Professional Documents
Culture Documents
9
Uploaded by
rahmawati aliwarmanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
9
Uploaded by
rahmawati aliwarmanCopyright:
Available Formats
Int J Clin Exp Med 2015;8(7):11342-11346
www.ijcem.com /ISSN:1940-5901/IJCEM0010203
Original Article
Comparison between photodynamic therapy
with topical application of 5-aminolevulinic acid
and CO2 laser therapy in the treatment of cervical
condylomata acuminate: a randomized controlled trial
Juan Du*, Xiao-Nian Lu*, Fei Li, Duo-Qin Wang, Ming Xu, Ying Sun, Jun Liang, Hui Tang, Yong-Sheng Yang,
Zhen Zhang, Xiao-Hua Zhu, Jin-Ran Lin, Jin-Hua Xu
Department of Dermatology, Huashan Hospital, Fudan University, Shanghai 200040, China. *Equal contributors.
Received May 14, 2015; Accepted July 3, 2015; Epub July 15, 2015; Published July 30, 2015
Abstract: The present study aimed to evaluate the efficacy of photodynamic therapy with topical applied 5-aminolevulinic acid (ALA-PDT) for the treatment of cervical condylomata accuminate (CA). 161 Patients with cervical
CA were randomly divided into ALA-PDT group and CO2 laser (control) group. Patients (n=89) in the ALA-PDT group
were treated with topical 5% ALA under occlusive dressing for 3 h followed by irradiation with semiconductor laser
at a dose of 1000 J/cm-2 and a power of 100 mW. Patients were treated 2 weeks later if necessary. Patients (n=72)
in the control group were treated with CO2 laser. The treatment was repeated at 1-week interval when necessary.
No response rate, complete response rate (CR) and recurrence rate of wart lesions as well as rate of eradication
of HPVs were analyzed. The CR rate was 90.2% in the ALA-PDT group and 96.2% in the control group. The eradication rate was 90.2% in the ALA-PDT group and 65.8% in the control group after 3 months of follow-up. Both the
eradication rate and recurrence rate in the ALA-PDT group were significantly lower than those in the control group
(P<0.001). The adverse event in patients receiving ALA-PDT was mainly mild bleeding. ALA-PDT is a more effective
and well-tolerated treatment for cervical CA compared with conventional CO2 laser therapy.
Keywords: 5-aminolaevulinic acid, cervical condylomata acuminate, photodynamic therapy
Introduction
Cervical condylomata acuminate (CA) are the
most common sexually transmitted disease,
which is caused by human papilloma virus
(HPV) infection. Clinical evidence suggests that
most sexually active adults will contract an HPV
infection at least once in their life time [1].
Approximately 40 types of HPVs infect the anogenital region and those with oncogenic potential are classified as high-risk HPVs [1]. Some of
them lead to not only genital warts but also lowgrade squamous intraepithelial lesions (SILs),
high-grades SILs and cervical cancer.
The ideal endpoint of treatment for cervical CA
is to make lesions clear and never recur.
However, conventional therapy could not eradicate HPV infection. For instance, the clearance
rate of surgical excision is 72%, whereas the
recurrence rate is 19~29%. Electric cauterization carries an excellent clearance of 94%, but
with a recurrence of 22%. Although widely used,
CO2 laser therapy is reported to have a clearance rate of 23~52% and a recurrence rate of
60~77% [2]. There are also kinds of side effects
caused by the above therapies such as cervical
incompetence and cervical canal stenosis.
Thus attending physicians will consider all pros
and cons associated with each therapeutic
modality, including cost, convenience and compliance.
Fortunately, 5-aminolaevulinic acid (ALA)-mediated photodynamic therapy (PDT), a new and
exciting therapeutic strategy has occurred and
become widely used during the last decade.
ALA is a precursor of the tissue photosensitizer
protoporphyrin IX (PPIX) in the heme biosynthesis pathway [6]. The presence of an excess of
ALA-PDT for the treatment of cervical CA
exogenous ALA could bypass the feedback control and lead to increased accumulation of PPIX
in mitochondria. Interestingly this occurred only
in certain types of cells [4-6]. Animal experiments showed that the epidermal cells, pilosebaceous units, urothelium and endometrium of
a mouse developed marked accumulation of
PPIX and became photosensitive with systemic
administration of ALA, whereas the dermis,
blood vessels, cartilage of the ear and myometrium did not [5]. Clinical trials revealed that
hyper-proliferative cells such as skin cancer
lesions and infected cells with specific virus
became photosensitized following local application of a solution of ALA, but normal tissue
did not [5, 6]. Such tissue specificity made it
get over the prolonged skin photosensitivity
defect of standard forms of photodynamic therapy and became widely used.
ALA-PDT has been considered as an effective
means for the treatment of CA due to lower
recurrence rate and less complications [7-10].
In the past 5 years, many patients with cervical
CA have been treated with ALA-PDT and shown
very good results especially those with multiple
lesions and latent infection [11-13]. However,
there is a lack of controlled clinical studies to
evaluate efficacy and tolerability of this therapy. In this study, we compared the topical application of ALA-PDT with CO2 laser therapy to
evaluate the efficacy of ALA-PDT.
Methods and materials
Study design
This was a randomized controlled trial that was
performed during February 2008 to March
2014 at the Department of Dermatology in
Huashan Hospital. Patients with a pathologic
diagnosis of cervical CA were eligible for inclusion. All patients provided informed consents.
This study was approved by the Ethical committee of Huashan Hospital and was conducted in
accordance with Declaration of Helsinki.
Patients
Totally 161 patients recruited from the outpatient Department of Dermatology in Huashan
Hospital with newly diagnosed cervical CA were
enrolled in this study. The diagnosis was confirmed by colposcopy, histological examination
and polymerase chain reaction. All patients
11343
had no systematic or topical treatment before
this study.
Patients with the following conditions were
excluded from the study: cutaneous sensitization, porphyria, immune deficiency or other severe systematic disease, congenital or acquired
coagulation disorders, pregnancy or lactation.
After treatment, patients were asked to abstain
from tub bathing and sexual intercourse.
ALA-PDT therapy
All patients were randomly allocated into the
ALA-PDT group and the control group. Patients
in the ALA-PDT group (n=89) were asked to lie
still in the lithotomy position. The vagina and
cervix were cleaned with an aqueous 0.4%
chlorhexidine solution. ALA powder (Zhangjiang
Bio-Pharm Co. Ltd, Shanghai, China) was dissolved in sterile saline to make a 5% ALAsolution (w/v) immediately before use. A thin
cotton swab was soaked in the ALA-solution
and applied to the cervical mucosa to be in contact with and cover the warts and the adjacent
normal skin (5-mm border). Then cling film was
used to cover the cervix, and thick gauze was
packed in the canal for light protection. After 3
hours of incubation, ALA was completely
removed with sterile saline, and the lesions and
adjacent normal skin (5-mm border) was
exposed to a cylindrical laser fiber emitting a
635 nm semiconductor laser (KDL-300, Beijing
Kedian Microwave Electronic Co. Ltd, Beijing,
China) at a fluency of 1000 J/cm2 at 100 mw.
Patients were treated two times at two-week
intervals if necessary. Colposcopy was performed after treatment once a month and biopsy and HPV test were given 2 and 6 months
after PDT.
CO2 laser therapy
For patients in the control group, lidocaine ointment was applied to the lesions after routine
sterilization for topical anesthesia. After the
lidocaine was removed with sterile saline, CO2
laser was given to vaporize the lesions and
their adjacent normal skin (5 mm border). A
repeat treatment was given at one-week interval where the lesions were not completely
removed, but no more than three times totally
was given. The follow-up was performed for the
above groups.
Int J Clin Exp Med 2015;8(7):11342-11346
ALA-PDT for the treatment of cervical CA
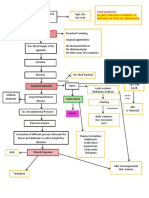
Figure 1. Cervical condylomata acuminate detected by colposcopy (lodine staining). Clinical appearance (A) before,
(B) 2 months after and (C) 6 months after photodynamic therapy using 5-aminolaevulinic acid.
Table 1. Comparison of efficacy in the two treatments
Group
NR (95% CI)
CR (95% CI)
HPV CR (95% CI)
RR (95% CI)
ALA-PDT 7.3% (1.70%-12.93%) 90.20% (83.76%-96.64%) 90.20% (83.76%-96.64%) 4.90% (0.23%-9.57%)
Control
0
96.2% (91.98%-100.0%) 65.80% (55.34%-76.26%) 19.00% (10.35%-27.65%)
NR: no response rate; CR: complete response rate; HPV CR: eradication rate of HPV infection; RR: recurrence rate.
Table 2. Adverse events in the two therapies
Group
Bleeding
Infection Cervical scaring
ALA-PDT 2 (2.44%)
0
0
Control 20 (25.32%) 5 (6.33%) 24 (30.38%)
Assessment of clinical efficacy
The indicators of efficacy were the clearance
rate of wart lesions including complete remission rate (CR), partial remission rate (PR) and
no response rate (NR), in addition to the clearance rate of HPV (HPV CR) which defined as no
HPV infection was found until the endpoint of
follow-up after treatment, as well as the recurrence rate (RR) and the incidence of adverse
event. Treatment outcomes were classified as:
CR: cervical lesions were completely cleared
and the mucosa returned to normal looking;
PR: lesion size reduced by 50% or more; NR:
less than 50% reduction in lesion size [12].
Biopsy examination and genotyping analysis
were performed for all patients at two month
and six month after treatment respectively. An
appearance of wart lesion after complete
remission was defined as recurrence and was
fixed by monthly colposcopy examination. Adverse events were asked to report at each follow-up during the study.
11344
Statistical analysis
Analysis of all data was performed by SPSS
19.0 software. Comparison of mean was used
to analysis the baseline characteristics between the two groups. Rank-sum test was used
to evaluate the general efficacy of two treatments. The CR, NR, HPV CR and RR were analyzed with chi-square test. P<0.05 was considered to be significant in all statistical analyses.
Results
Demographical data of the patients
The age range of patients enrolled in this study
was 18 to 64 years with an average of 30.29.0.
The number of wart lesions ranged from 1 to 4
with an average of 1.72. All 161 participants
were randomized divided into two groups. 89
patients were allocated into the ALA-PDT group
and 72 patients into the CO2 laser (control)
group. 146 of them completed the whole treatment and 6 months of follow-up, and 7 patients
who did not finish 3 times of treatments were
considered as no response to corresponding
treatment. For the other 8 patients dropped out
of the follow-up, data from their last visit were
included in the analysis. Baseline characteristics including age, number of lesions, size of
lesions and disease duration made no difference between groups.
Int J Clin Exp Med 2015;8(7):11342-11346
ALA-PDT for the treatment of cervical CA
Comparison of distribution of efficacy to lesions
Mann-Whitney U test was used to analyze the
general distribution of efficacy to lesions between groups. The test statistic Z=-1.6, P=0.13,
indicated no significant difference between
groups (=0.05).
Comparison of efficacy to wart lesions
We attempted to treat cervical CA with lower
concentration of ALA and achieved satisfactory
results (Figure 1).
For CR, there was no statistical difference
between ALA-PDT and control group (P=0.13),
whereas NR rate showed statistical difference
(P=0.42) (Table 1). The x2 was 4.1 and 2.2 for
NR and CR, respectively.
Comparison of HPV eradication
The eradication of HPVs infection was defined
as the negative result of biopsy examination
and HPV DNA test at the end of the treatments
and at 6 months during follow-up. The analysis
of HPV CR rate of both groups showed marked
statistical difference (x2=14.1, P<0.001) (Table
1). In addition, the RR also showed significant
statistical different (x2=7.7, P=0.006).
Adverse events
In all patients with ALA-PDT treatment, only 2
underwent mild bleeding, no infection or cervical scaring occurred. But in the control group,
20 patients had bleeding during treatment. 5
patients got infection and 24 had cervical scaring (Table 2).
Discussion
In the present study, we found that after ALAPDT therapy, both the CR rate and the HIV eradication rate were 90.2% in the ALA-PDT group.
In addition, the eradication rate and recurrence
rate in the ALA-PDT group were significantly
lower than those in the control group. Although
our study showed that ALA-PDT achieved CR
rate to CO2 laser vaporization, the latter causing a higher frequency of side effects.
The action mechanism of ALA-PDT was to excite
the accumulated PPIX which was increased by
local ALA using specific light. The singlet oxygen
11345
and other free radicals from this course lead to
necrosis and apoptosis of cells [4]. The maximum absorption band of porphyrins is in the
blue light spectrum (405-415 nm). The weaker
absorption bands are located in the green
(506-540 nm), yellow (572-582 nm), and red
spectra (628-635 nm) [16]. The 635 nm red
light is clinically used due to both absorption
rate and penetration depth.
There is a need for optimization of ALA concentrations and incubation time. The most widely
used modality is 20% of ALA solution and 3
hours incubation [11-13], which is basically
derived from the past reports and treatment of
skin diseases [14]. However, cervical tissue is
different with skin, which is lower in keratinization and stronger in penetration. In addition,
previous research indicated that 5% to 10%
ALA made optimal condition for the photodynamic therapy of urethral CA [15]. Since ALA
was expensive to most people, we attempted to
treat cervical CA with lower concentration of
ALA and achieved satisfactory results.
CO2 laser treatment was considered to be the
best method to remove lesions. However, in our
study, we found that the clearance rate in ALAPDT group and NR rate were not different from
CO2 laser group. This result indicated that low
concentration ALA-PDT can effectively eliminate CA.
In CA treatment, another important problem is
recurrence rate. Based on our results, the
recurrence rate in ALA-PDT group is much less
than that in control group. There are only 2
patients in ALA-PDT group had slight bleeding.
Moreover, there is no report on infection, cervical scar and menstrual disorder during the
follow-up.
In general, ALA PDT therapy has significant
advantages in HPV elimination and almost has
no side effects. We concluded that, topical ALAPDT, which is associated with a pretty lower RR
and less adverse events versus CO2 laser therapy, is an effective, minimally invasive, and
well-tolerated treatment for cervical CA, especially for patients with multiple lesions.
Disclosure of conflict of interest
None.
Int J Clin Exp Med 2015;8(7):11342-11346
ALA-PDT for the treatment of cervical CA
Address correspondence to: Jinhua Xu, Department of Dermatology, Huashan Hospital, Fudan
University, 2 Middle Wulumuqi Road, Shanghai
200040, China. Tel: 86-21-52887776; Fax: 86-2152887776; E-mail: xujinhua_hs@126.com
[9]
[10]
References
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
Bhatia N, Lynde C, Vender R, Bourcier M.
Understanding genital warts: epidemiology,
pathogenesis, and burden of disease of human papillomavirus. J Cutan Med Surg 2013;
Suppl 2: S47-54.
Lynde C, Vender R, Bourcier M, Bhatia N.
Clinical features of external genital warts. J
Cutan Med Surg 2013; Suppl 2: S55-60.
Dougherty TJ, Kaufman JE, Goldfarb A,
Weishaupt KR, Boyle D, Mittleman A. Photoradiation therapy for the treatment of malignant tumors. Cancer Res 1978; 38: 26282635.
Iinuma S, Farshi SS, Ortel B, Hasan T. A mechanistic study of cellular photodestruction with
5-aminolaevulinic acid-induced porphyrin. Br J
Cancer 1994; 70: 21-28.
Kennedy JC, Pottier RH, Pross DC. Photodynamic therapy with endogenous protoporphyrin IX: basic principles and present clinical experience. J Photochem Photobiol B 1990; 6:
143-148.
Kennedy JC, Pottier RH. Endogenous protoporphyrin IX, a clinically useful photosensitizer for
photodynamic therapy. J Photochem Photobiol
B 1992; 14: 275-292.
SeFehr MK, Chapman CF, Krasieva T, Tromberg
BJ, McCullough JL, Berns MW, Tadir Y. lective
photosensitizer distribution in vulvar condyloma acuminatum after topical application of
5-aminolevulinic acid. Am J Obstet Gynecol
1996; 174: 951-957.
Stefanaki IM, Georgiou S, Themelis GC,
Vazgiouraki EM, Tosca AD. In vivo fluorescence
kinetics and photodynamic therapy in condylomata acuminata. Br J Dermatol 2003; 149:
972-976.
11346
[11]
[12]
[13]
[14]
[15]
[16]
Kacerovska D, Pizinger K, Kumpova M,
Cetkovska P. Genital warts treated by photodynamic therapy. Skinmed 2007; 6: 295-297.
Nucci V, Torchia D, Cappugi P. Treatment of
anogenital condylomata acuminata with topical photodynamic therapy: report of 14 cases
and review. Int J Infect Dis 2010; 14 Suppl 3:
e280-282.
Liu YX, Zheng HY, Liu XR. 5-aminolaevulinic
acid-photodynamic therapy for the treatment
of cervical condylomata acuminata. Chin Med
Sci J 2009; 24: 151-155.
Wang HW, Zhang LL, Miao F, Lv T, Wang XL,
Huang Z. Treatment of HPV infection-associated cervical condylomata acuminata with
5-aminolevulinic acid-mediated photodynamic
therapy. Photochem Photobiol 2012; 88: 565569.
Chen MK, Luo DQ, Zhou H, Huang ZW, Zhang
QF, Han JD. 5-aminolevulinic acid-mediated
photodynamic therapy on cervical condylomata acuminata. Photomed Laser Surg 2011; 29:
339-43.
Szeimies RM, Karrer S, Sauerwald A,
Landthaler M. Photodynamic therapy with topical application of 5-aminolevulinic acid in the
treatment of actinic keratoses: an initial clinical study. Dermatology 1996; 192: 246-251.
Wang XL, Wang HW, Huang Z, Stepp H,
Baumgartner R, Dannecker C, Hillemanns P.
Study of protoporphyrin IX (PpIX) pharmacokinetics after topical application of 5-aminolevulinic acid in urethral condylomata acuminata.
Photochem Photobiol 2007; 83: 1069-1073.
Mei X, Shi W, Piao Y. Effectiveness of photodynamic therapy with topical 5-aminolevulinic
acid and intense pulsed light in Chinese acne
vulgaris patients. Photodermatol Photoimmunol Photomed 2013; 29: 90-96.
Int J Clin Exp Med 2015;8(7):11342-11346
You might also like
- When You Tell Me That Ou Love MeDocument2 pagesWhen You Tell Me That Ou Love Merahmawati aliwarmanNo ratings yet
- Westlife - My Love Song LyricsDocument2 pagesWestlife - My Love Song LyricsBuddy ArifNo ratings yet
- CREZIERDocument1 pageCREZIERrahmawati aliwarmanNo ratings yet
- F24 - Epilepsy After StrokeDocument6 pagesF24 - Epilepsy After StrokeplocnicuNo ratings yet
- JCN 11 E34Document8 pagesJCN 11 E34kakarafnieNo ratings yet
- What Is RH IncompatibilityDocument30 pagesWhat Is RH Incompatibilityrahmawati aliwarmanNo ratings yet
- Facts About Chikungunya17806 PDFDocument6 pagesFacts About Chikungunya17806 PDFNitin NaharNo ratings yet
- Without You (Reference Vocal) : Posting Lirik Ini Di Blog AndaDocument1 pageWithout You (Reference Vocal) : Posting Lirik Ini Di Blog Andarahmawati aliwarmanNo ratings yet
- All by MyselfDocument2 pagesAll by Myselfrahmawati aliwarmanNo ratings yet
- Bhattacharyya BPPV CPGDocument35 pagesBhattacharyya BPPV CPGrahmawati aliwarmanNo ratings yet
- 10 5923 J Ajdv 20150403 01Document3 pages10 5923 J Ajdv 20150403 01rahmawati aliwarmanNo ratings yet
- Vertigo diagnosis and management in primary careDocument3 pagesVertigo diagnosis and management in primary careAacg MeryendNo ratings yet
- Health Panel Seeks Sweeping Changes in Fertility TherapyDocument4 pagesHealth Panel Seeks Sweeping Changes in Fertility Therapyrahmawati aliwarmanNo ratings yet
- All by MyselfDocument2 pagesAll by Myselfrahmawati aliwarmanNo ratings yet
- Desviat 2006 CcaDocument4 pagesDesviat 2006 Ccarahmawati aliwarmanNo ratings yet
- True Vertigo Patients in Emergency Department An Epidemiologic StudyDocument4 pagesTrue Vertigo Patients in Emergency Department An Epidemiologic Studyrahmawati aliwarmanNo ratings yet
- 38 Acne PDFDocument7 pages38 Acne PDFRamadhan Harya Puja KusumaNo ratings yet
- JCN 11 262Document6 pagesJCN 11 262rahmawati aliwarmanNo ratings yet
- Histamine Antagonists For Treatment of Peripheral Vertigo: A Meta-AnalysisDocument5 pagesHistamine Antagonists For Treatment of Peripheral Vertigo: A Meta-Analysisrahmawati aliwarmanNo ratings yet
- Pi Is 0002934300004125Document8 pagesPi Is 0002934300004125rahmawati aliwarmanNo ratings yet
- 1 SS Skin Cancer - Chapter 1Document12 pages1 SS Skin Cancer - Chapter 1Muhammad IqbalNo ratings yet
- The Analysis of The Mycobacterium Leprae Resistance Against Ofloxacin After The Rifampicin Ofloxacin Minocycline (ROM) TherapyDocument5 pagesThe Analysis of The Mycobacterium Leprae Resistance Against Ofloxacin After The Rifampicin Ofloxacin Minocycline (ROM) Therapyrahmawati aliwarmanNo ratings yet
- Sel KeratinositDocument6 pagesSel KeratinositChristover Firstnando Saragih SimarmataNo ratings yet
- MelasmaDocument5 pagesMelasmarahmawati aliwarmanNo ratings yet
- Human SkinDocument15 pagesHuman Skinrahmawati aliwarmanNo ratings yet
- Bawang Ke SaDocument14 pagesBawang Ke SaDyah Anugrah KiranaNo ratings yet
- J. Nutr.-1992-Yamamoto-871-7Document7 pagesJ. Nutr.-1992-Yamamoto-871-7rahmawati aliwarmanNo ratings yet
- Should We Use Ceftriaxone To Treat Staphylococcal.2Document2 pagesShould We Use Ceftriaxone To Treat Staphylococcal.2rahmawati aliwarmanNo ratings yet
- 5 and Type 8 Capsular Polysaccharides by Type Regulation Of: Staphylococcus AureusDocument6 pages5 and Type 8 Capsular Polysaccharides by Type Regulation Of: Staphylococcus Aureusrahmawati aliwarmanNo ratings yet
- Correspondence: Methicillin-Resistant Staphylococcus Aureus Clinical Strain With Reduced Vancomycin SusceptibilityDocument12 pagesCorrespondence: Methicillin-Resistant Staphylococcus Aureus Clinical Strain With Reduced Vancomycin Susceptibilityrahmawati aliwarmanNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- CPC - Appendicitis (Flowchart)Document1 pageCPC - Appendicitis (Flowchart)Milet NacionalesNo ratings yet
- 5 Minute Fluency - Volume IDocument79 pages5 Minute Fluency - Volume IAlexandre Magno AlvesNo ratings yet
- Test Questionnaire For Needs AnalysisDocument5 pagesTest Questionnaire For Needs AnalysisYenyen Quirog-PalmesNo ratings yet
- Journal Pone 0118161Document10 pagesJournal Pone 0118161David PesireronNo ratings yet
- (Coll.) WHO Classification of Head and Neck Tumour (B-Ok - Xyz)Document285 pages(Coll.) WHO Classification of Head and Neck Tumour (B-Ok - Xyz)Andrea GonzalezNo ratings yet
- ĐỀ 26Document6 pagesĐỀ 26Uyên Lê PhươngNo ratings yet
- Manual of Cardio-Oncology - Cardiovascular Care in The Cancer Patient (PDFDrive)Document472 pagesManual of Cardio-Oncology - Cardiovascular Care in The Cancer Patient (PDFDrive)jimurgaNo ratings yet
- Nursing Management: Nursing Management: Acute Kidney Injury and Chronic Kidney DiseaseDocument22 pagesNursing Management: Nursing Management: Acute Kidney Injury and Chronic Kidney Diseasedian rachmat saputroNo ratings yet
- Adult Acute Lymphoblastic LeukemiaDocument22 pagesAdult Acute Lymphoblastic Leukemiamelki hadisasmitaNo ratings yet
- LiliDocument7 pagesLilialan azizNo ratings yet
- A Case Study On Breast Cancer (2003)Document58 pagesA Case Study On Breast Cancer (2003)Katty Rine100% (6)
- Adrenal Function Urine Test ExplainedDocument30 pagesAdrenal Function Urine Test ExplainedDamarys ReyesNo ratings yet
- Philippine Music and Arts QuizDocument4 pagesPhilippine Music and Arts Quizrizabesmonte100% (1)
- Seed Rotation Ebook Final 2Document10 pagesSeed Rotation Ebook Final 2Andreea Cretiu100% (3)
- Veterinary Surgery and Radiology MCQDocument66 pagesVeterinary Surgery and Radiology MCQJihad Anad81% (59)
- AmebaDocument21 pagesAmebamihaelaemma100% (2)
- Report On KhatDocument13 pagesReport On KhatYounas BhattiNo ratings yet
- Serenoa Repens (Saw Palmetto) A Systematic Review of Adverse EventsDocument11 pagesSerenoa Repens (Saw Palmetto) A Systematic Review of Adverse EventsAdam ZhangNo ratings yet
- Neoplasia Outline Notes - PathologyDocument4 pagesNeoplasia Outline Notes - Pathologykep1313No ratings yet
- Female Genital Cysts Tract PDFDocument6 pagesFemale Genital Cysts Tract PDFRaraNo ratings yet
- The Histological Aspects of Fillers Complications: Ute S. Zimmermann, MD, and Thierry J. Clerici, MDDocument10 pagesThe Histological Aspects of Fillers Complications: Ute S. Zimmermann, MD, and Thierry J. Clerici, MDMichele CarvalhoNo ratings yet
- DR J GowingDocument2 pagesDR J GowingkaylekayprNo ratings yet
- INTUSSUSCEPTIONDocument1 pageINTUSSUSCEPTIONMaecy PasionNo ratings yet
- Diabetes Mellitus Part 1 - Prof - AskandarDocument40 pagesDiabetes Mellitus Part 1 - Prof - AskandarAdekresnaHernataNo ratings yet
- The detection of Bence Jones protein in urine by the heat test helps in diagnosis of multiple myelomaDocument4 pagesThe detection of Bence Jones protein in urine by the heat test helps in diagnosis of multiple myelomaCarla PereiraNo ratings yet
- RACGP - Bones and JointsDocument31 pagesRACGP - Bones and JointstjelongNo ratings yet
- Medical TerminologyDocument47 pagesMedical TerminologyGina Andinia AzizahNo ratings yet
- Zebra XX, Part 2 PDFDocument3 pagesZebra XX, Part 2 PDFRamona MateiNo ratings yet