Professional Documents
Culture Documents
IgM Pada Thypoid
Uploaded by
ririlibertiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IgM Pada Thypoid
Uploaded by
ririlibertiCopyright:
Available Formats
Am. J. Trop. Med. Hyg., 57(6). 1997. pp.
656659
Copyright 0 1997 by The American Society of Tropical Medicine and Hygiene
LONGEVITY OF ANTIBODY RESPONSES TO A SALMONELLA TYPHI-SPECIFIC
OUTER MEMBRANE
PROTEIN: INTERPRETATION
OF A DOT ENZYME
IMMUNOSORBENT
ASSAY IN AN AREA OF HIGH TYPHOID FEVER ENDEMICITY
K. E. CHOO, T M. E. DAVIS, A. ISMAIL, ANDK. H. ONG
Department of Paediatrics and Department of Medical Microbiology
and Parasitology,
School of Medical Sciences,
Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia: Department of Medicine, Fremantle Hospital,
University of Western Australia, Fremantle, Western Australia
Abstract.
The objective of this study was to investigate the longevity of positive dot enzyme iminunosorbent
assay (dot EIA) results for 1gM and IgG to a Salmonella typhi outer membrane protein in Malaysian children with
enteric fever. The patients were children one month to 12 years of age with clinical evidence of typhoid fever, positive
blood or stool cultures for S. typhi, and/or a positive Widal test result who were admitted over a two-year period to
General Hospital (Kota Bharu, Malaysia). These patients received standard inpatient treatment for enteric fever in
cluding chloramphenicol
therapy for 14 days. Dot EIA tests were performed as part of clinical and laboratory as
sessments on admission, at two weeks, and then at 3, 6, 9, 12, 15, 18, and 21 months postdischarge.
Assessment of
the longevity of positive dot EIA 1gM and IgG titers was done by Kaplan-Meier analysis. In 94 evaluable patients,
28% were dot ELA 1gM positive but IgG negative on admission, 50% were both 1gM and IgG positive, and 22%
were 1gM negative and IgG positive. Mean persistence of 1gM dot EIA positivity was 2.6 months (95% confidence
interval = 2.03.1 months) and that of IgG was 5.4 months (4.56.3 months). There were no significant differences
between the three subgroups. Thus, positive 1gM and IgG results determined by dot EIA within four and seven
months, respectively, following documented or suspected enteric fever in a child from an endemic area should be
interpreted with caution. In other clinical situations, the dot EIA remains a rapid and reliable aid to diagnosis.
Although a positive bacterial culture remains the gold
standard for the diagnosis of typhoid fever, indirect diag
nostic tests are also in common use. The most established
of these is the Widal test, which continues to be evaluated
in field studies as an adjunct to clinical assessment and bac
terial isolation.' 2 Recently, a dot enzyme immunosorbent
as
say (dot EIA) using a 50-kD outer membrane protein (OMP)
from Salmonella typhi has been developed as a cost-effective
serologic test alternative that has the additional advantage of
providing a result within hours of blood sampling.3
The dot
EIA allows separate visual assessment of the presence of
specific IgG and 1gM antibodies to the OMP in a standard
1: 100 dilution of serum by a characteristic color change and
has been reported to be at least as specific and sensitive as
the Widal test in children with typhoid fever.5
In other infections, the kinetics of the antibody response can
vary with the infecting microorganism, the clinical state of the
patient at the time of diagnosis, and the response to treatment.
In Shigella dysentery affecting adults, for example, serum 1gM
titers peak within weeks of presentation and decrease to initial
levels after 23months, while IgG levels still are double the
initial titers at this time.6 The duration of significant 1gM titers
in Borrelia
burgdorferi
infections
can
sometimes
be
positive in Malaysian
highly endemic area.
is a function
of the clinical
features
Thus,
for different
infective
agents
typhi
or a positive
Widal
test
result
(significant
titer
1:
80)2 were eligible for recruitment. Informed consent was ob
mined from a parent or guardian of each child for partici
pation of the child in the study, including regular attendance
at outpatient assessments after discharge from the hospital.
The study was approved by the Ethical Committees of both
the Ministry of Health (Malaysia) and Universiti Sans Ma
laysia.
Methods. Clinical management of each child included mm
tial clinical assessment, routine hematologic and biochemical
tests and cultures, commencement
of rehydration either oral
ly or intravenously if required, and chioramphenicol
therapy
(administered orally, or intravenously if unable to take oral
ly, at a dose of 75 mg/kg/day) for 14 days. Blood and fecal
culture for S. typhi and the Widal test were performed as
described previously.5 Briefly, blood samples were taken us
ing aseptic technique, incubated in broth with regular sub
culture on blood agar over a period of seven days. Stool
cultures were plated on MacConkey
and deoxycholate-ci
trate agar both directly and after initial incubation in selenite
broth. Species identification in positive cultures was made
using a panel of biochemical and agglutination tests (Well
come Reagents, Kent, United Kingdom). The Widal test was
carried out using antigens obtained from Wellcome Diag
nostics (Dartford, United Kingdom) and standard serial di
lutions of serum in normal saline starting at 1:40.
Rapid serodiagnosis
was also performed at presentation
many
of the ill
and clinical
fever from a
Patients. All children between one month and 12 years
of age admitted to the Department of Paediatrics, General
Hospital (Kota Bharu, Kelantan State, Malaysia) in 1991 and
1992 with fever and positive blood or stool cultures for S.
ness.7 Persistence of Pseudomonas aeruginosa anti-lipopoly
saccharide antibodies appears to be independent of the severity
of the infection, antigemc stimulus, and initial serologic re
sponse.8
with entenc
PATIENTS AND METHODS
years, while the relationship between IgG and 1gM in the serum
at presentation
children
situa
tions, the duration of detectable specific 1gM and IgG may
vary. This may have implications for the interpretation of se
rologic test results, including the Widal test itself, in areas
where the infection is prevalent.9
To improve the interpretation of the dot EIA in the field,
we have evaluated how long 1gM and IgG test results remain
656
LONGEVITY
OF ANTIBODY
RESPONSE
657
TO S. TYPHI OMP
Percent positive
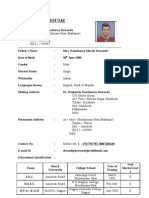
T@me 1
Details of the groups of patients classified by initial dot-enzyme
immunoassay results
Group 1
*1gM
2
Group 1
(IgM+IIgG)Group (1gM and lgG+)Group
(lgMIlgG+)Number2647Age
@l9G]
(years),21mean
3.0Sex(MIF)12/1421/2612/9Duration
3.17.5
SD8.0
2.37.1
fever(days),
of
7Blood mean SD12
culture posi
71
712
1
.5
(%)54%57%52%Widal
tive
0 antigen Ii
.5
5,'..
ter,
median1:3201:1601:80*(range)(01
1,280)(01:640)Widal
:1,280)(01 :
H antigen ti
ter,
median1:6401:3201:320(range)(1
,280)(01:1,280)a
:401
:640)(01 : 1
@
p < 0.02 versus GroupsI
Group 2
and 2.
ff@gM
lgG
St
using the dot EIA.4 Briefly, 1: 100 dilutions of patient serum
were added to standard aliquots of 0.3 @i.gof purified OMP
dotted on nitrocellulose
strips. After 1 hr. horseradish per
oxidaseconjugated antiserum to human IgG or 1gM was
added. The presence of antigen-antibody
complexes was as
sessed visually from the resultant color change in compari
son with that of positive control sera. A positive dot EIA
IgG or 1gM result was a titer of at least 1: 100 because only
one dilution was used.
Patients were hospitalized at least 14 days or until fever
clearance. Follow-up assessments,
including the dot EIA,
were scheduled at two weeks, and then at 3, 6, 9, 12, 15,
18, and 21 months postdischarge or until dot EIA results for
both 1gM and IgG were negative. Stool or rectal swab cul
tures were also taken at each assessment to identify carriers
of S. typhi.
Statistical
analysis.
Data analysis was performed
by
means of parametric statistics using the computer software
package SPSS for Windows (SPSS, Inc., Chicago, IL) and
results are given the mean and standard deviation (SD) un
less otherwise stated. Assessment of the duration of a posi
tive dot ELA result was done by Kaplan-Meier analysis and
the log-rank test was used to determine differences in mean
persistance
A two-tailed
of 1gM
and
IgG
levels
level of significance
between
patient
St
V
St
St
icx
Group 3
*1gM
lgG
80
60 e@'
St
St
St
40
5,
.5.
20
@, p
24
810
12
1416
18
20
groups.
Time (months)
was used.
FIGURE 1.
RESULTS
Of 151 children admitted during the two-year study period
with probable enteric fever, 94 (45 males and 49 females
between the ages of two and 11 years) were included in the
analysis. These 94 evaluable patients were those from whom
complete data were available for inpatient management, who
had at least one assessment after discharge, and who were
neither readmitted with typhoid fever nor had a positive stool
culture during follow-up.
On the basis of dot ELA results at the time of presentation,
patients were divided retrospectively
into one of three sub
groups. Group 1 consisted of those who were initially 1gM
positive and IgG negative, Group 2 comprised those who
were both 1gM and IgG positive on admission, and Group
Percentage
of patients
with
positive
dot enzyme
im
munosorbent assay 1gM and/or IgO results during follow-up for up
to 21 months postdischarge. Group 1 patients are those who were
only 1gM positive initially, Group 2 were both 1gM and IgO positive
at presentation,
and Group
3 had only
positive
IgO titers
on admis
sion.
3 patients were those who were 1gM negative but IgG pos
itive. Details of these groups are summarized in Table 1. The
groups had similar demographic characteristics
and features
related to typhoid fever except that those who were initially
1gM negative (Group 3) had significantly
lower Widal 0
antibody titers than those in the other two groups.
Figure 1 shows the serial changes in positivity for both
1gM and IgG antibodies by dot EIA over the period of fol
low-up. In Group 1, there was a decrease in the percentage
658
CHOO AND OTHERS
100
TABLE 2
[@Group
- Group
80
Mean survival [95% confidence intervals] in months for 1gM or IgG
antibody detected by dot-enzyme immunoassay in those patients
who were positive
A Censored
at any time during follow@up*
a)
>
positiveAll
U)
0
0.
60
1gM positive
patients2.6
lgG
5.4 [4.56.3]
(n = 82; 3 censored)
[2.03.1]
censored)Group (n = 75; 2
at
12.3
4.7 [2.96.5]
[1.63.0]
censored)Group (n = 26; 2
22.7
[1.93.4]
censored)Group (n
47; 0
3
a) 40
C.)
20
(n = 14; 0 censored)
5.8 [4.66.9]
(n = 47; 3 censored)
4.9 [3.06.81
(n = 2)
a Censored
cases
are those
who
(n = 21; 0 censored)
were
positive
initially
or during
follow-up
but defaulted
from further assessmentbefore the test results became negative.
[@Group 1
a)
>
- - Group
S..
Group
IgG antibodies (P = 0.075) with lower mean
Groups 1 and 3 compared with to Group 2.
a Censored
values
in
DISCUSSION
In
0
0.
CD
at
C
a)
C.)
a)
0.
10
12
14
16
18
20
Time (months)
FIGURE 2.
Persistence
curves
for both 1gM- and IgG-positive
dot
enzyme immunosorbent assay results grouped by initial serologic
result. Censored
quate follow-up
data are from patients who did not complete
and were excluded from persistance analysis.
ade
of patients who were 1gM positive such that all were nega
tive by six months. Less than half of this group became IgG
positive during this time and the decrease in the number of
IgG-positive cases was slower than for 1gM. This latter trend
was also observed in Group 2. In Group 3, only two patients
or just under 10% became 1gM positive during follow-up.
Persistance curves for 1gM and IgG are shown in Figure
2 and the results of Kaplan-Meier
analysis are summarized
in Table 2. Only two (2.7%) of 75 patients who tested 1gM
positive during the study defaulted from follow-up before
they became antibody negative (Figure 2). In the case of
IgG, this was the case in only three (3.7%) of 82 cases. The
mean persistance of detectable 1gM antibody in patients who
tested positive at any time during the study period was 2.6
months, with the majority of patients becoming negative
within three months of the positive result. There were no
significant differences in mean persistance value between
subgroups (P = 0.88), but because of insufficient numbers,
Group 3 was not included in analysis. For IgG, the mean
persistance of antibody positivity was approximately
twice
as long as that for 1gM (5.4 months), with most patients
becoming negative six months after initial assessment. There
was a nonsignificant
trend to shorter persistance times for
Our results indicate that in Malaysian children with en
tenc fever, the mean duration of an initially or subsequently
positive 1gM dot EIA result by persistance analysis is just
under three months postdischarge.
For IgG positivity, the
mean duration is approximately double this figure. The 95%
confidence intervals for these means approach one month on
either side. Thus, positive 1gM and IgG results within four
and seven months, respectively, of documented or suspected
enteric fever would appear to obfuscate the initial serologic
assessment of a febrile child.
Patients groups classified according to initial dot EIA 1gM
and IgG profiles did not differ in their basic demographic
and clinical features. However, it is interesting that a signif
icantly lower Widal anti-O titer was found in Group 3 chil
dren. This suggests that despite the comparable duration of
fever before presentation in the three groups, Group 3 pa
tients presented at an immunologically
later stage in their
infection
creasing
(with
Widal
a negative
1gM result by dot EIA and a de
anti-O titer) than children
in the other two
groups. Nevertheless, the duration of either 1gM or IgG test
result positivity did not appear to be influenced by the im
munologic stage at which the children presented.
In Group 1 patients who were all 1gM positive and IgG
negative
by dot
EIA
at presentation,
the development
of a
positive IgG test result occurred in less than half during fol
low-up. This may have been due partly to the sampling sched
ule, with some patients possibly exhibiting a transiently pos
itive IgG test result between assessments. However, given the
mean and 95% confidence intervals for persistance time of an
IgG response in the three groups compared with the 2.5-3month gap between samples, such a contribution would ap
pear limited. Thus, there appears to be a proportion of patients
(approximately
10% of the total series) who do not develop
IgG antibodies to the OMP as detected by the dot EIA.
Two patients in Group 3 who were initially 1gM negative
and IgG positive subsequently developed positive 1gM test
results. This could indicate that these patients had a residual
positive IgG titer from a previous episode of enteric fever
and redeveloped significant 1gM titers from the new infec
tion. Other unexpected patterns also emerged during follow
LONGEVITY
OF ANTIBODY
up in individual patients, including a transiently positive IgG
test result at 18 months in a child with a negative result three
months before and three months after this timepoint. How
ever, factors such as exposure to other Salmonella species
without the patient necessarily developing overt symptoms
of infection may influence the results of the dot EIA.
There are few studies that have prospectively
examined
aspects of humoral immunity to bacterial infections in hu
mans. Nevertheless, the longevity of detectable 1gM and IgG
antibodies by dot EIA in the present study was comparable
with that reported in bacterial infections such as Shigella
flexneri6 and Yersinia
Specific IgG antibodies
do not always develop after IgMU or may be delayed in their
appearance,12
observations
that
are
consistent
with
the
se
rologic findings in individual patients in our series.
Our data allow a better characterization
of the clinical ap
plications and limitations of the dot EIA. Where enteric fever
is uncommon, the patient has had no significant febrile ill
nesses
over
the
previous
seven
months,
and
has
suggestive
clinical features, a dot EIA can prove to be a rapid and reliable
diagnostic aid at the time of presentation. In an endemic area
and when the child has had known or possible typhoid fever
in the relatively recent past, the dot EIA result must be inter
preted with caution. Of note, comparable kinetic information
to that presented in this report is not available for the Widal
test, indicating a further potential advantage of the dot EtA
over conventional serologic diagnostic techniques.
Financial support: The study was supported by an Intensification of
Research in Priority Area grant from the Ministry of Science, Tech
nology and Environment of Malaysia.
Authors' addresses: K. E. Choo, Department of Paediatrics, School
of Medical Sciences, Hospital Universiti Sains Malaysia, Kubang
Kerian, 16150 Kelantan, Malaysia. T M. E. Davis, Department of
Medicine, Fremantle Hospital, University of Western Australia, P0
Box 480, Fremantle, Western Australia 6160. A. Ismail and K. H.
Ong, Department of Medical Microbiology and Parasitology, School
of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian,
16150 Kelantan, Malaysia.
RESPONSE
659
TO S. TYPHI OMP
Reprint requests: K. E. Choo, Depanment of Paediatrics, Hospital
Universiti Sains Malaysia, Kubang Kerian, 16150 Kelantan, Malaysia.
REFERENCES
1. Chow CB, Wang PS, Cheung MW, Yan WW, Leung NK, 1987.
Diagnostic value of the Widal test in childhood typhoid fever.
Pediatr infect Dis J 6: 914917.
2. Choo KE, Razif AR, Oppenheimer
SJ, Ariffin WA, Lau J, Abra
ham T, 1993. Usefulness of the Widal test in diagnosing
childhood
typhoid
fever in endemic
areas.
J Paediatr
Child
Health 29: 3639.
3. Ismail A, Ong KH, Kader ZA, 1991. Demonstration
of an an
tigenic protein specific for Salmonella typhi. Biochem Bio
phys Res Commun /81: 301305.
4. Ismail A, Kader ZS, Ong KH, 1991. Dot enzyme
immunosor
bent assay for the serodiagnosis of typhoid fever. Southeast
Asian J Trop Med Public Health 22: 563566.
5. Choo KB, Oppenheimer SJ, Ismail AB, Ong KH, 1994. Rapid
serodiagnosis
in an endemic
of typhoid
fever
area. Clin inftct
by dot enzyme
immunoassay
Dis 19: 172176.
6. Cohen D, Block C, Green MS. Lowell 0, Ofek I, 1989. Im
munoglobulin M, A, and 0 antibody response to lipopolysac
charide 0 antigen in symptomatic and asymptomatic Shigella
infections. J Clin Microbiol 27: 162167.
7. Hammers-Berggren
5, Lebech
AM, Karisson
M, Svenungsson
B, Hansen K, Stiernstedt 0, 1994. Serological follow-up after
treatment of patients with erythema migrans and neurobor
reliosis. J Clin Microbiol 32: 15191525.
8. Petras 0, Adam MM, 1987. Phases of the serological response
in Pseudomonas aeruginosa infections. Acta Microbiol Hung
34: 147157.
9. Schroeder SA, 1968. Interpretation of serologic tests for typhoid
fever. JAMA 206: 839840.
10. Granfors K, Viljanen M, Tillikainen A, Toivanen A, 1980. Per
sistence of 1gM, IgG, and IgA antibodies to Yersinia in Yer
sinia arthritis.
J infect Dis 141: 424429.
11. Elgh F, Wadell 0, Juto P. 1995. Comparison of the kinetics of
Puumala virus specific 1gM and 1gM antibody responses in
nephropathia
epidemica
as measured
by a recombinant
anti
gen-based enzyme-linked immunosorbent assay and an im
munofluorescence test. J Med Virol 45: 148150.
12. Kalish RA, Leong JM, Steere AC, 1995. Early and late antibody
responses to full-length and truncated constructs of outer sur
face protein A of Borrelia
immun 63: 22282235.
burgdoiferi
in Lyme disease.
infect
You might also like
- Wilderness Trails Zoo Coloring Activity BookDocument24 pagesWilderness Trails Zoo Coloring Activity BookHolly Crews100% (2)
- Arctic Animals FreebieDocument8 pagesArctic Animals FreebieBahiyyih Sayyah100% (1)
- The Respiratory Tract in Pediatric Critical CareDocument258 pagesThe Respiratory Tract in Pediatric Critical CareririlibertiNo ratings yet
- Arabic Hebrew Greek Study SheetDocument75 pagesArabic Hebrew Greek Study SheetAnonymous 7QjNuvoCpINo ratings yet
- Level 2 English 2018Document21 pagesLevel 2 English 2018Bá PhongNo ratings yet
- 500 Most Frequently Used Words CompleteDocument6 pages500 Most Frequently Used Words CompleteFrank Haynes JrNo ratings yet
- 4 Oral Cavity ProceduresDocument10 pages4 Oral Cavity ProceduresAnne MarieNo ratings yet
- Food Poisoning Final Print!Document3 pagesFood Poisoning Final Print!Joeven HilarioNo ratings yet
- Digestive System of The FrogDocument73 pagesDigestive System of The FrogNi Ki TaNo ratings yet
- Diving Physiology: Fakhri Mubarok 1510211033Document23 pagesDiving Physiology: Fakhri Mubarok 1510211033Hafizh Zaki IrsyadNo ratings yet
- Sheep DiseasesDocument20 pagesSheep DiseaseselkaiatNo ratings yet
- Case Studies in Pediatric Infectious Diseases PDFDocument399 pagesCase Studies in Pediatric Infectious Diseases PDFririliberti100% (3)
- Typhoid WidalDocument4 pagesTyphoid WidalamaliamldNo ratings yet
- Pattern of Changes in Liver Enzymes SGPT, SGOT Level During Dengue Infection in Hospitalized Pediatrics Patients in Tertiary Care CentreDocument4 pagesPattern of Changes in Liver Enzymes SGPT, SGOT Level During Dengue Infection in Hospitalized Pediatrics Patients in Tertiary Care CentreGrace CastilloNo ratings yet
- Antigen-Specific Proliferation and Interferon-γ and Interleukin-5 Production Are Down-Regulated during Schistosoma haematobium Infection PDFDocument5 pagesAntigen-Specific Proliferation and Interferon-γ and Interleukin-5 Production Are Down-Regulated during Schistosoma haematobium Infection PDFGabriel CoutoNo ratings yet
- The Study of Egg Allergy in Children With Atopic DermatitisDocument5 pagesThe Study of Egg Allergy in Children With Atopic DermatitisranifebNo ratings yet
- TJI-58070 (0) Tam Metin-Revizyon GerçekleştirilmişDocument10 pagesTJI-58070 (0) Tam Metin-Revizyon GerçekleştirilmişcerraheminNo ratings yet
- Original Article: Clinical and Laboratory Features of Typhoid Fever in ChildhoodDocument6 pagesOriginal Article: Clinical and Laboratory Features of Typhoid Fever in ChildhoodRidha Surya NugrahaNo ratings yet
- Clinical Efficacy and Safety of Meropenem in The Treatment of Severe Neonatal Bacterial Infectious PneumoniaDocument6 pagesClinical Efficacy and Safety of Meropenem in The Treatment of Severe Neonatal Bacterial Infectious PneumoniaI Made AryanaNo ratings yet
- Jurnal 2Document12 pagesJurnal 2zingioNo ratings yet
- IJP - Volume 5 - Issue 12 - Pages 6189-6194Document6 pagesIJP - Volume 5 - Issue 12 - Pages 6189-6194Yupie Faming JayaNo ratings yet
- Jurnal Respi - Comparison of IGRA AssayDocument5 pagesJurnal Respi - Comparison of IGRA AssaykaynabilNo ratings yet
- 21-0965-Persisten of IgG in Children After CovidDocument7 pages21-0965-Persisten of IgG in Children After CovidERIE YUWITA SARINo ratings yet
- Typhi-Specific Igm Antibodies and The Evolution of The ImmuneDocument6 pagesTyphi-Specific Igm Antibodies and The Evolution of The ImmunefrankyNo ratings yet
- Effects of Acute Critical Illnesses On The Performance of Interferongamma Release AssayDocument9 pagesEffects of Acute Critical Illnesses On The Performance of Interferongamma Release Assayt45tz5hfsfNo ratings yet
- jm000170 PDFDocument5 pagesjm000170 PDFArista Prima NNo ratings yet
- Comparative Study of Typhidot-M With Widal and Blood Culture in Diagnosis of Enteric FeverDocument4 pagesComparative Study of Typhidot-M With Widal and Blood Culture in Diagnosis of Enteric FeverPranay BhosaleNo ratings yet
- Assessment of Serum Levels of Immunoglobulin A and Immunoglobulin G Inchildren Newly Diagnosed With Type 1 Diabetes MelDocument5 pagesAssessment of Serum Levels of Immunoglobulin A and Immunoglobulin G Inchildren Newly Diagnosed With Type 1 Diabetes MelYuniarNo ratings yet
- OriginalarticleDocument5 pagesOriginalarticledjebrutNo ratings yet
- Milk Oral Immunotherapy Is Effective in School-Aged ChildrenDocument6 pagesMilk Oral Immunotherapy Is Effective in School-Aged ChildrenAnry UmarNo ratings yet
- Schatz 2018Document44 pagesSchatz 2018abhijeet abhijeetNo ratings yet
- Efikasi AzitromisinDocument4 pagesEfikasi AzitromisinNadia DesiNo ratings yet
- Efficacy+of+IgM+Rich+Immunoglobin+for+Bacterial+Sepsis (Case Control)Document6 pagesEfficacy+of+IgM+Rich+Immunoglobin+for+Bacterial+Sepsis (Case Control)Tristiani UtariNo ratings yet
- 12 Dengue Seroprevalence ComparisonDocument4 pages12 Dengue Seroprevalence ComparisonYipno Wanhar El MawardiNo ratings yet
- Cow Milk AllergyDocument12 pagesCow Milk AllergyAbi ArifiNo ratings yet
- Anticuerpos para RNDocument2 pagesAnticuerpos para RNEliana TorresNo ratings yet
- Clinical Presentation and Laboratory Features in Pediatric Typhoid Fever Patient Susceptibility To First-Line Antibiotic TherapyDocument10 pagesClinical Presentation and Laboratory Features in Pediatric Typhoid Fever Patient Susceptibility To First-Line Antibiotic TherapySuci ZahraniNo ratings yet
- Serum Iga, Igm, and Igg Responses in Covid-19: Cellular & Molecular ImmunologyDocument3 pagesSerum Iga, Igm, and Igg Responses in Covid-19: Cellular & Molecular ImmunologynpidasNo ratings yet
- Safety and Preliminary Efficacy On Cognitive Performance and Ada 2022 GenetiDocument10 pagesSafety and Preliminary Efficacy On Cognitive Performance and Ada 2022 Genetironaldquezada038No ratings yet
- Journal Read ChiaDocument14 pagesJournal Read ChiaChris Tine ChiaNo ratings yet
- Age Specific References For IgDDocument8 pagesAge Specific References For IgDBassem AhmedNo ratings yet
- TGF-b1 Genotype in Pediatric Migraine PatientsDocument5 pagesTGF-b1 Genotype in Pediatric Migraine PatientsMinerva StanciuNo ratings yet
- Circulating Interleukin-6 and Tumor Necrosis Factor Receptor-1 Predict Resistance To Therapy of Typhoidal SalmonellosisDocument5 pagesCirculating Interleukin-6 and Tumor Necrosis Factor Receptor-1 Predict Resistance To Therapy of Typhoidal SalmonellosisAndri YansyahNo ratings yet
- IgM IgG PDFDocument5 pagesIgM IgG PDFAndri AffandiNo ratings yet
- Kjped 60 77Document9 pagesKjped 60 77Labontu IustinaNo ratings yet
- Nutrients 10 01678Document11 pagesNutrients 10 01678zulfa nadiaNo ratings yet
- Retrospective Audit of The Widal Test For Diagnosis of Typhoid Fever in Pediatric Patients in An Endemic RegionDocument4 pagesRetrospective Audit of The Widal Test For Diagnosis of Typhoid Fever in Pediatric Patients in An Endemic RegionKiagus Mahendra EffendyNo ratings yet
- Common Cold JournalDocument5 pagesCommon Cold JournalJuwita PratiwiNo ratings yet
- Office-Based Point of Care Testing (Iga/Igg-Deamidated Gliadin Peptide) For Celiac DiseaseDocument9 pagesOffice-Based Point of Care Testing (Iga/Igg-Deamidated Gliadin Peptide) For Celiac DiseasemarcosNo ratings yet
- Diagnostics 12 00453Document15 pagesDiagnostics 12 00453Fabiola Vania FeliciaNo ratings yet
- Cow S Milk Allergic ChildrenDocument12 pagesCow S Milk Allergic ChildrenNurul Huda KowitaNo ratings yet
- Typhoid Blood Test ReportDocument3 pagesTyphoid Blood Test ReportPranay BhosaleNo ratings yet
- Probiotics in The Prevention of Eczema A Randomised Controlled Trial 2014 Archives of Disease in ChildhoodDocument7 pagesProbiotics in The Prevention of Eczema A Randomised Controlled Trial 2014 Archives of Disease in ChildhoodThiago TartariNo ratings yet
- Jurnal RdsDocument6 pagesJurnal RdsNaman KhalidNo ratings yet
- Comparison of The Reliability of 17 Celiac DiseaseDocument9 pagesComparison of The Reliability of 17 Celiac Diseasesiddhi divekarNo ratings yet
- Diagnosing TB Infection in Children: Analysis of Discordances Using in Vitro Tests and The Tuberculin Skin TestDocument9 pagesDiagnosing TB Infection in Children: Analysis of Discordances Using in Vitro Tests and The Tuberculin Skin TestAri Julian SaputraNo ratings yet
- New Schatz2018 OldDocument44 pagesNew Schatz2018 Oldabhijeet abhijeetNo ratings yet
- Differential Regulation of Igg Subclasses and Ige Antimalarial Antibody Responses in Complicated and Uncomplicated MalariaDocument9 pagesDifferential Regulation of Igg Subclasses and Ige Antimalarial Antibody Responses in Complicated and Uncomplicated MalariaJarwoto RoestanajieNo ratings yet
- Art ThiDocument5 pagesArt ThiLINA ESTRADA DUQUENo ratings yet
- An Early Evaluation On The Usefulness of NS1 Antigen-Capture ELISA Versus IGM ELISA TEST For The Diagnosis of Acute Dengue InfectionDocument10 pagesAn Early Evaluation On The Usefulness of NS1 Antigen-Capture ELISA Versus IGM ELISA TEST For The Diagnosis of Acute Dengue Infectionkurniawan naryoNo ratings yet
- Streptococcus Pneumoniae Carriage, Resistance and Serotypes Among Jordanian Children From Wadi Al Seer District, JordanDocument8 pagesStreptococcus Pneumoniae Carriage, Resistance and Serotypes Among Jordanian Children From Wadi Al Seer District, JordanInternational Medical PublisherNo ratings yet
- 153303-Article Text-401385-1-10-20170317Document10 pages153303-Article Text-401385-1-10-20170317Umar Farouq Mohammed GalibNo ratings yet
- ExcelenteDocument6 pagesExcelenteRicardo ColomaNo ratings yet
- Weil-Felix Test in Diagnosis of ScrubDocument3 pagesWeil-Felix Test in Diagnosis of ScrubvyasakandarpNo ratings yet
- A Comparative Study of Typhidot and Widal Test For Rapid Diagnosis of Typhoid FeverDocument5 pagesA Comparative Study of Typhidot and Widal Test For Rapid Diagnosis of Typhoid FeverArbusa86No ratings yet
- Igg and Igm Western Blot Assay For Diagnosis of Congenital ToxoplasmosisDocument5 pagesIgg and Igm Western Blot Assay For Diagnosis of Congenital ToxoplasmosisWilliam Bunga DatuNo ratings yet
- Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiDocument6 pagesPaediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiharnizaNo ratings yet
- Article On DengueDocument6 pagesArticle On Dengueاحمد احمدNo ratings yet
- New Schatz2018Document44 pagesNew Schatz2018abhijeet abhijeetNo ratings yet
- Typhoid JournalDocument7 pagesTyphoid JournalRegina AyediaNo ratings yet
- Long Term Persistence of Ige Anti-Influenza Virus Antibodies in Pediatric and Adult Serum Post Vaccination With Influenza Virus VaccineDocument6 pagesLong Term Persistence of Ige Anti-Influenza Virus Antibodies in Pediatric and Adult Serum Post Vaccination With Influenza Virus VaccineDesti EryaniNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Bronchiolitis: Hilliard Pediatrics - Dr. Tim Teller, M.D. - 9/10Document2 pagesBronchiolitis: Hilliard Pediatrics - Dr. Tim Teller, M.D. - 9/10ririlibertiNo ratings yet
- Iron Therapy For Preterm Infants PDFDocument16 pagesIron Therapy For Preterm Infants PDFririlibertiNo ratings yet
- Hydration in Infants and Children: Vanessa ShawDocument35 pagesHydration in Infants and Children: Vanessa ShawDonya GholamiNo ratings yet
- Teofilin VS SalbutamolDocument3 pagesTeofilin VS SalbutamolririlibertiNo ratings yet
- A Review On Vitamin D Deficiency Treatment in Pediatric PatientsDocument15 pagesA Review On Vitamin D Deficiency Treatment in Pediatric PatientsAsose TuNo ratings yet
- The Reproducibility of The Jaw Index in The Measurement of Healthy NewbornsDocument7 pagesThe Reproducibility of The Jaw Index in The Measurement of Healthy NewbornsririlibertiNo ratings yet
- Enhanced Theraphy Hemofilia ADocument8 pagesEnhanced Theraphy Hemofilia AririlibertiNo ratings yet
- Etiology of Abdominal Pain in Dengue FeverDocument5 pagesEtiology of Abdominal Pain in Dengue FeverririlibertiNo ratings yet
- STEPS Abdominal MassesDocument30 pagesSTEPS Abdominal MassesririlibertiNo ratings yet
- Biology - Manual of Allergy and Immunology - Diagnosis and Therapy, 4th EdDocument206 pagesBiology - Manual of Allergy and Immunology - Diagnosis and Therapy, 4th Edgandalf il grigio100% (1)
- Joosten 2010 Malnutrition in Pediatric Hospital Patients Current IssuesDocument5 pagesJoosten 2010 Malnutrition in Pediatric Hospital Patients Current IssuesPutri Wulan SukmawatiNo ratings yet
- Pediatric Solid TumorsDocument43 pagesPediatric Solid Tumorsririliberti100% (1)
- Childhood LeukemiaDocument55 pagesChildhood LeukemiaririlibertiNo ratings yet
- HB E AnakDocument2 pagesHB E AnakririlibertiNo ratings yet
- ESBL OkDocument12 pagesESBL OkririlibertiNo ratings yet
- Hemosiderin Is An Endogenous BloodDocument4 pagesHemosiderin Is An Endogenous BloodririlibertiNo ratings yet
- CDC Responds To ZIKADocument56 pagesCDC Responds To ZIKAririlibertiNo ratings yet
- 795 1027 1 PBDocument10 pages795 1027 1 PBRatri Abdatush SholihahNo ratings yet
- 795 1027 1 PBDocument10 pages795 1027 1 PBRatri Abdatush SholihahNo ratings yet
- Sandip Namdeorao Dawande ResumeDocument4 pagesSandip Namdeorao Dawande Resume95021No ratings yet
- HSB QA What Is DigestionDocument37 pagesHSB QA What Is DigestionVivienne WrightNo ratings yet
- Simple Garter Stitch Slippers v2Document3 pagesSimple Garter Stitch Slippers v2sylviacristinariveraNo ratings yet
- Integumentary Lab ActDocument5 pagesIntegumentary Lab ActJASMINE LAURONNo ratings yet
- Clearwater Creek Controlled Use AreaDocument1 pageClearwater Creek Controlled Use AreaJeremy DvorakNo ratings yet
- Neuritis in Morbus HansenDocument32 pagesNeuritis in Morbus HansenSiska IxchaNo ratings yet
- Monterey Bay Aquarium Seafood Watch Sushi GuideDocument1 pageMonterey Bay Aquarium Seafood Watch Sushi GuideMarikoNo ratings yet
- Breeding TetrasDocument5 pagesBreeding Tetraskevs29No ratings yet
- Gait CycleDocument1 pageGait CycleLakshita PrajapatiNo ratings yet
- T L 4010 Correct The Sentence Punctuation Activity Sheets Phase 23 Ver 4Document4 pagesT L 4010 Correct The Sentence Punctuation Activity Sheets Phase 23 Ver 4eda yıldırımNo ratings yet
- Trung tâm Luyện thi Amax - 39 LK 6A Làng Việt Kiều Châu ÂuDocument11 pagesTrung tâm Luyện thi Amax - 39 LK 6A Làng Việt Kiều Châu ÂuKiều Anh NguyễnNo ratings yet
- Cargill SummaryDocument19 pagesCargill SummaryNISREEN WAYA100% (1)
- Mrs Bixby and The Colonel S CoatDocument9 pagesMrs Bixby and The Colonel S CoatHst GonzalesNo ratings yet
- Cell ModificationsDocument8 pagesCell ModificationsOreeyoNo ratings yet
- DR Gargi Singh - 2 Page Notes - NeuralDocument9 pagesDR Gargi Singh - 2 Page Notes - NeuralSuccessfactors TrainerNo ratings yet
- 2023 CBSE I Succeed Eng. Lang. Lit. K. A. Zone Poetry SectionDocument9 pages2023 CBSE I Succeed Eng. Lang. Lit. K. A. Zone Poetry SectioniCOS iSpace100% (1)
- PREP OF PLACE WorksheetDocument1 pagePREP OF PLACE WorksheetAnnaNo ratings yet
- Gupta 2018Document6 pagesGupta 2018franklinNo ratings yet
- Third Periodical Test in English IvDocument1 pageThird Periodical Test in English IvRuby GonzalesNo ratings yet
- Minggu 1 Amali PengenalanDocument36 pagesMinggu 1 Amali PengenalanAtiq NadzirahNo ratings yet