Professional Documents
Culture Documents
2 Amato - Respiratory Emergencies
Uploaded by
l10n_assOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2 Amato - Respiratory Emergencies
Uploaded by
l10n_assCopyright:
Available Formats
Advanced Pediatric Emergency
Medicine Assembly
March 11 14, 2013
Lake Buena Vista, FL
Respiratory Emergencies: Latest and
Greatest Treatments
In pediatrics the most common system that causes havoc
is the respiratory system. Is it primarily in the lungs or is
there cardiac involvement as well? What is the noise and
how do we treat it? What are the new thoughts on
respiratory management from medications to devices?
Review the national standards for asthma.
Describe how to distinguish between systems with
respiratory issues in the infant and toddler.
Discuss treatment modalities for the most common
and life threatening respiratory conditions.
3/11/2013
8:30 AM - 9:00 AM
(+)No significant financial relationships to disclose
Christopher S. Amato, MD, FACEP, FAAP
Assistant Professor, Department of Emergency
Medicine, Mount Sinai School of Medicine; Director,
Pediatric Emergency Medicine Fellowship; Medical
Director, Pediatric Advanced Life Support, Atlantic;
Attending Physician, Pediatric Emergency Medicine,
Morristown, New Jersey
SYLLABUS for:
Pediatric Respiratory Emergencies: Latest and Greatest Treatments
SPEAKER:
Christopher S. Amato, MD, FAAP, FACEP
Asst. Professor, Dept. of Emergency Medicine, Mount Sinai School of Medicine
Member, Education Committee, National ACEP Committee
Director, Pediatric Emergency Medicine Fellowship
Medical Director, Pediatric Advanced Life Support, Atlantic
Attending Physician, Pediatric Emergency Medicine
Morristown Memorial Hospital /Goryeb's Children's Hospital
Morristown, N.J. 07962
Emergency Medical Associates
COURSE DESCRIPTION:
This course will discuss, in a case-based manner, the past and most recent literature pertaining to the
pediatric patient with a respiratory emergency. I will discuss recent statistics related to respiratory illness
in the pediatric patient; review specific treatment modalities for the most common and potentially life
threatening respiratory conditions; I will discuss the literature that reviews any recent changes in the care
of these specific conditions; An in-depth discussion of asthma and the current national guidelines will be
presented; and finally, a brief discussion of tricks-of-the-trade in differentiating upper vs. lower airway
disease as well as the different approach one may take depending on the age of the affected patient.
The reason for providing the case-based approach is to involve the learner in a clinically relevant
approach to discussing the most common causes of respiratory emergencies. As respiratory illness or
obstruction is a major cause of cardiopulmonary arrest in pediatrics, it is important to review the most
common causes as well as the treatment and discuss a standardization of approach.
COURSE OBJECTIVES:
1) Review basic epidemiology as it relates to respiratory emergencies in pediatrics
2) Review a variety of common pediatric respiratory illness that can lead to arrest and their treatment with
documentation of the literature to support the treatment
3) Review the national Guidelines for the care of the asthmatic during an exacerbation
Course Outline:
1) Epidemiology of Respiratory illness/ arrest
2) Case-based discussion of Croup and the evidence based approach to treatment
3) Case-based discussion of aspiration of foreign bodies with a special discussion of the button battery
aspiration
4) Case-based discussion of Bronchiolitis and recent literature as to whom to admit
5) Case-based discussion of Asthma and review of current literature regarding
a. Use of MDI with Spacer (and even home-made spacers) vs. Neb
b. Timing of steroids
c. Ipatroprium Bromide
d. IV Magnesium Sulphate
e. Review current statistics/ epidemiology of asthma
6) Case-based discussion of Pertussis and its diagnosis in the ED
References:
Petruzella FD, Gorelick MH. Duration of Illness in infants with Bronchiolitis evaluated in the Emergency
Department. Pediatrics. 2010 Aug;126(2):285-90
Marlais M, Evans J, Abrahamson E. Clinical predictors of admission in infants with acute bronchiolitis.
Arch Dis Child. 2011; 96 (7): 648-652
Quality of Care for Common Pediatric Respiratory Illnesses in United States Emergency Departments:
Analysis of 2005 National Hospital Ambulatory Medical Care Survey Data. Pediatrics, 2008; 122: 1165
1170
Zar HJ, Brown G, Brathwaite N, et al. Home-made spacers for bronchodilator therapy in children with
acute asthma: a randomized trial. The Lancet. September 1999, 354: 979-982
Dolovich M. The Journal of Aerosol Medicine. March 1996, 9(s1): S-49-S-58
The effectiveness of glucocorticoids in treating croup: meta-analysis. BMJ 1999;319:595-600
Mackey, Wojcik, MS, Callahan, MD, Grant, EdD. Predicting Pertussis in a Pediatric Emergency
Department Population. Clinical Pediatrics, 2007; 46: 437-440
Finelli L, DrPH, Fiore A, Dhara R, et al., Influenza-Associated Pediatric Mortality in the United States:
Increase of Staphylococcus aureus Coinfection. Pediatrics 2008;122 (4):805811
2/20/2013
Advanced Pediatric Emergency Medicine
Assembly
Disneys Contemporary Resort | March 12-14, 2013
Respiratory Emergencies: The
Latest and Greatest Treatments!
Christopher S. Amato, MD, FACEP, FAAP
Morristown Medical / Goryeb Childrens Hospital
Emergency Medical Associates
Morristown, NJ
Things To Talk About
Foreign Bodies
Croup
Bronchiolitis
Asthma
Pertussis
2/20/2013
This is Why we are Here
1 Respiratory
10%
10%
Shock
80%
1 Cardiac
PediatricCardiopulmonaryArrests
The Numbers
10 % of ALL Pediatric Emergency Visits
20% of ALL Hospitalizations
1oC >37 = 3-7 breaths per minute additional
<12 months can be 7-11 breaths/min
2/20/2013
The Dangers of Math
Poiseuilles Law
R=
8nl
r4
Ifradiusishalved,resistanceincreases16fold
DiagramoftheEffectofEdemaonthe
CrossSectionalAirwayDiameter
(R=radius)
1mm = 20% loss
Adult Airway
Area = R2 = 102 = 100 mm2 (Normal)
If have 1 mm Edema Area = 92 = 81 mm2
Or 81% of normal
20 mm
1mm = 50% loss
6 mm
Full Term Newborn
Area = R2 = 32 = 9 mm2 (Normal)
If have 1 mm Edema Area = 22 = 4 mm2
Or 44% of normal
2/20/2013
Case #1
A 3 year old is sent in by his pediatrician at 2
AM after listening to him coughing by phone
The child had a URI for 2 days and then began
to cough, with progression to hoarseness and
what sounds like stridor
In the ED he is febrile (39), running around the
room, without stridor at rest
Assesment
Awake, abnormal breathing, normal circulation
Vital signs:
T 39, RR 30, P 100, PulsOx 99%
PE Mild tachypnea but no Distress
2/20/2013
InitialAssesment
Patent
Tachypnea without retractions
Color is normal, skin is warm and dry, pulse is
rapid but strong and regular.
Alert with no focal neurologic signs; GCS 15
No obvious signs of injury
What can be done diagnostically?
CXR / labs
Just say NO----the history and PE favor croup
www.andorrapediatrics.com
Quick recheck of immunization status---epiglottitis is still possible in this group
Prior stenosis due to Trisomy 21 or Subglottic
2/20/2013
What can be done therapeutically?
Mist therapy
Doesnt work!
Dont upset them!
Corticosteroids
Effective in moderate to severe croup---PO/IM superior
to nebulized
Dexamethasone (0.15 - 0.6 mg/kg) PO/IM
Racemic Epinephrine
Racemic 0.05 mL/kg (max 0.5 mL)
L-epinephrine (1:1,000 solution) 0.5 mL/kg (max 5 mL)
Observe for 2hoursrebound unlikely afterward
2 strikes and youre OUT! Admit
Cochrane Review 2011
38 studies met the inclusion criteria (4299pts)
Glucocorticoid treatment was associated with
an improvement in the croup severity score at
6 hours
Fewer returns and Length of stay
2/20/2013
Case #2
Mother of 13-month-old boy found him
choking and gagging next to container of
spilled nuts.
Paramedics noted appearance is alert; work of
breathing is increased with audible stridor;
subcostal retractions; color is normal.
UpperAirwayObstruction
ConsiderEtiologies:
Acute anaphylaxis
Choking/foreign body
Infectious
Croup
Epiglottitis
Abscess
2/20/2013
Assesment
Awake, abnormal breathing, normal circulation
Vital signs:
HR 160, RR 60, BP 88/56,
T 37.1C, O2 sat 93%, Wt 11 kg
InitialAssesment
Stridor
Tachypnea with retractions, reduced tidal
volume
Color is normal, skin is warm and dry, pulse is
rapid but strong and regular.
Alert with no focal neurologic signs; GCS 15
No obvious signs of injury
2/20/2013
ForeignBodyAspiration
A history of choking is the most reliable
predictor of FB aspiration
Specificity>90%
Sensitivity4576%
Other signs and symptoms include:
Upper airway: Stridor, respiratory or
cardiopulmonary arrest
Lower airway: Coughing, wheezing,
retractions, decreased breath sounds,
cyanosis
Background:
150300fatalitiesinyoungchildreneachyear
Foreverydeath=100chokingrelatedeventsseen
inanE.D
2/3ofcasesareinchildren12yo
2/20/2013
Often occurs in children
<5 years
Common offending
agents: foods and
home items
Balloons are the most
common FB to result in
death
Pediatricians Propose Hot Dog
Redesign aka SafetyDog
Feb 22, 2010 11:30 AM
"Ifyouweretofindthebestengineersintheworld
andaskthemtodesigntheperfectplugforachild's
airway,youcouldn'tdomuchbetterthanthehotdog
Popcorn,nuts,grapes,seedsandrawcarrotsas"high
riskfoods."
Hotdog
~17percentoffoodrelatedasphyxiations
~10,000children<14toEDforchoking
Upto77youngpeopledie
10
2/20/2013
Chest X-ray: Normal in 20-40%
FB often Radiolucent
Inspiratory / Expiratory
vs. Decubitus
Lower Airway Obstruction
HeliOx can be tried
ButtonBattery
TrueEmergency
LeakageofContents
PressureNecrosis
MucosalBurnfromElectrolyteReaction
11
2/20/2013
Case #3
Mother of 2-month-old boy with 3days of a
URI now with increasing work of breathing.
EMS called
En route patient remained alert and they note a
waterfall of snot from his nose
LowerAirwayObstruction
ConsiderEtiologies:
Asthma
Pulmonary Edema
Infectious
Pneumonia
Bronchiolitis
12
2/20/2013
Assesment
Awake, abnormal breathing, normal circulation
Vital signs:
HR 160, RR 60, BP: hahahaha
T 38.4C, O2 sat 93%, Wt 5 kg
InitialAssesment
Patent
Tachypnea with paradoxical breathing,
scattered wheeze
Color is normal, skin is warm and dry, pulse is
rapid but strong and regular.
Alert with no focal neurologic signs; GCS 15
No obvious signs of injury
13
2/20/2013
Bronchiolitis
AffectsChildren<2yo
Viral, often RSV (may be metapneumovirus)
Differentiate upper vs. Lower in <5second
Other signs and symptoms include:
Upper airway: Stridor, respiratory or
cardiopulmonary arrest
Lower airway: Coughing, wheezing,
retractions, decreased breath sounds,
cyanosis
Bronchiolitis
RSV NP may be necessary for bed placement
NO need for CXR
72% of bronchiolitis visits had CXR done!
Who do I admit?
Clinicalpredictorsofadmissionininfantswith
acutebronchiolitis,ArchDisChild2011
14
2/20/2013
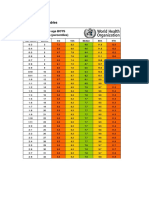
Clinicalpredictorsofadmissionininfants
Points
withacute DurationofSxs <5days
1
bronchiolitis
0
>5days
Respiratoryrate
Heart Rate
O2 Sat.
>50Breath/min
<50Breath/min
>155BPM
<155BPM
<97%
>97%
Ageatpresentation <18weeks
>18weeks
Total
Optimal cut off score >3 for admit
Sensitivity 74%, Specificity 77%
PPV 67%, NPV 83%
Case #4
A 6 year old presents with a 3 day history of
cough, worse with activity
No one smokes inside the house.
Strong family history of asthma
15
2/20/2013
Assesment
Awake, abnormal breathing, normal circulation
Vital signs:
T 37.2, RR 26, P 90, PulsOx 94%, Wt 25 kg
PE Mild tachypnea but no Distress
InitialAssesment
Patent
Tachypnea without retractions, No wheezing
heard, ? Prolonged expiratory phase
Color is normal, skin is warm and dry, pulse is
rapid but strong and regular.
Alert with no focal neurologic signs; GCS 15
No obvious signs of injury
16
2/20/2013
What can be done diagnostically?
CXR
in RAD will show hyperinflation AND rule out
odd etiologies in first time wheezers
Hyperinflation and Flattened Diaphragms
What can be done diagnostically?
Trial of a bronchodilator
DEFINITELY indicated since the first symptom of RAD
is cough, not wheezing
in older kids, Peak Flow measurements pre and post
aerosols will often seal the deal
many of these chronic cough kids get labeled as
bronchitis, not really a pediatric disease, and end up
on antibiotics
Cephakillit all vs. Z-pack vs. Dancing funky chicken
17
2/20/2013
What can be done therapeutically?
Albuterol and Atrovent
Indicated, often X3
Use spacers
Steroids
give them EARLY, often for 3-5 days, may use
Dexmethasone
Oral as effective as IV
Spacers vs. Nebulizers
Analyzed 1,076 children and 444 adults included in
22 trials from emergency department (ED) and
community settings
In addition, 5 trials on inpatients with acute asthma
(184 children and 28 adults)
Method of delivery of 2-agonist did not appear to
affect hospital admission rates
CochraneReview,2009,CatesCJ
18
2/20/2013
Spacers vs. Nebulizers
No difference in admission rate
95% CI ( OR: 0.4 to 2.1 )
Childrens LOS in the ED shorter
mean diff: -0.62 hours
95% CI ( -0.84 to -0.40 )
No difference for LOS in adults
Decreased Pulse & tremor in spacer group
Each spray = 108 microgram
Spacers vs. Nebulizers
19
2/20/2013
Nebulizers versus inhalers
Conclude
MDI + holding chambers produced outcomes that
were at least equivalent to nebulizer delivery
Holding chambers may have some advantages
compared with nebulizers for children with acute
asthma
FYI
MDI comes out at 60MPH
Spacer decreased med deposition to pharynx by 50%
National Asthma Education and
Prevention Program: Expert Panel 3
Assess severity
physical examination, and signs and symptoms
by lung function measures (for ages 5 years and up)
History
Risk factors for severity: most recent ED visits or
admissions, prior intubation or PICU admission,
rapidly progressive episodes, how often theyve used
steroids and MDI
20
2/20/2013
National Asthma Education and
Prevention Program: Expert Panel 3
Treat to relieve hypoxemia and airflow obstruction; reduce
airway inflammation.
Use supplemental oxygen as appropriate to correct hypoxemia.
Treat with repetitive or continuous SABA (shortacting beta2
agonist), w/ inhaled ipratropium bromide in severe
exacerbations.
Give oral systemic corticosteroids in moderate or severe
exacerbations or for patients who fail to respond promptly and
completely to SABA.
Consider adjunctive treatments, such as intravenous
magnesium sulfate or heliox, in severe exacerbations
unresponsive to treatment.
Monitor response with repeat assessment of lung function
measures, PE, and signs and sxs, and, in ED, pulse oximetry.
National Asthma Education and
Prevention Program: Expert Panel 3
Discharge with medication and patient
education:
Medications: SABA, oral systemic corticosteroids;
consider starting ICS (inhaled corticosteroids)
Referral to followup care
Asthma discharge plan
Review of inhaler technique and, whenever possible,
environmental control measures
21
2/20/2013
Therapy
Spacer versus Nebulizer
Timing of Steroids
Ipratropium bromide
Magnesium SO4
Steroids
Cochrane Review: May 2001
12 Studies:
863 Patients
409 Pediatric
Main outcome: need for admission
22
2/20/2013
Steroids
Steroids
Number needed to treat with steroids
in the first hour to prevent 1
admission:
6
23
2/20/2013
Canadian Asthma Consensus Group:
Level 1 Evidence
For patients in ED or admitted
IV steroid therapy has NO advantage over oral therapy in
terms of rate of resolution of airflow limitation
Dexmethasone 0.6mg/kg (16mg max) in lieu of 5d
Prednisolone
Single dose therapy for mild to moderate asthma (18mg
max)
IM vs Oral
Therapy
Spacer versus Nebulizer
Timing of Steroids
Ipratropium bromide
Magnesium SO4
24
2/20/2013
Ipratropium bromide
Single dose does not work
Multiple dose decreases admissions
NNT 12 overall
95% CI ( 8, 32 )
NNT 7 severe subgroup 95% CI ( 5,20 )
Ipratropium - Admissions
25
2/20/2013
Effectofnebulizedipratropiumonhospitalizationratesof
childrenwithasthma
Qureshi etal,NEJM,Oct1998
Results
Lower rate of hospitalization in treatment
group
asthma score improved especially in Severe
No significant difference in moderate
Significant reduction in severe group
PEFR <50%, asthma score 12-15
NNT(# needed to treat) with severe asthma to
prevent 1 admission=6.6
Therapy
Spacer versus Nebulizer
Timing of Steroids
Ipratropium bromide
Magnesium SO4
26
2/20/2013
MgSO4
Mechanism of Action
translocation of Ca across cell membrane, leads to SM
relaxation & bronchodilation
Inhibits degranulation of mast cells
Decreases release of ACH ( excitability of muscle fiber
membranes)
Side Effects:
Facial warmth/flushing, hypotension, nausea, emesis,
muscle weakness, sedation, loss of DTRs, resp
depression
Dose:
20-100mg/kg (2g max) IV over 20-30 min
IV and nebulized MgSo4 for treating
acute asthma in adults and children: A
systematic review and Meta analysis:
25 Trials (16 IV, 9 Nebulized)
1754 patients
IV MgSO4 (in addition to 2-agonist & Steroids)
Improved pulmonary function and Admission for Children
Only improved lung function in adults
Shan Z, Rong Y Respir Med. 2013
27
2/20/2013
Magnesium - Admissions
Magnesium - Harm?
28
2/20/2013
IV MgSO4 Cochrane 2009
7 trials (5 adult, 2 Peds) = 665 pts.
Current evidence does not support routine use
of IV MgSo4 in ALL patients with acute
asthma presenting to ED.
MgSO4 appears to be safe and beneficial in
patients who present with SEVERE acute
asthma.
Asthma Statistics
18.9 million Americans have asthma (7.2million
children)
3400 deaths annually
479,000 hospital discharges with asthma as
primary diagnosis
African Americans hospitalized 3x more than other
americans
AA and Hispanic in inner cities are 2-6x more likely
to die from asthma
29
2/20/2013
Asthma Stats (contd)
10,000,000 school absences per year
3,000,000 PMD visits anually
Age of onset:
30% by 1 year old
80-90% by 4-5 years old
CONCLUSIONS
Current therapy in children is based on
variable levels of evidence
Level 1 evidence to support steroids, Atrovent,
MgSO4
Level 2 evidence for HELIOX
Level 3-5 evidence for ketamine, NO,
aminophylline, anesthetic agents
30
2/20/2013
Case #5
A 6mo presents with cough for 7 days
What began as a URI has progressed to bursts
of coughing followed by post-tussive emesis
Non-stop cough
No significant PMH, immunized for age
Assesment
Awake, normal breathing, normal circulation
Vital signs:
T 37, RR 20, P 76, PulsOx 99%
Subconjunctival hemorrhages and facial
petechiae
Intermittent staccato cough
31
2/20/2013
InitialAssesment
Patent
No wheezing heard, CTA
Color is normal, skin is warm and dry, pulse is
rapid but strong and regular.
Alert with no focal neurologic signs; GCS 15
No obvious signs of injury
Approximately42,000casesofwhooping
coughwerereportedlastyear.
Thelargestoubreak ofpertussissince1955
Predicting Pertussis in a Pediatric Emergency
Department Population
Mackey, Wojcik, MS, Callahan,
MD, Grant, EdD Clinical Pediatrics
46: 437-440 2007
32
2/20/2013
Summary
Quick recognition of the illness allows rapid triage,
isolation, and prevention of nosocomial transmission
Infants younger than 2 months who have a cough or
choking associated with cyanosis
as well as a cough and rhonchi on physical examination,
have a high likelihood of pertussis and should be identified
in triage, isolated immediately, and tested for pertussis
This may lead to appropriate therapy for this population
and decrease the transmission of pertussis to other
patients and staff in the ED
What can be done diagnostically?
CXR
probably not helpful, but may rule out foreign
body
Bronchodilator?
NO, this is not a lower airway disease
CBC
WBC may show leukocytosis and lymphocytosis
(pertussis)
Pertussis swab
33
2/20/2013
What can be done therapeutically?
Avoid any form of oral stimulation
Provide supplemental oxygen
Admission?
Treat the child and household contacts with a
Macrolide
Make sure youve received a pertussis
immunization
In Summary
History of Choking is the most reliable
predictor of Aspirated Foreign Body
Standardized approaches to asthma will
improve outcomes
Steroids have an EARLY role in both croup
and RAD
Pertussis surveillance is mandatory
34
2/20/2013
QUESTIONS???
Dani theasthmaticMuppet
35
You might also like
- Beverly J. McCabe, Eric H. Frankel, Jonathan J. Wolfe Handbook of Food-Drug InteractionsDocument1 pageBeverly J. McCabe, Eric H. Frankel, Jonathan J. Wolfe Handbook of Food-Drug Interactionsl10n_assNo ratings yet
- Classification of Cutaneous LupusDocument5 pagesClassification of Cutaneous Lupusl10n_assNo ratings yet
- NPPA040112 DecisiontreeDocument1 pageNPPA040112 Decisiontreel10n_assNo ratings yet
- TABLE Boys 3mo To 5yr TRICEPSage PercentileDocument2 pagesTABLE Boys 3mo To 5yr TRICEPSage Percentilel10n_assNo ratings yet
- Boeck Ler 2009Document5 pagesBoeck Ler 2009l10n_assNo ratings yet
- Bmi For Age Z-ScoreDocument1 pageBmi For Age Z-ScoreTisha Patricia OedoyNo ratings yet
- Wozniacka2005 Optimal Use of Antimalarials in TreatingDocument11 pagesWozniacka2005 Optimal Use of Antimalarials in Treatingl10n_assNo ratings yet
- Callen2009 Clinically Relevant InformationDocument4 pagesCallen2009 Clinically Relevant Informationl10n_assNo ratings yet
- Callen2004 Update On The Management of Cutaneous Lupus ErythematosusDocument6 pagesCallen2004 Update On The Management of Cutaneous Lupus Erythematosusl10n_assNo ratings yet
- Jurnal Kriteria Baru SleDocument10 pagesJurnal Kriteria Baru SleDr Edi HidayatNo ratings yet
- Weight gain by birth weight and age groups for boysDocument1 pageWeight gain by birth weight and age groups for boysl10n_assNo ratings yet
- F E T C: Luid AND Lectrolyte Herapy IN HildrenDocument12 pagesF E T C: Luid AND Lectrolyte Herapy IN HildrenHartantoRezaGazaliNo ratings yet
- Bmifa Boys Z 5 19 LabelsDocument1 pageBmifa Boys Z 5 19 LabelssufigueiraNo ratings yet
- Z Score BMI 5-19yearsold Label GirlDocument1 pageZ Score BMI 5-19yearsold Label GirlVienny Widhyanti RosaryaNo ratings yet
- Vital Signs Reference Chart - 1Document1 pageVital Signs Reference Chart - 1l10n_assNo ratings yet
- CHT Acfa Boys Z 3 5Document1 pageCHT Acfa Boys Z 3 5Rivadin NurwanNo ratings yet
- Temperature MeasurementDocument5 pagesTemperature Measurementl10n_ass100% (1)
- BMI Chart for Boys Ages 5-19Document1 pageBMI Chart for Boys Ages 5-19Justitia LantuNo ratings yet
- CSFDocument1 pageCSFl10n_assNo ratings yet
- PDFDocument1 pagePDFl10n_assNo ratings yet
- CSFDocument1 pageCSFl10n_assNo ratings yet
- Lubchenco Curve PDFDocument1 pageLubchenco Curve PDFWarren Lie25% (4)
- Cross2013 New Research With Diets and EpilepsyDocument6 pagesCross2013 New Research With Diets and Epilepsyl10n_assNo ratings yet
- GCS PDFDocument1 pageGCS PDFFrincia100% (1)
- Dahlin2005 The Ketogenic Diet Influences The Levels of Excitatory and Inhibitory Amino Acids in The CSF in Children With Refractory EpilepsyDocument11 pagesDahlin2005 The Ketogenic Diet Influences The Levels of Excitatory and Inhibitory Amino Acids in The CSF in Children With Refractory Epilepsyl10n_assNo ratings yet
- Best2000 Cardiac Complications in Pediatric Patients On The Ketogenic DietDocument3 pagesBest2000 Cardiac Complications in Pediatric Patients On The Ketogenic Dietl10n_assNo ratings yet
- PDFDocument1 pagePDFl10n_assNo ratings yet
- Cunnane2002 Potential Role of Polyunsaturates in Seizure Protection Achieved With The Ketogenic DietDocument5 pagesCunnane2002 Potential Role of Polyunsaturates in Seizure Protection Achieved With The Ketogenic Dietl10n_assNo ratings yet
- Brodie2005 Diagnosing and Predicting Refractory EpilepsyDocument4 pagesBrodie2005 Diagnosing and Predicting Refractory Epilepsyl10n_assNo ratings yet
- Bough2007 Anticonvulsant Mechanisms of The Ketogenic DietDocument16 pagesBough2007 Anticonvulsant Mechanisms of The Ketogenic Dietl10n_assNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- CCT in Anaesthetics - Assessment Blueprint Aug 2010 V1.3Document14 pagesCCT in Anaesthetics - Assessment Blueprint Aug 2010 V1.3sherif11110% (1)
- Ringerfundin e 03 07Document14 pagesRingerfundin e 03 07Annisa KhairunnisaNo ratings yet
- Staining Abnormalities of Dermal Collagen in Eosinophil - or Neutrophil-Rich Inflammatory Dermatoses of Horses and Cats As DemonstrateDocument6 pagesStaining Abnormalities of Dermal Collagen in Eosinophil - or Neutrophil-Rich Inflammatory Dermatoses of Horses and Cats As DemonstratejenNo ratings yet
- 625-Naskah Artikel-1439-1-10-20190107Document11 pages625-Naskah Artikel-1439-1-10-20190107Dhany Nufikha LanasariNo ratings yet
- DR - VM.Thomas - Consultant EmbryologistDocument2 pagesDR - VM.Thomas - Consultant EmbryologistdrthomasfertilitycenterNo ratings yet
- LacerationsDocument2 pagesLacerationsGoldyNo ratings yet
- A Singing Flutist BreathDocument2 pagesA Singing Flutist BreathBrittanyTrotterNo ratings yet
- Nicole Ryan ThesisDocument7 pagesNicole Ryan ThesisEnglishPaperHelpSaintPaul100% (1)
- Understanding Autism, OCD, and Their TreatmentsDocument8 pagesUnderstanding Autism, OCD, and Their TreatmentsTaha MohamedNo ratings yet
- IlizarovDocument2 pagesIlizarovsunshinehospitalNo ratings yet
- Nurse Education in Practice: Book ReviewsDocument1 pageNurse Education in Practice: Book ReviewsUswatun HasanahNo ratings yet
- HaloperidolDocument1 pageHaloperidolSalma AKNo ratings yet
- Guidelines For Surgery in The HIV Patient: Samuel Smit, MB CHB, M Med (Surg)Document8 pagesGuidelines For Surgery in The HIV Patient: Samuel Smit, MB CHB, M Med (Surg)Afkar30No ratings yet
- The Diagnosis of Appendicitis in Children: Outcomes of A Strategy Based On Pediatric Surgical EvaluationDocument8 pagesThe Diagnosis of Appendicitis in Children: Outcomes of A Strategy Based On Pediatric Surgical EvaluationAndikaNo ratings yet
- 1 1000 MCQ Bank of Previous Years AdcDocument6 pages1 1000 MCQ Bank of Previous Years Adcdrravimds50% (2)
- Cerebralangiography Jesppt 1Document17 pagesCerebralangiography Jesppt 1iqbalNo ratings yet
- Pediatric Physiology 2007Document378 pagesPediatric Physiology 2007Andres Jeria Diaz100% (1)
- Brosur EnglishDocument2 pagesBrosur EnglishSumiari LuhNo ratings yet
- OCR BasicOphthalmology4MedicalStudents&PrimaryCareResidents8ed2004BradfordDocument244 pagesOCR BasicOphthalmology4MedicalStudents&PrimaryCareResidents8ed2004Bradfordハルァン ファ烏山No ratings yet
- Emily J. Mathios: EducationDocument2 pagesEmily J. Mathios: Educationapi-427066976No ratings yet
- Etiology of Asthma PDFDocument2 pagesEtiology of Asthma PDFTiffanyNo ratings yet
- Blindness in Indonesia: Farida SirlanDocument41 pagesBlindness in Indonesia: Farida SirlannonawitaNo ratings yet
- Presentasi SoyaDocument29 pagesPresentasi SoyaAyla AzuraNo ratings yet
- Colorectal Cancer Screening: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document49 pagesColorectal Cancer Screening: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)StangPongritNo ratings yet
- Management of The Hydrocephalus and OutcomeDocument24 pagesManagement of The Hydrocephalus and Outcomerajan kumar100% (1)
- Bhabha ReprtDocument126 pagesBhabha ReprtRinky MansukhaniNo ratings yet
- Epistatus Administer DerbyPCT PDFDocument2 pagesEpistatus Administer DerbyPCT PDFAlex GeorgeNo ratings yet
- Essential Newborn Resuscitation StepsDocument27 pagesEssential Newborn Resuscitation StepsAnusha Verghese100% (1)
- List of Empanelled HospitalsDocument17 pagesList of Empanelled Hospitalsfathima555100% (1)
- Instructions for Ministry of Health Officials on Statement of Need LettersDocument1 pageInstructions for Ministry of Health Officials on Statement of Need LetterssurenvishvaNo ratings yet