Professional Documents
Culture Documents
RC Managing Hemodynamics During HFOV JA en
Uploaded by
sgod34Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
RC Managing Hemodynamics During HFOV JA en
Uploaded by
sgod34Copyright:
Available Formats
ritical Care Review
CURRENT APPLICATIONS AND ECONOMICS
Managing Hemodynamics During
High Frequency Oscillatory Ventilation
Stephen Minton, MD
Matching Ventilation/Perfusion
The goal of breathing is to match alveolar ventilation
with pulmonary perfusion to obtain an ideal V/Q
balance as it is the major determinant of PaO2 and
PaCO2. While our ventilation management determines
the "V" component, there are three major determinants
of pulmonary "Q". They are myocardial function, the
pulmonary blood volume, and pulmonary vascular
resistance (PVR).
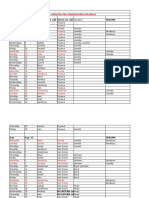
There are many factors which play a role in PVR. The
lung is not a passive participant in PVR but plays an
active role affecting PVR by lung volume (Figure 1).
The lung parenchyma not only tethers the airways, but
tethers the extra alveolar vessels. At low lung volume,
there is a reduction in radial traction reducing the
cross-sectional area of the extra alveolar vascular bed,
increasing PVR in these vessels. As lung volume
increases, PVR falls to its minimal level at an optimum
lung volume. However, if mean airway pressure (Paw)
continues to increase lung volume resulting in over
distention of the alveoli, this results in compression of
the intra-alveolar vessels which lack perivascular
support resulting in a rise of PVR. Because of this direct
action by the ventilator on a major component of
hemodynamic performance, it is therefore important to
track hemodynamic responses while changing Paw.
Clinical Cardiovascular Monitoring Heart Rate
Monitoring the heart rate is an essential element for
0.11
cmH2O
cc/min
0.12
vascular resistance
Introduction
There is an inextricable link between hemodynamic
characteristics and response to ventilation settings.
Therefore, a careful evaluation of cardiovascular
function in critically ill patients with pulmonary
disease is an important aspect of their ventilatory
management. It is also then important to understand
and utilize those tools and measurements that will
enhance our understanding of these inter-relationships.
0.10
0.09
0.08
0.07
0.06
50
100
150
200
lung volume (cc)
Figure 1.
evaluating the cardiovascular status. The pediatric
heart rate is influenced by age and disease process.
Neonates have the added influence of gestational age
and weight. Additional influences on heart rate include
central nervous system dysfunction, autonomic
dysfunction, stress, drugs, sepsis, anemia,
hyperthermia, and endocrine dysfunction (e.g. thyroid).
Since cardiac output equals stroke volume times heart
rate, monitoring changes in heart rate can reflect an
acute change in the patients condition or trend
impending problems.
Patients in respiratory failure frequently have an
increase in heart rate to improve cardiac output and to
compensate for decreased oxygenation. Although,
increasing heart rate is an effective mechanism for
increasing cardiac output, there is a point when
increasing the heart rate will cause the cardiac output
to decrease as the decreased time for ventricular filling
and coronary blood flow effect cardiac efficiency.
Bradycardia can be associated with episodes of apnea
ritical Care Review
and hypoxia. Other physiologic dysfunctions
associated with a decrease in heart rate include cardiac
ischemia, mechanical defects, hypovolemia, and
increased vascular resistance. On rare occasions, it has
been seen secondary to a reflex response to high PEEP
or Paw.
Blood Pressure
Arterial blood pressure is the dynamic measurement of
the force of blood against the wall of the artery
reflected during systole (tension during LV contraction),
and diastole (relaxation pressure during ventricular
diastole). Pulse pressure, the difference between the
systolic and diastolic, reflects the ventricular ejection
amplitude. Normal values vary in the pediatric patient
by age, sex, and method of monitoring. Neonates
have the additional effects of gestational age, birth
weight, and postnatal age to consider.
C U R R E N T A P P L I C AT I O N S A N D E C O N O M I C S
About 70% of the time, the correct placement is
approximately T9 on AP chest x-ray. With normal
cardiac status, CVP reflects right atrium pressure,
which correlates with right ventricular pressure. CVP is
used to evaluate pre-load to the right ventricle. It
allows us to evaluate hemodynamic states such as
intravascular volume, intra-thoracic pressure, and
response to volume replacement.
The normal range for CVP in the neonate and pediatric
patient varies, ranging from 0-8 mmHg. However, in
our experience, we cannot usually use high frequency
oscillatory ventilation (HFOV) effectively if the CVPs in
the 0-3 mmHg range, but may require CVPs of 5-8
mmHg to allow increasing Paw above the critical
opening pressure of the lung.
Hypotension may result from true low blood volume,
low effective blood volume secondary to peripheral
vasodilatation, or left ventricular dysfunction.
Hypotension induced reduction in oxygenation delivery
may result in tissue hypoxia and elevation of lactic acid
levels. Hypertension, or an elevated blood pressure,
can be the result of increased peripheral vascular
resistance or fluid overload. Pulse pressure can be
increased with the left-to-right shunt from a patent
ductus arteriosus (PDA) or decreased by shock,
hypovolemia, or heart failure.
In the pediatric population, considerable information
can be obtained from the arterial pressure tracing. The
shape of the tracing, pulse pressure, and location of
the dicrotic notch, all give pertinent hemodynamic
information about the patient.
Central Venous Pressure
Central venous pressure (CVP) is the pressure obtained
from a catheter inserted into the superior vena cava or
the right atrium. It is crucial when using this pressure
to be certain of the catheters placement (Fig 2). In the
neonate, slight displacement of the catheter from the
right atrium can result in fictitious measurements.
These errors can result from placing the catheter
across the foramen ovale into the left atrium, or by
placing it too far into the right atrium with partial
obstruction from the intra-atrial septum. If the catheter
is not inserted far enough, the pressure may reflect
hepatic pressures. Both an AP and lateral chest x-ray
for placement is very helpful. In our nursery, we
document UVC placement with ultrasonography.
Figure 2.
CVPs decrease in hypovolemia or with any mechanism
causing delayed venous return to the right heart.
Increasing levels of Paw without blood volume
expansion can also cause decreases in venous return.
Increases in CVPs are seen in right heart failure,
hypervolemia, or myocardial dysfunction.
While the validity of CVP in the critically ill or
mechanically ventilated patient has been questioned, in
our experience, if the CVP is placed in the appropriate
position (entrance of right atrium), it is very valuable in
evaluating right ventricular preload.
Pulmonary Artery Occlusion or Wedge Pressure
Pulmonary artery occlusion or wedge pressure is
used for measuring the preload for the left ventricle.
The Swan-Ganz catheter introduction by right heart
ritical Care Review
C U R R E N T A P P L I C AT I O N S A N D E C O N O M I C S
catheterization into the pulmonary artery (PA) is the
standard method in pediatrics and adults for evaluating
pulmonary vascular hemodynamics. The indications
for a PA catheter include discriminating cardiac and
noncardiac causes of pulmonary infiltrates, titration of
fluid therapy, evaluation of pharmacologic
interventions in pulmonary hypertension, and to
determine the etiology of hypotension.
To obtain a pulmonary capillary wedge pressure
(PCWP), the distal lumen of the catheter is used.
Balloon inflation isolates the distal tip of the catheter
from upstream pulmonary arterial pressure creating a
static, nonflowing column of blood distal to the
balloon. Without flow there is no pressure drop along
the column of fluid. The pressure at the catheter tip
measures pressure in the pulmonary vein. Because
there is normally minimal resistance in the pulmonary
veins, the pressure measured approximates the
pressure in the left atrium.
Oxygen Delivery
Oxygen tension (PaO2) is the partial pressure of oxygen
in the arterial blood. PaO2 is affected by FiO2, alveolar
ventilation, diffusion defects, V/Q mismatch, and shunt
(intrapulmonary or intracardiac). Oxygen is carried by
the blood in two ways. Although we frequently focus
on PaO2, this dissolved oxygen (0.0031 ml/torr) is only
a small fraction (< 5%) of O2 carried in the blood. The
remaining and most significant portion is carried
bound with the hemoglobin (Hb) as determined by the
O2 saturation. Each gram of Hb can carry 1.34 ml of O2
and therefore, the arterial oxygen content (CaO2) or the
total amount of oxygen carried is dramatically effected
by changes in hemoglobin.
Normal CaO2 is approximately 20 ml O2/dl blood
(Vol%). To emphasize the difference between PaO2 and
CaO2 (CaO2 = O2 carried by Hb + dissolved O2),
consider the aspects of varying Hb concentration on
the following patients:
Patient 1:
The CaO2 for a child with a Hb of
15 gm, PaO2 of 100 torr and O2 Sat
of 97%:
= (15 x 1.34 x 0.97) + (0.0031 x 100)
= 19.50 ml O2/dl + 0.31 ml O2/dl
= 19.81 ml O2/dl
Patient 2:
The CaO2 for a child with a Hb of
8 gm, PaO2 of 100 torr and O2 Sat
of 97%:
CaO2 = O2 carried by Hb + dissolved O2
= (8 x 1.34 x 0.97) + (0.0031 x 100)
= 10.40 ml O2/dl + 0.31 ml O2/dl
= 10.71 ml O2/dl
These two examples demonstrate the dramatic fall in
blood oxygen content that occurs with the fall in Hb.
Although both patients have the same PaO2 and O2
Sat, the second patient must almost double cardiac
output to maintain the same oxygen delivery as the
first patient.
Oxygen Extraction
The Arterial-Venous Difference (A-VDO2)
The Arterial-Venous difference (A-VDO2) is the amount
of O2 extracted by the tissues and is commonly used in
the ICU as an indirect measurement of cardiac output.
The A-VDO2 is derived from oxygen content
calculations from arterial and mixed venous blood
drawn simultaneously. The normal CaO2 is
approximately 20 Vol% while the CvO2 is 15 Vol%.
Therefore only 5 ml O2 in each 100 ml is extracted for
utilization by the tissues. An increase in the A-VDO2
indicates that either tissue extraction has increased or
cardiac output has decreased. Conversely, a decrease
in the A-VDO2 usually indicates an increase in cardiac
output. Ideally, a true venous sample should be drawn
from the pulmonary artery. If drawn from the right
atrium, there is an increased probability for poor
venous mixing and loss of data reliability.
Cardiac Output In Pediatric Patients
Methods used to directly measure cardiac output in
pediatric patients include the Fick equation, dye
indicator-dilution and most commonly by the use of
thermal dilution. The thermal dilution technique utilizes
injection of chilled 0.9% sodium chloride into the
right atrium while the temperature of the blood is
constantly measured in the pulmonary artery with a
thermistor-tipped catheter. The warming of the saline
reflect the blood flow heat transfer. This is an accurate
method of determining cardiac output that allows
repeated measurements, however, consideration must
be given when administering volume to infants and
small children relative to the potential for fluid
overload. The newest thermal dilution technology
replaces cold boluses as an indicator with pulses of
energy from a thermal filament in the catheter. This
eliminates the potential of fluid overload and can
provide continuous measurements.
ritical Care Review
Cardiac performance can also be assessed clinically by
observation of indirect signs, frequently presented as
the signs of poor organ perfusion. Signs and
symptoms of low cardiac output include cool and pale
extremities (skin), oliguria (renal), and decreased level
of consciousness (CNS). Variables that may be used
indirectly to measure the adequacy of cardiac output
include: systemic blood pressure, right atrial pressure
(CVP), left atrial pressure (LAP), urine output, blood pH
and lactate levels, and arterial venous oxygen
difference (A-VDO2).
Because pediatric patients have greater variation in
size, it is important to normalize cardiac output by the
cardiac index (CI = cardiac output per square meter of
body surface area). The CO in children is higher per
kilogram of body weight than the adult, resulting in a
higher CI. When comparing the childs cardiac function
to the adult, it is important to note that the range
of increase in stroke volume is much smaller and
therefore a childs cardiac output is more directly
proportional to heart rate. Tachycardia in the
pediatric patient is the most efficient way to increase
cardiac output.
Echocardiographic Evaluation of
Cardiovascular Function
The heart is a parallel pump that delivers blood into
two circuits, the right heart to the lungs and the left
heart to the systemic circulation. It is critical that these
parallel pumps work in sync to meet the metabolic
demands of the body for oxygen and nutrients and the
removal of the byproducts of metabolism. In the
neonate where signs and symptoms of respiratory
distress, sepsis, and metabolic derangements may
mimic those of congenital heart disease, it may be
more difficult to arrive at a correct hemodynamic
interpretation at the bedside without more advanced
technology. In complex heart-lung interactions,
the only true methods to evaluate myocardial
function are with an echocardiogram and pulmonary
artery catheter.
Left Ventricular Performance
The stroke volume component of CO is affected
by cardiac preload, myocardial contractility and
afterload. Stroke volume will rise when preload
or myocardial contractility improves and fall when
afterload increases.
The measurement of left ventricular end-diastolic
volume (LVED) reflects preload. This volume effects the
C U R R E N T A P P L I C AT I O N S A N D E C O N O M I C S
stretch of the myocardial fiber length. Preload
decreases with blood loss, inadequate fluid
maintenance and during positive pressure ventilation.
Fluid volume replacement will usually correct a
decreased preload in a healthy myocardium. Fluid
overload increases preload and can be treated with
diuretics. Preload can be evaluated using CVP and
circumferential fiber shortening (VCFc).
Afterload is the resistance to blood flow from the
ventricle and is effected by aortic pressure, radius of
the ventricle, peripheral vascular resistance and the
viscosity of the blood. It increases with hypertension
and an enlarged ventricle. Decreases in afterload are
seen with anemia, vasodilation and central shunting of
blood volume. Pharmacologic agents such as
Nitroprusside that alter vascular tone will also change
right and left ventricular afterload. Left ventricular
afterload can be evaluated measuring left ventricular
posterior wall stress. Laplaces Law states that wall
stress of a chamber is equal to the pressure times the
cavity diameter/wall thickness. Combining blood
pressure with left ventricular wall thickness and cavity
dimensions allows calculation of peak systolic wall
stress (PSS).
The force of contraction of the heart, reflected in the
efficiency of myocardial fiber shortening, is called
contractility. Left Ventricular Shortening Fraction (LVSF)
and Ventricular Ejection Fraction (VEF) are best
estimated when the left ventricle is circular. In the
premature infant, there is intraventricular septal
flattening causing distortion of the shape of the left
ventricle and a decrease in circularity. This results in a
shortening fraction in the neonate which can
underestimate the differences in regional ventricular
function. Decrease in contractility occurs with hypoxia,
acidosis, with certain drugs and glucose abnormalities.
Inotropic drugs will usually improve contractility and
cardiac output once preload deficits have been
corrected. Common inotropic agents utilized to
improve contractility include Dopamine, Dobutamine,
Epinephrine, Isoproterenol, Norepinephrine and
Amrinone. The ratio of PSS and VCFc allows better
evaluation of myocardial function by reducing the
effect of preload and postload. Other echocardiographic
measures that may assist in evaluation of left
ventricular function include Left Ventricular Cardiac
Output calculated from the velocity time integral aortic
valve area and heart rate, Left Ventricular Volume, and
Left Ventricular Systolic Time Interval (LVSTI) as an
index of LVS function.
C U R R E N T A P P L I C AT I O N S A N D E C O N O M I C S
Right Ventricular Performance
In the neonate, the right heart is more difficult to
evaluate echocardiographically. The right ventricle lies
directly beneath the sternum, has an irregular crescent
shape, and trabeculated walls. Useful right ventricular
performance measurements include right ventricular
afterload (estimated by measuring right ventricular end
diastolic diameter-RVEDD), Right Systolic Time Interval
(RSTI), and Right Ventricular Output (calculated from
the velocity time integral x pulmonary valve area x
heart rate).
Pulmonary Artery Pressure
Echocardiography is also an ideal noninvasive method
for estimating pulmonary artery pressure and
evaluating the degree of pulmonary artery
hypertension. Right ventricular systolic time intervals
can reflect elevated pulmonary vascular resistance.
Echocardiography can be used to measure the velocity
and direction of flow across the PDA. Use of the
tricuspid regurgant jet across the tricuspid valve and
CVP in a simplified Bernoullis equation gives an
estimate of the Systolic Pulmonary Artery Pressure
(SPAP). This method has been shown to be more
reliable than the other echocardiographic methods.
Ductus Venous
The ductus venous can be assessed ultrasonographically
for flow pattern. The flow pattern reflects the
portocaval pressure gradient and the pressure on the
right side of the heart and in the pulmonary arteries.
Shunts
Patterns of flow across a Patent Foramen Ovale (PFO)
or ductus arteriosus can be recorded by color flow and
pulsed-wave Doppler studies. The size of the defect,
direction of shunt, and velocity can be estimated.
Contrast echocardiography to evaluate PFO flow using
an agitated saline flush can be performed if color flow
is unsatisfactory.
Hemodynamics In High Frequency Oscillatory
Ventilation
Abnormal respiratory function treated with assisted
mechanical ventilation can alter lung volume,
pulmonary vascular resistance, or intrathoracic
pressure. All of these can have significant effects on
normal and abnormal circulatory function. During
conventional mechanical ventilation (CMV) increasing
the tidal volume can decrease venous return.
Increasing PEEP is associated with decreased cardiac
output, although cardiac function has generally been
observed to be normal with PEEP.
The decreased cardiac output with PEEP appears to be
due to decreased venous return. Administration of
fluids can usually overcome the decreased venous
return and restore cardiac output.
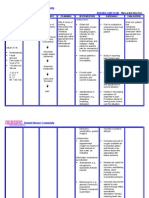
ZEEP
Venous Return/Cardiac Output
ritical Care Review
PEEP 10
PEEP 20
VR0
A
B
VRP
C
D
Right Atrial Pressure MCPZEEP
MCPPEEP
Figure 3. Effects of PEEP on the Determinants of
Venous Return
The decreased venous return with increasing PEEP can
be explained in Figure 3. As lung volume increases
with PEEP, intrathoracic pressure increases by an
amount determined by chest wall compliance and the
lung volume. This effect is transmitted to the right
atrium, where it decreases venous return. As PEEP
increases from zero to 20 (PEEP 20 = cardiac function
curve with PEEP 20), there is a progressive rightward
shift in the cardiac function curves (ZEEP = cardiac
function curve with zero end expiratory pressure; PEEP
10 and PEEP 20 = cardiac function curve with 10 and 20
cmH20 PEEP). The point of intersection between the
cardiac function and venous return curves shifts from
Point A to B to C. Point D is a theoretical point of
intersection between the original venous return curve
and the cardiac function curve on PEEP, which would
have been the situation had mean circulatory pressure
not increased with PEEP. Thus, increased mean
circulatory pressure buffered the effects of increased
PEEP on cardiac output and venous return. There is
also a decrease in the downward slope of the venous
return curve with PEEP which suggests an increase in
the resistance to venous return as well. In addition,
Fessler demonstrated a vascular waterfall in the
Inferior Vena Cava (IVC) associated with mechanical
compression of the lower lobes of the right lung on the
ritical Care Review
IVC causing a flow limitation. Veddeng found PEEP
applied to the right lung alone limits cardiac output
more than PEEP to the left lung alone. This effect may
be explained on the basis of either direct mechanical
compression by the inflating lung on the right ventricle
and right atrium with greater increases in right atrial
pressure and hence greater decreases in venous return
or exceeding a critical closing pressure of the inferior
vena cava.
There have been relatively few studies in the literature
concerning cardiovascular effects of HFOV, especially
in immature subjects.
The ventilatory strategy used in all pathophysiologies
except gross air leak is an optimum lung volume
strategy. Because the tidal volumes are very small in
HFOV, the lung volumes remain near constant. Mean
airway pressure is increased on the inflation limb of
the pressure volume above the critical opening
pressure of the lung. Lung volume is maintained above
the critical closing pressure of the lung on the deflation
limb of the hysteresis curve. This results in a higher
PEEP than seen in CMV. However, because in CMV
there is an expiration time with a lower pressure
(usually a low PEEP), it is more forgiving in its effect on
venous return for the same blood volume than the
higher PEEP seen in HFOV. Although when HFOV
Paw is similar to that of CMV, several authors found no
significant differences in cardiac output, organ blood
flow, or metabolic status.
Traverse, et al, found impairment of hemodynamics on
HFOV in the cat model. They found that cardiac output
decreased and pulmonary vascular resistance
increased with increasing Paw. Although the response
was diminished in animals with decreased respiratory
system compliance, it was not eliminated.
Kinsella, et al, investigated the hemodynamic
consequences of ventilator strategies for HFOV and
CMV in the baboon model of HMD using the radio
labeled microsphere technique. Measuring cardiac
output and organ blood flow at three time points (3, 8,
and 23 hours) showed no significant differences in left
ventricular output, effective systemic flow, organ blood
flow, or central venous pressure. The HFOV strategy
resulted in significant improvement in oxygenation
during the 24 hours of treatment without adverse effect
on left ventricular output, cerebral blood flow, or
central venous pressure.
C U R R E N T A P P L I C AT I O N S A N D E C O N O M I C S
Nicol, et al, studied changes in aortic blood flow and
blood pressure in normal and surfactant deficient
rabbits under varying ventilator strategies of
Conventional Tidal Volume Ventilation (CMV), Inverse
Ratio Ventilation (IRV), High Frequency Positive
Pressure Ventilation (HFV) and High Frequency
Oscillatory Ventilation (HFOV). Each strategy was also
studied at PEEP (Paw) levels of 0, 5 and 10 cmH2O. In
the injured lungs, when 10 cmH2O of distending
pressure was applied, PaO2 increased with all modes,
but the aortic blood flow was significantly reduced
(p<0.05) with a 40% reduction in calculated oxygen
delivery during CMV and IRV as compared to HFV or
HFOV. They concluded that hemodynamic stability is
better maintained during HFV or HFOV when high
PEEP levels are required for oxygenation.
Minton, et al, compared the hemodynamics in 100
newborn infants with birth weights less than 2500
grams with RDS randomized to either CMV and
surfactant or HFOV and surfactant. The strategy used
on HFOV was an optimum lung volume strategy. They
found no difference in cardiac output or right and left
ventricular hemodynamics if close attention was paid
to blood volume expansion.
We have subsequently reported on 299 patients on
HFOV who underwent 1420 echocardiograms in the
first 21 days of life. In these patients (GA 22.5 to 42
weeks and BW 310 to 5200 grams) we found a slight
increase in cardiac output with advancing gestation
age and birth weight increasing from 280 cc at 23
weeks to 300 cc at 41 weeks. Mean cardiac output was
314 cc/kg/mm with a standard deviation of 28
cc/kg/mm. There did not appear to be any effects on
left or right hemodynamics, cardiac output, or
incidence of patent ductus arteriosus or foramen ovale
shunting in these patients. The cardiovascular effects
of a patent ductus arteriosus (in a premature baboon
model of HMD treated with CV or HFOV) were studied
by Yoder, et al. There were no significant differences
between the two forms of ventilation when MAP, HR,
CO, or modes of ventilation were compared.
Gutierrez, et al, evaluated eight of their pediatric
patients who had been managed with HFOV for severe
respiratory failure and had pulmonary artery catheters
in place. With significant 50% increases in mean
airway pressures from CMV to HFOV (20.9 cmH2O to
30 cmH2O), the only observed effect was a mean
reduction in heart rate of 20 beats/min. Oxygen
ritical Care Review
delivery, cardiac index, and mean systemic arterial
blood pressure did not change significantly following
the change to HFOV with the exception of one patient.
Blood Volume Expansion and Inotropic Support
Venous return is influenced by the blood volume and a
reduction will cause a decrease in cardiac output and
hypotension. It is important to correct hypovolemia by
fluid replacement. Decreases in cardiac output may
also occur in patients with normal volume status and
inotropic drugs may be used to improve their
myocardial function.
C U R R E N T A P P L I C AT I O N S A N D E C O N O M I C S
repeated times three until cardiac output improves
which will be reflected by an increase in RAP greater
than 2 mmHg than the original pressure. If there is no
improvement, an echocardiogram should be
performed for spatial anatomy, myocardial function,
and chamber dimensions.
Inotropic Support
Dopamine
1. Low Dose: 2-5 g/kg/min IV. Low dose Dopamine
increases renal perfusion and has a minimal effect on
heart rate and cardiac output.
Measurement of the left atrial pressure (LAP) provides
the most accurate guide to fluid replacement and is the
earliest indicator of hypovolemia. CVP reflects the
right ventricular end diastolic pressure. Although CVP
is often a poor correlate of left-sided filling pressure,
its measurement is important in the assessment of
right-sided pressure of the patients with right-sided
obstructive lesions.
2. Intermediate Dose: 5-15 g/kg/min IV. Effects
include increases in renal perfusion, heart rate, cardiac
contractility and cardiac output.
Preload is best assessed by the measurement of LAP.
If filling pressures are low, volume should be
administered using normal saline, lactated Ringers,
Plasmatate, plasma, 5% albumin, or blood transfusion.
In the neonate, usual fluid replacement is administered
with 5-10% glucose at a rate of 80-100 ml/kg/day.
When cardiac output is compromised, a fluid challenge
may be required until stabilization occurs.
Dobutamine
Once the preload is optimized, cardiac output and
systemic blood pressure should be measured again. If
the output is still low, but the BP is now elevated, a
peripheral vasodilator should be used to decrease
ventricular afterload (nitroprusside + nitroglycerin).
Preload should be carefully monitored during the
infusion of vasodilators as sudden peripheral
vasodilatation may increase the need for volume
administration. If the cardiac output and blood
pressure remain low after preload optimization, then
contractility should be increased by the use of inotropic
agents. Several drugs that are used have both
inotropic and vasoactive properties.
RAP of less than 6 mm Hg may be challenged with
fluid bolus of 10 ml/kg. Pressures between 6-10 mmHg
may require a fluid bolus of 5 ml/kg and pressures of
greater than 10 mmHg may respond to a bolus of 3
ml/kg. All volume is infused over 30-60 minutes. If the
RAP continues to be within 2 mmHg of the original
measurement repeat the fluid bolus. The bolus can be
3. High Dose: >20 g/kg/min IV. High doses increase
systemic vascular resistance and supports arterial BP.
High doses of Dopamine decreases renal perfusion.
4. Maximum Dose: 20-50 g/kg/min IV.
1. Continuous IV infusion: 2.5-15 g/kg/min.
Dobutamine is an effective beta adrenergic and
increases arterial BP and myocardial contractility.
Tachycardia and hypertension may occur.
2. Maximum Dose: 40 g/kg/min.
Intractable Shock
Patients on HFOV that experience intractable shock in
the face of maximum inotropic support and adequate
fluid administration should be considered for
alternative treatment. These alternatives include
transitioning the patient back to conventional
mechanical ventilation or transfer to an ECMO facility.
In our experience, careful selection of mean airway
pressures to optimize lung inflation, adequate fluid
administration with appropriate inotropic agent and
use of all the monitoring techniques described in this
article, has limited cases of intractable shock to a
handful in more than 600 infants we have treated with
the SensorMedics 3100A.
ritical Care Review
C
CU
UR
RR
RE
EN
NT
T A
AP
PP
PL
L II C
CA
AT
T II O
ON
NS
S A
AN
ND
D E
EC
CO
ON
NO
OM
M II C
CS
S
15 Johnson KB. The Harriet Lane Handbook (Reference
Book). Mosby, 1993.
REFERENCES
1 Arnold JH et al. High frequency oscillatory ventilation in
pediatric respiratory failure. Crit Care Med 1993;21:272-8.
2 Arnold JH et al. Prospective, randomized comparison of
high frequency oscillatory ventilation and conventional
mechanical ventilation in pediatric respiratory failure. Crit
Care Med 1994;22:1530-9.
3 Berglund JE, Haldn E, Jakobson S, Svensson J. PEEP
ventilation does not cause humorally mediated cardiac output
depression in pigs. Intensive Care Med 1994;20:360-364.
4 Berglund JE, Haldn E, Jakobson S. The effect of PEEP
ventilation on cardiac function in closed chest pigs. Ups J
Med Sci 1994;99:167-178.
5 Blumer J. Pediatric Intensive Care (3rd Ed).
6 Boyton BR, Waldemar CA, Jobe AH. New therapies for
neonatal respiratory failure (Reference Book). Cambridge
University Press, 1994.
7 Clark RH, Null DM. High frequency oscillatory ventilation
(Book Chapter). Neonatology for the Clinician. 1993 Chapter
24, pp. 289-309.
8 Dally EK, Schroeder JS. Bedside Hemodynamic Monitoring
(Reference Book). Mosby, 1985.
9 Dantzker DR, Scharf SM. Cardiopulmonary Critical Care
(Reference Book). WB Saunders, 1998.
10 Fessler HE, Brower RG, Shapiro EP, Permutt S. Effects of
positive end-expiratory pressure and body position on
pressure in the thoracic great veins. Am Rev Resp Dis 1993;
148:1657-1664.
11 Fessler HE, Brower RG, Wise RA, Permutt S. Effects of
positive end-expiratory pressure on the canine venous return
curve. Am Rev Resp Dis 1992;146:4-10.
12 Goldsmith JP. Assisted Ventilation of the Neonate
(Reference Book). WB Saunders, 1998.
13 Gutierrez JA et al. Hemodynamic effects of high frequency
oscillatory ventilation in severe pediatric respiratory failure.
Intensive Care Med 1995;21:505-10.
14 Hazinski T. Nursing Care of the Critically III Child (2nd Ed).
16 Kinsella, JP, Gerstmann DR, Clark RH et al. High frequency
oscillatory ventilation versus intermittent mandatory
ventilation: Early hemodynamic effects in the premature
baboon with hyaline membrane disease. Pediatric Research
1991; 29:160-166.
17 Minton SD. Echocardiographic comparison of high
frequency oscillatory ventilation to conventional mechanical
ventilation in neonate with respiratory distress syndrome
during the first twenty-four hours of life (Abstract). Soc Crit
Care Med 1996.
18 Minton SD, Gerstmann DR, Stoddard RA. Use of high
frequency oscillatory ventilation in newborns (Course
Syllabus). 1995 Utah Valley Regional Medical Center Advance
Training Course, Provo, Utah.
19 Morrow WR, Taylor AF, Kinsella JP, et al. Effect of ductal
patency on organ blood flow and pulmonary function in the
preterm baboon with hyaline membrane disease. Critical Care
Medicine 1995; 23:179-186.
20 Nicol ME, Dritsopoulou A, Wang C, et al. Ventilation
techniques to minimize circulatory depression in rabbits with
surfactant deficient lungs. Pediatr Pulmonol 1994; 18:317-322.
21 Sprung CL. The Pulmonary Artery Catheter (Reference
Book). University Park Press, 1993.
22 Traverse JH et al. Impairment of hemodynamics with
increasing mean airway pressure during high frequency
oscillatory ventilation. Pediatr Res 1988;23:628-31.
23 Veddeng OJ, Mybre ES, Risow C, Smiseth OA. Selective
positive end-expiratory pressure and intracardiac dimensions
in dogs. J Appl Physiol 1992;73:2016-2020.
24 Weil MMH, Henning RJ. New concepts in the diagnosis
and fluid treatment of circulatory shock. Anesth Analg 1979;
58:124-131.
25 West JB. Pulmonary Pathophysiology (Reference Book).
Williams & Wilkins, 1977.
26 Yoder BA, Kuehl TJ, deLemos RA, et al. Patent ductus
arteriosus during high frequency ventilation for hyaline
membrane disease. Critical Care Medicine 1987:
15:587-590.
ABOUT THE AUTHOR...
Stephen D. Minton, MD
Dr. Minton is the Director of Newborn Services and Medical Director of the Perinatal Center at Utah Valley Regional
Medical Center in Provo, Utah as well as the Medical Director of Newborn Nurseries at Orem Community Hospital in
Orem, Utah. He has been a staff Neonatologist at UVRMC since 1979 and participates in numerous Neonatal and
Pediatric Committees and Programs. He is also a member of several medical associations, community activities, and
involved in clinical research studies for the improvement of managing the critically ill.
SensorMedics Corporation
22705 Savi Ranch Parkway
Yorba Linda, CA 92887-4645
Telephone: (800) 520-4368 (714) 283-1830
Fax: (714) 283-8493
http://www.sensormedics.com
P/N 770118-006 Copyright SensorMedics Corporation 1999
SensorMedics BV
Rembrandtlaan 1b
3723 BG Bilthoven
The Netherlands
Telephone: (31) 30 2289711
Fax: (31) 30 2286244
8#
You might also like
- NOAC ChartDocument2 pagesNOAC Chartsgod34No ratings yet
- Laparoscopic Peritoneal Entry TechniquesDocument52 pagesLaparoscopic Peritoneal Entry Techniquessgod34100% (1)
- Nutrition Support: Sean P Harbison MDDocument42 pagesNutrition Support: Sean P Harbison MDsgod34No ratings yet
- Modes of Mechanical VentilationDocument4 pagesModes of Mechanical Ventilationsgod34100% (1)
- Resident Rotation Schedule 2015-16 - FinalDocument14 pagesResident Rotation Schedule 2015-16 - Finalsgod34No ratings yet
- Abdominal InfectionsDocument6 pagesAbdominal InfectionsPatrico Rillah SetiawanNo ratings yet
- Surgery Preround Template SkeletonDocument2 pagesSurgery Preround Template Skeletonsgod34No ratings yet
- 2012 KevinSextonMay2 BC Wound HealingDocument40 pages2012 KevinSextonMay2 BC Wound HealingYulinda PrimilisaNo ratings yet
- Espinal STS PDFDocument2 pagesEspinal STS PDFsgod34No ratings yet
- Espinal STSDocument2 pagesEspinal STSsgod34No ratings yet
- Nadelman STSDocument2 pagesNadelman STSsgod34No ratings yet
- Basic Ventilator y ModesDocument47 pagesBasic Ventilator y ModesAlina VanceaNo ratings yet
- Venous DiseaseDocument50 pagesVenous Diseasesgod34No ratings yet
- Venous Disorder - GodelmanDocument27 pagesVenous Disorder - Godelmansgod34No ratings yet
- Master Schedule 10-22Document65 pagesMaster Schedule 10-22sgod34No ratings yet
- Abnormal LFTs in General PracticeDocument57 pagesAbnormal LFTs in General Practicesgod34No ratings yet
- Veins More DistensibleDocument27 pagesVeins More Distensiblesgod34No ratings yet
- Lecture 5 Vascular Disorders StudentsDocument103 pagesLecture 5 Vascular Disorders Studentssgod34No ratings yet
- Endoscopy TechniqueDocument8 pagesEndoscopy Techniquesgod34No ratings yet
- 7 MedEd Vascular Jonny Hodgkinson 12.11.12 1Document35 pages7 MedEd Vascular Jonny Hodgkinson 12.11.12 1sgod34No ratings yet
- HemostasisDocument38 pagesHemostasissgod34100% (1)
- ABSITE REVIEW: Vascular Cranial Nerves and Leg UlcersDocument183 pagesABSITE REVIEW: Vascular Cranial Nerves and Leg Ulcerssgod34No ratings yet
- Fluid Resucitation, 2015Document44 pagesFluid Resucitation, 2015sgod34No ratings yet
- ABX Dosing & RDocument11 pagesABX Dosing & Rsgod34No ratings yet
- Guidelines Management 2007w Bookmarks PDFDocument0 pagesGuidelines Management 2007w Bookmarks PDFdiaga081No ratings yet
- Colon CADocument16 pagesColon CAsgod34No ratings yet
- General Surgery - DR Tadros - CompressedDocument164 pagesGeneral Surgery - DR Tadros - Compressedsgod34No ratings yet
- Bile Duct Injuries: Dr. Joe M Das Junior Resident S3 UnitDocument149 pagesBile Duct Injuries: Dr. Joe M Das Junior Resident S3 Unitsgod34No ratings yet
- Anast Bleed MMDocument17 pagesAnast Bleed MMsgod34No ratings yet
- Bile Duct Injuries: Dr. Joe M Das Junior Resident S3 UnitDocument149 pagesBile Duct Injuries: Dr. Joe M Das Junior Resident S3 Unitsgod34No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Science Daily Test 1Document5 pagesScience Daily Test 1yuniNo ratings yet
- Acyanotic CHDDocument83 pagesAcyanotic CHDmrinmayee deshmukhNo ratings yet
- Right Sided Heart Failure Case 4.2Document4 pagesRight Sided Heart Failure Case 4.2Athari AdityaNo ratings yet
- Stroke and HypertensionDocument4 pagesStroke and HypertensionKhessie Laye Garcia JacintoNo ratings yet
- Cardiology: 27 Maret 2021Document52 pagesCardiology: 27 Maret 2021Dian ParamitaNo ratings yet
- Guide to Cardiac Exam Findings and DiagnosesDocument58 pagesGuide to Cardiac Exam Findings and Diagnoseseliaszavaleta100% (1)
- Cuarta Definicion de InfartoDocument41 pagesCuarta Definicion de InfartoJerax PNo ratings yet
- Icu Skills Assessment ExamDocument5 pagesIcu Skills Assessment ExamJona AureNo ratings yet
- 56 MediastinumDocument6 pages56 MediastinumRahmi Dwi AzkiahNo ratings yet
- Kasus Lain LainDocument14 pagesKasus Lain LainofislinNo ratings yet
- 2018 ESC-EACTS Guidelines On Myocardial RevascularizationDocument96 pages2018 ESC-EACTS Guidelines On Myocardial RevascularizationTony Miguel Saba SabaNo ratings yet
- Basic Life Support (BLS) : Franklin O. Que, BSN-RNDocument90 pagesBasic Life Support (BLS) : Franklin O. Que, BSN-RNfrank_1785No ratings yet
- Vital Signs ProcedureDocument10 pagesVital Signs ProcedureJojebelle Kate Iyog-cabanlet100% (3)
- Nursing Care Plan - Myocardial InfarctionDocument3 pagesNursing Care Plan - Myocardial Infarctionderic80% (10)
- Circulatory System Important Questions and AnswersDocument5 pagesCirculatory System Important Questions and Answerssamhi96No ratings yet
- Pathophysiology of Heart FailureDocument38 pagesPathophysiology of Heart FailureRizqy JoeandriNo ratings yet
- Advanced Cardiac Life Support AsystoleDocument14 pagesAdvanced Cardiac Life Support AsystoleKar TwentyfiveNo ratings yet
- Kanski's Clinical Ophthalmology A Systematic Approach by John SalmonDocument20 pagesKanski's Clinical Ophthalmology A Systematic Approach by John SalmonAliNo ratings yet
- Anatomi Organ DR - Siti Rafiah HusainDocument73 pagesAnatomi Organ DR - Siti Rafiah HusainfitrahfajrianihamingNo ratings yet
- ACS Case StudyDocument26 pagesACS Case StudyMari Lyn100% (1)
- IMELS New Approach in Basic Life SupportDocument28 pagesIMELS New Approach in Basic Life SupportAstri Arri FebriantiNo ratings yet
- Rheumatic Fever and Rheumatic Heart DiseaseDocument54 pagesRheumatic Fever and Rheumatic Heart DiseaseFian AldyNo ratings yet
- Amiodarone Hydro ChlorideDocument4 pagesAmiodarone Hydro Chlorideapi-3797941No ratings yet
- Occupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesDocument2 pagesOccupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesMathea Cohen0% (1)
- Ischaemic Heart DiseaseDocument23 pagesIschaemic Heart Diseasebrain bareNo ratings yet
- Cor Pulmonale: Definition, Causes, Symptoms & TreatmentDocument31 pagesCor Pulmonale: Definition, Causes, Symptoms & TreatmentAnjela BaidyaNo ratings yet
- Nursing Care of Patient With Cardiac ArrestDocument78 pagesNursing Care of Patient With Cardiac ArrestNurhamizah Abd hamidNo ratings yet
- Cardiovascular SystemDocument6 pagesCardiovascular Systemtasneem8No ratings yet
- Clinical Cardiology - April 1994 - Wareing - Cardiac Surgery 2nd Edition by John W Kirklin and Brian G Barratt BoyesDocument1 pageClinical Cardiology - April 1994 - Wareing - Cardiac Surgery 2nd Edition by John W Kirklin and Brian G Barratt BoyesOlga KochubeiNo ratings yet
- Study This Question Med Surg FinalDocument14 pagesStudy This Question Med Surg FinalAna Gonzalez83% (6)