 pagesAmputee Activity Score PDFLydia MartínNo ratings yet
- Rehabilitation of Patients After StrokeDocument47 pagesRehabilitation of Patients After StrokeRogerNo ratings yet
- Exercise your way to health: Arthritis: Exercise plans to improve your lifeFrom EverandExercise your way to health: Arthritis: Exercise plans to improve your lifeNo ratings yet
- Balance Dysfunction in Parkinson’s Disease: Basic Mechanisms to Clinical ManagementFrom EverandBalance Dysfunction in Parkinson’s Disease: Basic Mechanisms to Clinical ManagementNo ratings yet
- Evaluation of The Hand!Document84 pagesEvaluation of The Hand!Ahmad A. Fannoon100% (1)
- H Clinical Assessment ToolsDocument71 pagesH Clinical Assessment ToolsPaijo SusenoNo ratings yet
- Occupational Therapy As A Major Activity of Human Being: by Rafia KhalidDocument20 pagesOccupational Therapy As A Major Activity of Human Being: by Rafia Khalidnomi9818No ratings yet
- Cardiac RehabilitationDocument114 pagesCardiac RehabilitationAfiqul RashyedNo ratings yet
- Ot Guidelines ParkinsonDocument145 pagesOt Guidelines ParkinsonFannyNo ratings yet
- Stroke Rehab, Info Proving PNF To Improve Upper Limb Function - FullDocument6 pagesStroke Rehab, Info Proving PNF To Improve Upper Limb Function - FullThomas CorbettNo ratings yet
- Orthosisofhandppt 181202162551Document65 pagesOrthosisofhandppt 181202162551Khageswar SamalNo ratings yet
- Tendon Injury and GraftingDocument66 pagesTendon Injury and GraftingVinay KarwalNo ratings yet
- The Role of Fear of Movement/ (Re) Injury in Pain DisabilityDocument18 pagesThe Role of Fear of Movement/ (Re) Injury in Pain DisabilityWilbur WhateleyNo ratings yet
- Cerebral PalsyDocument23 pagesCerebral Palsyane2sa100% (1)
- Environmental Modifications: Nakul RangaDocument42 pagesEnvironmental Modifications: Nakul Rangataniamahapatra1No ratings yet
- De Quervain SyndromeDocument5 pagesDe Quervain Syndromebangla018No ratings yet
- PD 8278 Energy Conservation PDFDocument4 pagesPD 8278 Energy Conservation PDFahmad kusnaeniNo ratings yet
- Dementia AOTA Helpful Fact SheetDocument2 pagesDementia AOTA Helpful Fact SheetMysti Reeder100% (1)
- Principles For Proper Body Mechanics: Self-Study GuideDocument8 pagesPrinciples For Proper Body Mechanics: Self-Study GuideSLCNtc100% (1)
- Pediatric Rehab 2001-2009Document221 pagesPediatric Rehab 2001-2009beekerdogNo ratings yet
- PAV y PSV PDFDocument8 pagesPAV y PSV PDFAni Fran SolarNo ratings yet
- 2014 Electromyographic Analysis of Shoulder Muscles During Press-Up Variations and ProgressionsDocument7 pages2014 Electromyographic Analysis of Shoulder Muscles During Press-Up Variations and ProgressionsAni Fran SolarNo ratings yet
- Enlightened Keyboard Technique A Definitive Model For The 21st CenturyDocument4 pagesEnlightened Keyboard Technique A Definitive Model For The 21st CenturyAni Fran SolarNo ratings yet
- PAV Interacción Paciente Ventilador PDFDocument11 pagesPAV Interacción Paciente Ventilador PDFAni Fran SolarNo ratings yet
- 2013 A Systematic Review and Meta-Analysis of Tai Chi For Osteoarthritis of The KneeDocument11 pages2013 A Systematic Review and Meta-Analysis of Tai Chi For Osteoarthritis of The KneeAni Fran SolarNo ratings yet
- 1997 Economic Analysis of Respiratory RehabilitationDocument10 pages1997 Economic Analysis of Respiratory RehabilitationAni Fran SolarNo ratings yet
- 2014 The Size and Structure of Arm Movement Variability Decreased With Work Pace in A Standardised Repetitive Precision TaskDocument13 pages2014 The Size and Structure of Arm Movement Variability Decreased With Work Pace in A Standardised Repetitive Precision TaskAni Fran SolarNo ratings yet
- Traqueostomia Paciente CriticoDocument12 pagesTraqueostomia Paciente CriticoOsman Arteaga IriarteNo ratings yet
- Paper 2Document10 pagesPaper 2KaryTapiaLizamaNo ratings yet
- 2001 A Focused Exercise Regimen Improves Clinical Measures of Balance in Patients With Peripheral NeuropathyDocument5 pages2001 A Focused Exercise Regimen Improves Clinical Measures of Balance in Patients With Peripheral NeuropathyAni Fran SolarNo ratings yet
- 2011 A Review of The Relation of Aerobic Fitness and Physical Activity To Brain Structure and Function in ChildrenDocument11 pages2011 A Review of The Relation of Aerobic Fitness and Physical Activity To Brain Structure and Function in ChildrenAni Fran SolarNo ratings yet
- 2001 Proprioceptive Training and Prevention of Anterior Cruciate Ligament Injuries in SoccerDocument6 pages2001 Proprioceptive Training and Prevention of Anterior Cruciate Ligament Injuries in SoccerAni Fran SolarNo ratings yet
- Muscle Injury in Repetitive Motion DisordersDocument11 pagesMuscle Injury in Repetitive Motion DisordersAni Fran SolarNo ratings yet
- 2014 Does Immobilization After Arthroscopic Rotator Cuff Repair Increase Tendon Healing, A Systematic Review and Meta-AnalysisDocument7 pages2014 Does Immobilization After Arthroscopic Rotator Cuff Repair Increase Tendon Healing, A Systematic Review and Meta-AnalysisAni Fran SolarNo ratings yet
- Psychobiological Model of Temperament and CharacterDocument16 pagesPsychobiological Model of Temperament and CharacterStojan Bajraktarov100% (1)
- 2014 Rehabilitation of Meniscal Injury and SurgeryDocument20 pages2014 Rehabilitation of Meniscal Injury and SurgeryAni Fran SolarNo ratings yet
- Variability in Action, Contributions of A Songbird Cortical-Basal Ganglia Circuit To Vocal Motor Learning and ControlDocument9 pagesVariability in Action, Contributions of A Songbird Cortical-Basal Ganglia Circuit To Vocal Motor Learning and ControlAni Fran SolarNo ratings yet
- Effectiveness of An Exercise Program To Improve Forward Head Posture in Normal AdultsDocument14 pagesEffectiveness of An Exercise Program To Improve Forward Head Posture in Normal AdultsAni Fran SolarNo ratings yet
- 2014 Effectiveness of Continuous Vertebral Resonant Oscillation Using The POLD Method in The Treatment of Lumbar Disc Hernia. A Randomized Controlled Pilot StudyDocument25 pages2014 Effectiveness of Continuous Vertebral Resonant Oscillation Using The POLD Method in The Treatment of Lumbar Disc Hernia. A Randomized Controlled Pilot StudyAni Fran SolarNo ratings yet
- 2001 An Economic Overview of Chronic Obstructive Pulmonary DiseaseDocument20 pages2001 An Economic Overview of Chronic Obstructive Pulmonary DiseaseAni Fran SolarNo ratings yet
- 2014 Walking Energetics, Fatigability, and Fatigue in Older Adults The Study of Energy and Aging PilotDocument8 pages2014 Walking Energetics, Fatigability, and Fatigue in Older Adults The Study of Energy and Aging PilotAni Fran SolarNo ratings yet
- 2014 Effectiveness of Continuous Vertebral Resonant Oscillation Using The POLD Method in The Treatment of Lumbar Disc Hernia. A Randomized Controlled Pilot StudyDocument25 pages2014 Effectiveness of Continuous Vertebral Resonant Oscillation Using The POLD Method in The Treatment of Lumbar Disc Hernia. A Randomized Controlled Pilot StudyAni Fran SolarNo ratings yet
- 2011 A Review of The Relation of Aerobic Fitness and Physical Activity To Brain Structure and Function in ChildrenDocument11 pages2011 A Review of The Relation of Aerobic Fitness and Physical Activity To Brain Structure and Function in ChildrenAni Fran SolarNo ratings yet
- 2014 Factors Affecting Rotator Cuff HealingDocument11 pages2014 Factors Affecting Rotator Cuff HealingAni Fran SolarNo ratings yet
- 2014 No. 5 Effects of Exercise Interventions On Pro-Inflammatory Biomarkers in Breast Cancer SurvivorsDocument1 page2014 No. 5 Effects of Exercise Interventions On Pro-Inflammatory Biomarkers in Breast Cancer SurvivorsAni Fran SolarNo ratings yet
- 2003 How We Walk, Central Control of Muscle Activity During Human WalkingDocument11 pages2003 How We Walk, Central Control of Muscle Activity During Human WalkingAni Fran SolarNo ratings yet
- Differential Activation of Parts of The Serratus Anterior Muscle During Push-UpDocument7 pagesDifferential Activation of Parts of The Serratus Anterior Muscle During Push-UpRudolfGerNo ratings yet
- 2014 Evaluating Anterior Knee PainDocument21 pages2014 Evaluating Anterior Knee PainAni Fran SolarNo ratings yet
- 2014 O1-16-6 Center-Based Exercise On Cancer-Related Fatigue in Breast Cancer Survivors During Active Treatment A Meta-AnalysisDocument1 page2014 O1-16-6 Center-Based Exercise On Cancer-Related Fatigue in Breast Cancer Survivors During Active Treatment A Meta-AnalysisAni Fran SolarNo ratings yet
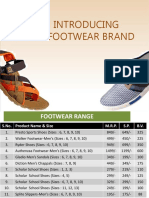
- Shoe Size Conversion Chart: (U.S. Sizes in Bold)Document1 pageShoe Size Conversion Chart: (U.S. Sizes in Bold)ThoraNo ratings yet
- Waltham Forest News 12th January 2015Document24 pagesWaltham Forest News 12th January 2015ChingfordCCNo ratings yet
- Critical Gait Parameters and Normal Human LocomotionDocument40 pagesCritical Gait Parameters and Normal Human LocomotionAastha chandankhedeNo ratings yet
- 202137-Pricing StrategyDocument4 pages202137-Pricing StrategyPriya MalhotraNo ratings yet
- Gait Asymmetry in Patients With Limb Length DiscrepancyDocument8 pagesGait Asymmetry in Patients With Limb Length DiscrepancyPhooi Yee LauNo ratings yet
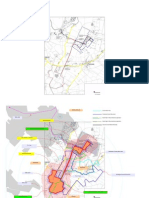
- Wichita Mtns Trail MapDocument1 pageWichita Mtns Trail Mapmattlee7No ratings yet
- Ingles para ToeflDocument51 pagesIngles para ToeflJeziel JuárezNo ratings yet
- SPEX 201 Lab 1 - Motion Analysis Techniques - STUDENT - 2023Document8 pagesSPEX 201 Lab 1 - Motion Analysis Techniques - STUDENT - 2023tom mallardNo ratings yet
- PIN Flash 38 - FINALDocument74 pagesPIN Flash 38 - FINALPUSHER69No ratings yet
- Sport ShoesDocument50 pagesSport ShoesGabriel RohNo ratings yet
- Authenza ShoeDocument84 pagesAuthenza ShoesatishNo ratings yet
- Recreation and Other Social Welfare Concerns: Lesson 27Document30 pagesRecreation and Other Social Welfare Concerns: Lesson 27Rachelle PitpitNo ratings yet
- Rec Trail Project ListDocument1 pageRec Trail Project ListBander Al–kouhlaniNo ratings yet
- Gait Analysis PresentationDocument41 pagesGait Analysis PresentationKýñg ButlerNo ratings yet
- Pacific Spirit MapDocument1 pagePacific Spirit MapEllie CoyteNo ratings yet
- Claremont Courier 1.30.13Document20 pagesClaremont Courier 1.30.13Claremont CourierNo ratings yet
- Fall Risk Assessment Form: Total Score - A Total Score of 10 or More Indicates A Resident "At Risk" For FallsDocument1 pageFall Risk Assessment Form: Total Score - A Total Score of 10 or More Indicates A Resident "At Risk" For FallswaheedmohsinNo ratings yet
- ATHLETE.X Sprint Training Program - Cycle 1 (4 Weeks)Document4 pagesATHLETE.X Sprint Training Program - Cycle 1 (4 Weeks)Corrado De Simone67% (3)
- Walkingaids 180118043224Document74 pagesWalkingaids 180118043224venkata ramakrishnaiahNo ratings yet
- Sosole Outfit 1Document2 pagesSosole Outfit 1Patty ICNo ratings yet
- Stonehenge Farm Map With ImpactDocument3 pagesStonehenge Farm Map With ImpactemmahareNo ratings yet
- Gait & Posture Volume Issue 2018 - Gluteal Tendinopathy and Hip Osteoarthritis - Different PatholDocument23 pagesGait & Posture Volume Issue 2018 - Gluteal Tendinopathy and Hip Osteoarthritis - Different PatholGiancarlo Gardella MartínezNo ratings yet
- GDT ItineraryDocument7 pagesGDT ItineraryGary MagnanNo ratings yet
- Lace Detail Ankle Boots With Track Soles - PULL&BEARDocument1 pageLace Detail Ankle Boots With Track Soles - PULL&BEARNini MatkavaNo ratings yet
- Loake 2018Document22 pagesLoake 2018martin9947No ratings yet
- Vitality Fitness Points Table High Performance PDFDocument1 pageVitality Fitness Points Table High Performance PDFpieterinpretoria391No ratings yet
- Pedestrian WalkwaysDocument87 pagesPedestrian Walkwaysaiswarya. premanNo ratings yet
- Bosaeng JayaDocument8 pagesBosaeng JayaiqbalarianNo ratings yet
- Footfall Induced Vibration On StairsDocument9 pagesFootfall Induced Vibration On Stairssam07rocksNo ratings yet