Professional Documents
Culture Documents
Perio Heart PDF
Uploaded by
Rahadian RamadhanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Perio Heart PDF
Uploaded by
Rahadian RamadhanCopyright:
Available Formats
Periodontal infections and cardiovascular
disease
The heart of the matter
Ryan T. Demmer, PhD; Mose Desvarieux, MD, PhD
fter two decades of
A ABSTRACT A D
research, it has been J
A
firmly established that
an association exists Background. Oral infection models have emerged
N
CON
between periodontal
IO
as useful tools to study the hypothesis that infection is
T
disease and cardiovascular disease
T
a cardiovascular disease (CVD) risk factor. Periodontal
A
N
I
U C
U
(CVD). The pertinent question, infections are a leading culprit, with studies reporting A ING ED 2
RT
however, is about the nature and associations between periodontal disease and CVD. The ICLE
relevance of this association. results, however, have varied, and it often is unclear what conclusions can
Specifically, does the infectious be drawn from these data.
and inflammatory periodontal dis- Summary. An association exists between periodontal disease and CVD. It
ease process contribute causally to is unknown, however, whether this relationship is causal or coincidental.
heart attacks and strokes, or are Early studies predominantly used nonspecific clinical and radiographic defi-
these two conditions coincidentally nitions of periodontal disease as surrogates for infectious exposure. While
associated? most studies demonstrated positive associations between periodontal dis-
Although the evidence of a ease and CVD, not all studies were positive, and substantial variations in
potentially contributory role of results were evident. More recent studies have enhanced the specificity of
periodontal infections in the nat- infectious exposure definitions by measuring systemic antibodies to selected
ural history of CVD continues to periodontal pathogens or by directly measuring and quantifying oral micro-
mount, there are well-founded rea- biota from subgingival dental plaque. Results from these studies have shown
sons for skepticism. With this in positive associations between periodontal disease and CVD.
mind, we provide a state-of-the- Conclusions. Evidence continues to support an association among peri-
science article regarding the asso- odontal infections, atherosclerosis and vascular disease. Ongoing observa-
ciation between periodontal dis- tional and focused pilot intervention studies may inform the design of large-
ease and CVD. scale clinical intervention studies. Recommending periodontal treatment for
the prevention of atherosclerotic CVD is not warranted based on scientific
TRADITIONAL STUDIES OF evidence. Periodontal treatment must be recommended on the basis of the
PERIODONTAL DISEASE AND
CARDIOVASCULAR DISEASE value of its benefits for the oral health of patients, recognizing that patients
are not healthy without good oral health. However, the emergence of peri-
In 1989, two Scandinavian reports odontal infections as a potential risk factor for CVD is leading to a conver-
revived a century-old hypothesis gence in oral and medical care that can only benefit the patients and public
relating chronic infections with health.
vascular disease that originally Key Words. Cardiovascular; infection; periodontitis; epidemiology.
was proposed by French and JADA 2006;137(10 supplement):14S-20S.
German scientists.1 Mattila and
colleagues2 found higher combined Dr. Demmer is a postdoctoral research scientist, Department of Epidemiology, Mailman School of Public
levels of caries, periodontitis, peri- Health, Columbia University, New York City.
apical lesions and pericoronitis (all Dr. Desvarieux is a faculty member, Department of Epidemiology, Mailman School of Public Health,
Columbia University, New York City; chair of excellence, Unit Mixte de Recherche, Site 707, Institut
serving as surrogate markers of National de la Sant et de la Recherche Mdicale, Universit Pierre et Marie Curie-Paris. Address reprint
oral infections) more frequently in requests to Dr. Desvarieux at Department of Epidemiology, Mailman School of Public Health, Columbia
patients with recent myocardial University, 722 W. 168th St., Suite 1704, New York, N.Y. 10032, e-mail md108@columbia.edu.
14S JADA, Vol. 137 http://jada.ada.org October 2006
Copyright 2006 American Dental Association. All rights reserved.
infarction than in healthy control patients from smoking status, dietary patterns, race/ethnicity,
the same population. Syrjanen and colleagues3 education and socioeconomic status.7-11,13 These
observed relatively poor oral health among results have particular importance in the case of
patients who had experienced a recent stroke smoking, as some have postulated that the asso-
compared with control patients who had not ciation between periodontal disease and CVD is
experienced stroke. due to smoking-related bias.14 While smoking
These authors drew careful conclusions, pri- status was assessed in most studies, the level of
marily because of the substantial overlap noted adjustment varied, with some studies providing a
between risk factors for both periodontal disease more detailed smoking assessment. For example,
and CVDbeing older, being male, cigarette Morrison and colleagues10 observed that partici-
smoking, diabetes and low socioeconomic status. pants with periodontal disease had more risk of
If periodontal disease and CVD simply share developing fatal coronary heart disease and expe-
common risk factors, a correlation between the riencing stroke even after controlling for smoking
two would be expected even if a causal link did status by classifying current smokers according to
not exist. This epidemiologic phenomenon is the number of cigarettes smoked per day. Others
referred to as confounding.4 have controlled for smoking by restricting their
These studies enrolled patients when they analyses to never-smokers. Joshipura and col-
came to a hospital with a heart leagues13 reported an 80 percent
attack or stroke, which meant that elevation in stroke risk for people
measures of oral health were taken Most studies reported with zero to 24 teeth compared with
after the cardiovascular event had positive associations those who had 25 or more teeth
occurred, raising the possibility between periodontal among never-smokers. Desvarieux
that the cardiovascular event might disease and and colleagues15 reported similar
have influenced oral health nega- cardiovascular disease findings between tooth loss and
tively. The geographical homo- carotid atherosclerosis, unmodified
after accounting for
geneity and small number of par- by smoking status. Nevertheless,
ticipants enrolled in these studies the effects of multiple underlying the confounding by
precluded any reliable generaliza- risk factors such as smoking argument is the possi-
tions beyond the specific study age, sex, diabetes, bility of a healthy bias effect, in
population. cholesterol levels, which people who smoke are more
Subsequently, studies addressing blood pressure, likely to have unhealthy lifestyles,
many of these limitations have which can lead to both periodontal
obesity, smoking
made substantial contributions to disease and CVD.
our understanding of periodontal status, dietary Grau and colleagues16 provide
disease and CVD associations. 5,6 patterns, race/ important information concerning
These studies collectively included ethnicity, education the specificity of the hypothesis to
more than 100,000 adult men and and socioeconomic periodontal disease; they reported a
women from diverse populations, status. 400 percent increase in stroke risk
which has enhanced the consistency associated with periodontitis but
and generalizability of the proposed found no relationship between
association between periodontal disease and caries and stroke. The specificity of these findings
CVD. Because many of these studies were to periodontal disease argues against a healthy
prospective or retrospective,7-13 the assessment of lifestyle bias in which people with poor oral
periodontal disease often was done before the health practices, which can lead to both caries
occurrence of cardiovascular events, thus better and periodontal disease, also would be less likely
establishing the temporality of the association. to engage in behaviors related to cardiovascular
Several authors also rigorously tested whether health.
periodontal disease was associated with CVD Not all studies have found a positive relation-
independent of risk factors common to both con- ship between periodontal disease and CVD.
ditions. Specifically, most studies reported posi- Reports from the Health Professionals Follow-Up
tive associations after accounting for the effects Study17 and the Physicians Health Study18
of multiple risk factors such as age, sex, diabetes, observed no association between periodontal dis-
cholesterol levels, blood pressure, obesity, ease and either coronary heart disease or stroke
JADA, Vol. 137 http://jada.ada.org October 2006 15S
Copyright 2006 American Dental Association. All rights reserved.
among more than 66,000 male health profes- lative exposure to periodontal infections is not
sionals. The large sample sizes of these two meaningfully different between edentulous
studies provide a good reason for caution with patients and those with periodontitis.15 Reports
regard to the overall hypothesis. However, a from the Oral Infections and Vascular Disease
major limitation of these studies stems from the Epidemiology Study (INVEST) and the Study of
self-report nature of periodontal disease assess- Health in Pomerania (SHIP) demonstrated that in
ment in which participants were asked via ques- both U.S. and German cohorts, participants with
tionnaire whether they had a history of peri- more tooth loss had more clinical periodontal dis-
odontal disease as opposed to receiving an ease, suggesting that periodontal disease might
in-person clinical examination.17,18 have been an important reason for tooth loss.15,22
Hujoel and colleagues19 found no association Furthermore, data from INVEST15,23 and SHIP22
between periodontal disease and coronary heart suggest that edentulous people remain at an ele-
disease in the First National Health and Nutri- vated or a potentially intermediate risk of devel-
tion Examination Survey (NHANES I) cohort. oping subclinical CVD. Consequently, it is pos-
Among younger participants (younger than 55 sible that the potential risk from periodontal
years), however, there was an approximately 50 to infections might not be reversible after a certain
80 percent increased risk of developing coronary threshold of subclinical CVD has developed.
heart disease associated with periodontitis.5,19 Reports from the United States11 and Ger-
Although subgroup results of this nature are sus- many16,23 have provided evidence that the associa-
ceptible to chance findings, these results are con- tion between periodontal disease and CVD might
sistent with the findings of Janket and colleagues5 be stronger among men than among women. The
and Mattila and colleagues,20 which suggest that possibility that novel risk factors might partly
periodontal disease might pose a stronger risk for explain some of the sex differential in CVD risk is
CVD among younger participants. intriguing.23 For example, in SHIP, Desvarieux
Interestingly, two of the studies reporting no and colleagues22 reported that men had more
association between periodontal disease and coro- severe periodontal disease than did women,
nary disease are at odds with stroke findings from raising the possibility that women did not reach a
the same population. Wu and colleagues11 found threshold of inflammation necessary for systemic
strong positive associations between periodontal effects.
disease and stroke in the same NHANES popula- In summary, research supports a moderate rel-
tion in which Hujoel and colleagues21 reported no ative association between CVD and periodontal
relationship between periodontal disease and coro- disease assessed clinically and radiographically.5,6
nary disease. Joshipura and colleagues reported This relationship appears to be more pronounced
no association between periodontal disease and in younger participants, possibly different in male
coronary disease,17 but they did find a positive and female subjects and consistently stronger for
association for stroke13 in the same cohort. These clinical stroke outcomes. Although the existence of
discrepancies are consistent with the literature, some null publications provides reason for cau-
which indicates that periodontal disease might be tion, these studies were based on self-reported
a stronger risk factor for cerebrovascular disease periodontal disease status, contradicted by other
than for coronary disease.5 analyses of the same dataset or potentially
In another report, Hujoel and colleagues21 explained by threshold effects. Nevertheless, sub-
reported that edentulous participants did not stantial variation in results among studies is
have a lower coronary heart disease risk com- apparent. A likely explanation for this variation is
pared with dentate participants with periodon- the nonspecificity of clinically or radiographically
titis. While these data could be interpreted as defined exposures used by traditional studies.
arguing against an association between vascular New research designed to measure oral infection
disease and periodontal disease, other explana- exposure more directly is needed.
tions should be considered. Indeed, while total
tooth extraction prevents exposure to periodontal NOVEL RESEARCH APPROACHES TO REFINE
AND TEST MORE SPECIFIC HYPOTHESES
infection, it does not remove the history of expo-
sure. For example, in populations in which tooth The study of periodontal disease and CVD asso-
loss primarily is due to periodontal disease, this ciations has its roots in the broader hypothesis
may lead to an apparent paradox in which cumu- concerning infections and CVD. Therefore, recent
16S JADA, Vol. 137 http://jada.ada.org October 2006
Copyright 2006 American Dental Association. All rights reserved.
research has provided new insights by obtaining levels of the periodontal bacteria, after adjust-
more precise measures of exposure to periodontal ment for traditional risk factors. This relationship
microbes, incorporating outcome measures of sub- with atherosclerosis was specific for the four peri-
clinical CVD or both. odontal etiologic bacteria. No relationship was
Systemic antibody titers. Moving away from found between increased atherosclerosis and the
the earlier studies linking clinical and radiologic group of control bacteria, diminishing the likeli-
periodontal disease with vascular disease, hood of an unhealthy lifestyle bias. These results
Pussinen and colleagues24,25 reported that ele- constitute the most direct evidence to date of a
vated antibodies to selected periodontal possible contributory role of periodontal infections
pathogens were associated with an increased to atherosclerosis. However, while these findings
prevalence of coronary heart disease, increased are novel, they also are cross-sectional; thus, we
atherosclerosis in the carotid artery and more must await prospective results to determine
risk of developing coronary events during 10 whether oral microorganisms are associated with
years of follow-up. In a separate cohort, they atherosclerotic progression that will translate into
reported more risk of experiencing stroke asso- clinical events in this cohort.
ciated with elevated antibody titers.26 Both Recently, Spahr and colleagues33 provided evi-
studies were conducted in European populations. dence that these subclinical effects might be
In a U.S. cohort, Beck and colleagues27,28 translated into clinical coronary disease. They
reported that increased systemic directly assessed the periodontal
antibody levels to periodontal pathogen burden and found that an
microbes are related to an increased Carotid increased pathogen burden was
prevalence of coronary heart disease atherosclerosis as related positively to the presence of
and subclinical atherosclerosis. measured by clinical coronary heart disease.
Although these findings are not intima-media Subclinical intervention
prospective, they are consistent with studies. We are aware of three
thickening increased
previous findings that demonstrated intervention studies that have
an association between clinical peri- with higher levels assessed the impact of periodontal
odontal disease and atherosclerosis of the periodontal treatment on subclinical markers of
in the same population.29 These find- bacteria. CVD.34-36 Each reported that peri-
ings also are of interest because odontal treatment was associated
they show a relationship between with improved measures of sys-
antibody titers and coronary heart temic inflammation or subclinical
disease even among never-smokers, providing CVD. While these findings are novel and support
further evidence that the observed relationship is potential cardiovascular benefits from periodontal
not simply a result of smoking-induced bias. treatment, some important limitations should be
Direct measurement of oral microbiology. noted. First, these interventions were not ran-
An even more direct approach to assessing expo- domized, and they lacked an untreated control
sure to periodontal microbes is to measure bac- group of subjects with periodontal disease.
teria quantitatively in periodontal plaque sam- Second, oral infection was not measured directly
ples, a procedure that has not been undertaken at baseline and follow-up to address the contribu-
frequently in large samples because of the sub- tions of oral microbiology to these findings.
stantial undertaking and costs. INVEST Finally, these studies included small numbers of
researchers analyzed nearly 5,000 subgingival participants, and researchers were unable to
plaque samples in 657 dentate participants for determine if these subclinical findings translated
quantification of 11 known periodontal bacteria, into fewer clinical cardiovascular events.
including four (Actinobacillus actinomycetem-
comitans, Porphyromonas gingivalis, Tannerella MECHANISMS BY WHICH
PERIODONTITIS MAY RELATE TO
forsythensis and Treponima denticola) defined a CARDIOVASCULAR DISEASE
priori as being related etiologically to periodontal
disease30,31 and seven other bacterial species A number of reviews have been published that
acting as controls. Desvarieux and colleagues32 outline potential biological mechanisms linking
reported that carotid atherosclerosis as measured infections and periodontal disease to CVD
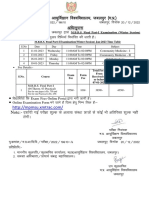
by intima-media thickening increased with higher (Figure).37-40 We provide an overview of the
JADA, Vol. 137 http://jada.ada.org October 2006 17S
Copyright 2006 American Dental Association. All rights reserved.
ated early atherosclerosis
Microbes among infected mice. Gia-
cona and colleagues50 found
Direct Invasion
Indirect that certain strains of
Circulation P. gingivalis are capable of
Endotoxin
Vascular Injury infecting macrophages and
Cytokines
enhancing foam cell forma-
Abnormal Lipid Profile Inflammation
tion in the vascular wall,
LDL Cytokines
HDL Tissue Growth Factors adding further credence to
Triglycerides LDL and Oxidized LDL in Macrophages
P. gingivalis ability to ini-
Atherosclerosis tiate or exacerbate the ath-
Procoagulant Environment erosclerotic process.
Activation of Coagulation Cascade
Finally, in vitro studies
Platelet Aggregation
Thrombomodulin
Factor X Activation demonstrated the ability of
Thrombosis Streptococcus sanguis and
P. gingivalis to induce
platelet aggregation and
Vulnerable Plaque hypercoagulability,
increasing the likelihood of
thrombus formation, which
can lead to ischemic cardio-
Ischemia
vascular events.51-54
Indirect pathways.
Figure. Example of a potential mechanism of infectious agents in atherosclerosis. LDL: Low-density
lipoprotein. HDL: High-density lipoprotein. Source: Fong.37 Atherosclerosis has a
strong inflammatory com-
leading biological hypotheses. ponent,55,56 and epidemiologic evidence suggests
Direct pathways. Oral microbes and their that increased levels of systemic inflammation are
byproducts can gain systemic access via the circu- predictive of cardiovascular events.57,58
41
latory system. Geerts and colleagues showed People with periodontal disease have elevated
that gentle mastication can induce endotoxemia, levels of systemic inflammatory markers, such as
and this risk was elevated according to an C-reactive protein,59-63 and treatment for peri-
increased severity of periodontal disease. Kinane odontal disease has been reported to decrease sys-
and colleagues,42 Rajasuo and colleagues,43 temic inflammation levels.64 There are many
44 45
Roberts and Forner and colleagues have shown potential triggers for this enhanced systemic
that dental procedures and toothbrushing can inflammatory response, including transient bac-
induce bacteremias. Recent research indicates teremias and the local release of bacterial by-
that the magnitude of bacteremia after scaling products such as lipopolysaccharide.34,65
was amplified among patients with periodontitis Another plausible mechanism connecting oral
as opposed to patients with gingivitis or healthy infection and CVD is molecular mimicry, in which
control patients.45 Studies of carotid endarterec- antibodies targeted toward bacterial (including
tomy samples have found common periodontal periodontal) species inadvertently cross-react with
pathogens from arterial plaques.46,47 In gaining host cells. For example, heat shock protein 60 has
systemic access, oral microbes have the potential been studied for its potential role in mediating
to directly influence subclinical mediators of infection-induced atherosclerosis, as human and
cardiovascular events such as hypercoagulability, bacterial heat shock proteins 60 are conserved
atherosclerotic development or both. highly.66 These instances of mistaken identity
A mice study demonstrated that intravenous could lead to vascular inflammation and
inoculation with P. gingivalis accelerates athero- atherosclerosis.
sclerotic development.48 Lalla and colleagues49
induced periodontal infection via oral inoculation CONCLUSION
with P. gingivalis and were later able to recover At a minimum, periodontal infections are epi-
P. gingivalis DNA from the aortic tissue of demiologically associated with CVD; that is, peri-
infected mice only and observe signs of acceler- odontal infections seem to be found more fre-
18S JADA, Vol. 137 http://jada.ada.org October 2006
Copyright 2006 American Dental Association. All rights reserved.
quently in patients with CVD. However, the crit- of periodontal infections as a possible risk factor
ical question of whether periodontal infections are for CVD is leading to a convergence in oral and
a risk factor for or contribute causally to CVD and medical care. As dental, public health and medical
cerebrovascular disease remains unanswered. researchers and practitioners reach across disci-
The possibility that periodontal disease and CVD plines, a holistic approach to care can only benefit
share common risk factors or are manifestations the patients and public health as a whole.
of a similar underlying pathology remains, as sev-
eral analyses were conducted post hoc and statis- This work was supported by National Institute of Dental and Cranio-
facial Research grant R01 DE 13094 and Projet ANR R05115DD from
tical adjustment for confounders can be imperfect. the French Agency for Research.
However, the mounting evidence points to an
association of periodontal disease at the bio- 1. Nieto FJ. Infections and atherosclerosis: new clues from an old
hypothesis? Am J Epidemiol 1998;148(10):937-48.
logical, clinical, radiographic and microbiological 2. Mattila KJ, Nieminen MS, Valtonen VV, et al. Association between
levels in relation to clinical and subclinical vas- dental health and acute myocardial infarction. BMJ 1989;298(6676):
779-81.
cular disease. Because periodontal infections are 3. Syrjanen J, Peltola J, Valtonen V, Iivanainen M, Kaste M, Hut-
so prevalent, the potential attributable risk of tunen JK. Dental infections in association with cerebral infarction in
young and middle-aged men. J Intern Med 1989;225(3):179-84.
such an association would be substantial at the 4. Rothman KJ, Greenland S. Modern epidemiology. Philadelphia:
population level. There is, however, no direct Lippincott-Raven; 1998:62.
5. Janket SJ, Baird AE, Chuang SK, Jones JA. Meta-analysis of peri-
peer-reviewed evidence to suggest that treating or odontal disease and risk of coronary heart disease and stroke. Oral
preventing periodontal infections leads to fewer Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95(5):559-69.
6. Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis, and
clinical cardiovascular events. Some insurance cardiovascular disease. Crit Rev Oral Biol Med 2004;15(6):403-13.
company studies, however, find fewer medical 7. DeStefano F, Anda RF, Kahn HS, Williamson DF, Russell CM.
Dental disease and risk of coronary heart disease and mortality. BMJ
care needs in patients who maintain their peri- 1993;306(6879):688-91.
odontal health. If the relationship holds, one of 8. Beck J, Garcia R, Heiss G, Vokonas PS, Offenbacher S. Periodontal
disease and cardiovascular disease. J Periodontol 1996;67(supplement
the remaining issues will be to determine 10):1123-37.
whether the possible contribution of periodontal 9. Mattila KJ, Valtonen VV, Nieminen M, Huttunen JK. Dental infec-
tion and the risk of new coronary events: prospective study of patients
disease to CVD risk can be addressed better via with documented coronary artery disease. Clin Infect Dis 1995;20(3):
treatment of existing disease or through preven- 588-92.
10. Morrison HI, Ellison LF, Taylor GW. Periodontal disease and risk
tion before a threshold of irreversible subclinical of fatal coronary heart and cerebrovascular diseases. J Cardiovasc Risk
CVD is reached. 1999;6(1):7-11.
11. Wu T, Trevisan M, Genco RJ, Dorn JP, Falkner KL, Sempos CT.
It will be necessary to conduct large-scale ran- Periodontal disease and risk of cerebrovascular disease: the first
domized intervention trials designed specifically national health and nutrition examination survey and its follow-up
study. Arch Intern Med 2000;160(18):2749-55.
to test these questions. Before valid and pow- 12. Jansson L, Lavstedt S, Frithiof L, Theobald H. Relationship
eredlarge and costlyclinical intervention between oral health and mortality in cardiovascular diseases. J Clin
Periodontol 2001;28(8):762-8.
trials can be organized, it is important to obtain 13. Joshipura KJ, Hung HC, Rimm EB, Willett WC, Ascherio A.
the results of ongoing national and international Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke
2003;34(1):47-52.
observational research studies and new mecha- 14. Hujoel PP, Drangsholt M, Spiekerman C, DeRouen TA.
nistic or intermediate trials testing focused Periodontitis-systemic disease associations in the presence of smoking:
causal or coincidental? Periodontol 2000 2002;30:51-60.
hypotheses. Results from these studies will help 15. Desvarieux M, Demmer RT, Rundek T, et al. Relationship
inform future intervention designs by answering between periodontal disease, tooth loss, and carotid artery plaque: the
Oral Infections and Vascular Disease Epidemiology Study (INVEST).
questions regarding such topics as optimal expo- Stroke 2003;34(9):2120-5.
sure definitions, treatment targets and optimal 16. Grau AJ, Becher H, Ziegler CM, et al. Periodontal disease as a
risk factor for ischemic stroke. Stroke 2004;35(2):496-501.
windows of intervention, mechanisms of disease, 17. Joshipura KJ, Rimm EB, Douglass CW, Trichopoulos D, Ascherio
appropriate biological markers and appropriate A, Willett WC. Poor oral health and coronary heart disease. J Dent Res
1996;75(9):1631-6.
populations in which to conduct interventions. 18. Howell TH, Ridker PM, Ajani UA, Hennekens CH, Christen WG.
Recommending periodontal treatment solely Periodontal disease and risk of subsequent cardiovascular disease in
U.S. male physicians. J Am Coll Cardiol 2001;37(2):445-50.
for the purpose of atherosclerotic CVD prevention 19. Hujoel PP, Drangsholt M, Spiekerman C, DeRouen TA. Peri-
is not warranted based on current scientific evi- odontal disease and coronary heart disease risk. JAMA 2000;284(11):
1406-10.
dence. Periodontal treatment must be recom- 20. Mattila KJ, Asikainen S, Wolf J, Jousimies-Somer H, Valtonen V,
mended on the basis of the value of its benefits for Nieminen M. Age, dental infections, and coronary heart disease. J Dent
Res 2000;79(2):756-60.
the oral health of patients, recognizing that 21. Hujoel PP, Drangsholt M, Spiekerman C, Derouen TA. Examining
patients are not healthy without good oral health the link between coronary heart disease and the elimination of chronic
dental infections. JADA 2001;132(7):883-9.
and taking into account American Heart Associa- 22. Desvarieux M, Schwahn C, Volzke H, et al. Gender differences in
tion recommendations.67 However, the emergence the relationship between periodontal disease, tooth loss, and atheroscle-
JADA, Vol. 137 http://jada.ada.org October 2006 19S
Copyright 2006 American Dental Association. All rights reserved.
rosis. Stroke 2004;35(9):2029-35. periodontal inflammation. J Clin Periodontol 2006;33(6):401-7.
23. Engebretson SP, Lamster IB, Elkind MS, et al. Radiographic 46. Haraszthy VI, Zambon JJ, Trevisan M, Zeid M, Genco RJ. Identi-
measures of chronic periodontitis and carotid artery plaque. Stroke fication of periodontal pathogens in atheromatous plaques. J Peri-
2005;36(3):561-6. odontol 2000;71(10):1554-60.
24. Pussinen PJ, Alfthan G, Tuomilehto J, Asikainen S, Jousilahti P. 47. Chiu B. Multiple infections in carotid atherosclerotic plaques. Am
High serum antibody levels to Porphyromonas gingivalis predict Heart J 1999;138(5 part 2):S534-6.
myocardial infarction. Eur J Cardiovasc Prev Rehabil 2004;11(5): 48. Li L, Messas E, Batista EL Jr, Levine RA, Amar S. Porphy-
408-11. romonas gingivalis infection accelerates the progression of atheroscle-
25. Pussinen PJ, Nyyssonen K, Alfthan G, Salonen R, Laukkanen rosis in a heterozygous apolipoprotein E-deficient murine model. Circu-
JA, Salonen JT. Serum antibody levels to Actinobacillus actino- lation 2002;105(7):861-7.
mycetemcomitans predict the risk for coronary heart disease. 49. Lalla E, Lamster IB, Hofmann MA, et al. Oral infection with a
Arterioscler Thromb Vasc Biol 2005;25(4):833-8. periodontal pathogen accelerates early atherosclerosis in apolipoprotein
26. Pussinen PJ, Alfthan G, Rissanen H, Reunanen A, Asikainen S, E-null mice. Arterioscler Thromb Vasc Biol 2003;23(8):1405-11.
Knekt P. Antibodies to periodontal pathogens and stroke risk. Stroke 50. Giacona MB, Papapanou PN, Lamster IB, et al. Porphyromonas
2004;35(9):2020-3. gingivalis induces its uptake by human macrophages and promotes
27. Beck JD, Eke P, Heiss G,. Periodontal disease and coronary heart foam cell formation in vitro. FEMS Microbiol Lett 2004;241(1):95-101.
disease: a reappraisal of the exposure. Circulation 2005;112(1):19-24. 51. Herzberg MC, Meyer MW. Effects of oral flora on platelets: pos-
28. Beck JD, Eke P, Lin D, et al. Associations between IgG antibody sible consequences in cardiovascular disease. J Periodontol 1996;
to oral organisms and carotid intima-medial thickness in community- 67(supplement 10):1138-42.
dwelling adults. Atherosclerosis 2005;183(2):342-8. 52. Meyer MW, Gong K, Herzberg MC. Streptococcus sanguis-induced
29. Beck JD, Elter JR, Heiss G, Couper D, Mauriello SM, Offen- platelet clotting in rabbits and hemodynamic and cardiopulmonary con-
bacher S. Relationship of periodontal disease to carotid artery intima- sequences. Infect Immun 1998;66(12):5906-14.
media wall thickness: the Atherosclerosis Risk In Communities (ARIC) 53. Fong IW. Emerging relations between infectious diseases and
study. Arterioscler Thromb Vasc Biol 2001;21(11):1816-22. coronary artery disease and atherosclerosis. CMAJ 2000;163(1):49-56.
30. Consensus report: periodontal diseasespathogenesis and micro- 54. Imamura T, Potempa J, Tanase S, Travis J. Activation of blood
bial factors. Ann Periodontol 1996;1(1):926-32. coagulation factor X by arginine-specific cysteine proteinases (gingi-
31. Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL Jr. pain-Rs) from Porphyromonas gingivalis. J Biol Chem 1997;272(25):
Microbial complexes in subgingival plaque. J Clin Periodontol 16062-7.
1998;25(2):134-44. 55. Ross R. Atherosclerosis is an inflammatory disease. Am Heart J
32. Desvarieux M, Demmer RT, Rundek T, et al. Periodontal micro- 1999;138(5 part 2):S419-20.
biota and carotid intima-media thickness: the Oral Infections and Vas- 56. Libby P. Coronary artery injury and the biology of atherosclerosis:
cular Disease Epidemiology Study (INVEST). Circulation 2005;111(5): inflammation, thrombosis, and stabilization. Am J Cardiol 2000;86(8B):
576-82. 3J-9J.
33. Spahr A, Klein E, Khuseyinova N, et al. Periodontal infections 57. Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH.
and coronary heart disease: role of periodontal bacteria and impor- Inflammation, aspirin, and the risk of cardiovascular disease in appar-
tance of total pathogen burden in the Coronary Event and Periodontal ently healthy men (published correction in N Engl J Med 1997;337[5]:
Disease (CORODONT) study. Arch Intern Med 2006;166(5):554-9. 356). N Engl J Med 1997;336(14):973-9.
34. Elter JR, Hinderliter AL, Offenbacher S, et al. The effects of peri- 58. Ridker PM, Rifai N, Stampfer MJ, Hennekens CH. Plasma con-
odontal therapy on vascular endothelial function: a pilot trial. Am centration of interleukin-6 and the risk of future myocardial infarction
Heart J 2006;151(1):47. among apparently healthy men. Circulation 2000;101(15):1767-72.
35. Mercanoglu F, Oflaz H, Oz O, et al. Endothelial dysfunction in 59. Slade GD, Ghezzi EM, Heiss G, Beck JD, Riche E, Offenbacher S.
patients with chronic periodontitis and its improvement after initial Relationship between periodontal disease and C-reactive protein among
periodontal therapy. J Periodontol 2004;75(12):1694-700. adults in the Atherosclerosis Risk in Communities study. Arch Intern
36. Seinost G, Wimmer G, Skerget M, et al. Periodontal treatment Med 2003;163(10):1172-9.
improves endothelial dysfunction in patients with severe periodontitis. 60. Slade GD, Offenbacher S, Beck JD, Heiss G, Pankow JS. Acute-
Am Heart J 2005;149(6):1050-4. phase inflammatory response to periodontal disease in the US popula-
37. Fong IW. Infections and their role in atherosclerotic vascular dis- tion. J Dent Res 2000;79(1):49-57.
ease. JADA 2002;133(supplement):7S-13S. 61. Loos BG, Craandijk J, Hoek FJ, Wertheim-van Dillen PM, van der
38. OConnor S, Taylor C, Campbell LA, Epstein S, Libby P. Poten- Velden U. Elevation of systemic markers related to cardiovascular dis-
tial infectious etiologies of atherosclerosis: a multifactorial perspective. eases in the peripheral blood of periodontitis patients. J Periodontol
Emerg Infect Dis 2001;7(5):780-8. 2000;71(10):1528-34.
39. Beck JD, Pankow J, Tyroler HA, Offenbacher S. Dental infections 62. Ebersole JL, Machen RL, Steffen MJ, Willmann DE. Systemic
and atherosclerosis. Am Heart J 1999;138(5 part 2):S528-33. acute-phase reactants, C-reactive protein and haptoglobin, in adult
40. Li X, Kolltveit KM, Tronstad L, Olsen I. Systemic diseases caused periodontitis. Clin Exp Immunol 1997;107(2):347-52.
by oral infection. Clin Microbiol Rev 2000;13(4):547-58. 63. Kowolik MJ, Dowsett SA, Rodriguez J, De La Rosa RM, Eckert
41. Geerts SO, Nys M, De MP, et al. Systemic release of endotoxins GJ. Systemic neutrophil response resulting from dental plaque accumu-
induced by gentle mastication: association with periodontitis severity. lation. J Periodontol 2001;72(2):146-51.
J Periodontol 2002;73(1):73-8. 64. DAiuto F, Parkar M, Andreou G, et al. Periodontitis and systemic
42. Kinane DF, Riggio MP, Walker KF, MacKenzie D, Shearer B. inflammation: control of the local infection is associated with a reduc-
Bacteraemia following periodontal procedures. J Clin Periodontol tion in serum inflammatory markers. J Dent Res 2004;83(2):156-60.
2005;32(7):708-13. 65. Mahanonda R, Sa-Ard-Iam N, Charatkulangkun O. Monocyte
43. Rajasuo A, Nyfors S, Kanervo A, Jousimies-Somer H, Lindqvist activation by Porphyromonas gingivalis LPS in aggressive periodontitis
C, Suuronen R. Bacteremia after plate removal and tooth extraction. with the use of whole-blood cultures. J Dent Res 2004;83(2):540-5.
Int J Oral Maxillofac Surg 2004;33(4):356-60. 66. Ford P, Gemmell E, Walker P, West M, Cullinan M, Seymour G.
44. Roberts GJ. Dentists are innocent! Everyday bacteremia is the Characterization of heat shock protein-specific T cells in atheroscle-
real culprita review and assessment of the evidence that dental sur- rosis. Clin Diagn Lab Immunol 2005;12(2):259-67.
gical procedures are a principal cause of bacterial endocarditis in chil- 67. Dajani AS, Taubert KA, Wilson W, et al. Prevention of bacterial
dren. Pediatr Cardiol 1999;20(5):317-25. endocarditis: recommendations by the American Heart Association.
45. Forner L, Larsen T, Kilian M, Holmstrup P. Incidence of bac- Circulation 1997;96(1):358-66.
teremia after chewing, tooth brushing and scaling in individuals with
20S JADA, Vol. 137 http://jada.ada.org October 2006
Copyright 2006 American Dental Association. All rights reserved.
You might also like
- Pile Foundation As Per IRC 112Document59 pagesPile Foundation As Per IRC 112ARVIND SINGH RAWAT0% (1)
- FAT Form Winch UnitDocument7 pagesFAT Form Winch UnitYadi KusmayadiNo ratings yet
- Periodontitis and Atherosclerotic Cardiovascular DiseaseDocument3 pagesPeriodontitis and Atherosclerotic Cardiovascular DiseaseHuỳnh Bảo Anh NguyênNo ratings yet
- Periodontitis y Enfermedad CardiovascularDocument8 pagesPeriodontitis y Enfermedad CardiovascularDafne MendozaNo ratings yet
- Atherosclerosis 2Document6 pagesAtherosclerosis 2Gustivanny Dwipa AsriNo ratings yet
- iej.12710Document13 pagesiej.12710oanaNo ratings yet
- Periodontal Disease and Diabetes: A Two-Way StreetDocument6 pagesPeriodontal Disease and Diabetes: A Two-Way StreetywdNo ratings yet
- Is Gum Disease Killing Your Patient?: R. A. SeymourDocument2 pagesIs Gum Disease Killing Your Patient?: R. A. SeymourhanyNo ratings yet
- Increasing Evidence For An Association Between Periodontitis and Cardiovascular DiseaseDocument3 pagesIncreasing Evidence For An Association Between Periodontitis and Cardiovascular DiseaseIrsyadNo ratings yet
- PEAK Is There A Link Between Periodontitis and Cardiovascular Disease PDFDocument12 pagesPEAK Is There A Link Between Periodontitis and Cardiovascular Disease PDFYama Piniel FrimantamaNo ratings yet
- Enfermedad PeriodontalDocument5 pagesEnfermedad PeriodontalLuisa Fernanda Gil MartinezNo ratings yet
- Chen 2015Document6 pagesChen 2015nurminsyahNo ratings yet
- Diabetes Mellitus As A Modulating Factor of Endodontic InfectionsDocument10 pagesDiabetes Mellitus As A Modulating Factor of Endodontic InfectionsDiana SitepuNo ratings yet
- Cardiovascular Risks Associated With Incident and Prevalent Periodontal DiseaseDocument8 pagesCardiovascular Risks Associated With Incident and Prevalent Periodontal DiseaseAlyaefkageNo ratings yet
- Journal of Periodontology - 2020 - Beck - Periodontal Disease Classifications and Incident Coronary Heart Disease in TheDocument10 pagesJournal of Periodontology - 2020 - Beck - Periodontal Disease Classifications and Incident Coronary Heart Disease in TheSung Soon ChangNo ratings yet
- 10 1002@cre2 336Document14 pages10 1002@cre2 336Sung Soon ChangNo ratings yet
- Int Endodontic J - 2021 - Sebring - Endodontic Inflammatory Disease A Risk Indicator For A First Myocardial InfarctionDocument12 pagesInt Endodontic J - 2021 - Sebring - Endodontic Inflammatory Disease A Risk Indicator For A First Myocardial InfarctionIrzam PratamaNo ratings yet
- Hepatitis B Virus Transmissions Associated With ADocument9 pagesHepatitis B Virus Transmissions Associated With AAyesha Nasir KhanNo ratings yet
- Periodontitis and Systemic Disease: BDJ Team November 2015Document5 pagesPeriodontitis and Systemic Disease: BDJ Team November 2015Jenea CapsamunNo ratings yet
- Fimmu 13 915081Document15 pagesFimmu 13 915081Zakia MaharaniNo ratings yet
- FRAMMINGHAM1605794700Characterization of Cardiovascular Risk Factors and Framingham Score in An HIV 1 Population-1Document4 pagesFRAMMINGHAM1605794700Characterization of Cardiovascular Risk Factors and Framingham Score in An HIV 1 Population-1Asry AinunNo ratings yet
- Instructions: Oral Health and Systemic DiseaseDocument4 pagesInstructions: Oral Health and Systemic Diseaselove tripNo ratings yet
- Remisión A Medico Chan - Et - Al-2017-Periodontology - 2000Document6 pagesRemisión A Medico Chan - Et - Al-2017-Periodontology - 2000Jesus FandiñoNo ratings yet
- Pediatric Appendicitis Imaging During COVID Shows Higher RatesDocument9 pagesPediatric Appendicitis Imaging During COVID Shows Higher RatesDokter GamingNo ratings yet
- Ren 2018Document7 pagesRen 2018atikahanifahNo ratings yet
- Kuo 2017Document35 pagesKuo 2017regarskidNo ratings yet
- Endodontics and Diabetes: Association Versus CausationDocument13 pagesEndodontics and Diabetes: Association Versus CausationGaby GarciaNo ratings yet
- Periodontitis and Systemic Disease: FeatureDocument4 pagesPeriodontitis and Systemic Disease: Featurewendyjemmy8gmailcomNo ratings yet
- Journal of Diabetes and Its ComplicationsDocument7 pagesJournal of Diabetes and Its ComplicationsOanna ChippNo ratings yet
- Chen 2012Document8 pagesChen 2012MEHERNo ratings yet
- 10 1002@lary 29336Document6 pages10 1002@lary 29336Novia KurniantiNo ratings yet
- jada.archive.2006.0403Document7 pagesjada.archive.2006.0403mapecorelli2626No ratings yet
- Sistemico EndoDocument20 pagesSistemico EndoAlexandre SallesNo ratings yet
- The Evidence Base For The Efficacy of Antibiotic Prophylaxis in Dental PracticeDocument17 pagesThe Evidence Base For The Efficacy of Antibiotic Prophylaxis in Dental PracticebmNo ratings yet
- Arya 17 1 2362Document8 pagesArya 17 1 2362oanaNo ratings yet
- Association of Vitamin D in Patients With Periodontitis: A Cross-Sectional StudyDocument12 pagesAssociation of Vitamin D in Patients With Periodontitis: A Cross-Sectional Studyimam rifaiNo ratings yet
- Comparative Clinical Study On Periodontal Health SDocument20 pagesComparative Clinical Study On Periodontal Health Spennyshevlin1No ratings yet
- JPER.20-0607Document8 pagesJPER.20-0607oanaNo ratings yet
- Cross Sectional AnalyticDocument6 pagesCross Sectional AnalyticSitti Monica A. AmbonNo ratings yet
- COVID-19 and Thrombotic or Thromboembolic Disease: Implications For Prevention, Antithrombotic Therapy, and Follow-UpDocument24 pagesCOVID-19 and Thrombotic or Thromboembolic Disease: Implications For Prevention, Antithrombotic Therapy, and Follow-UpDr. RajibNo ratings yet
- Artigo PeriodontiaDocument7 pagesArtigo PeriodontiaDANIELA MARTINS LEITENo ratings yet
- Periodontitis Increases The Risk of Respiratory Disease Mortality in OlderDocument5 pagesPeriodontitis Increases The Risk of Respiratory Disease Mortality in OlderJavier Ramos GascaNo ratings yet
- 1 s2.0 S0939475322004616 MainDocument8 pages1 s2.0 S0939475322004616 MainSalvia Elvaretta HarefaNo ratings yet
- Pharmaceuticals 15 01146 v2Document26 pagesPharmaceuticals 15 01146 v2Norlando RuizNo ratings yet
- Pulpal Inflammation and Incidence of Coronary Heart Disease Joshipura 2006Document5 pagesPulpal Inflammation and Incidence of Coronary Heart Disease Joshipura 2006Jing XueNo ratings yet
- N E W S: Periodontitis, Tongue Cancer LinkedDocument2 pagesN E W S: Periodontitis, Tongue Cancer LinkedRendiNo ratings yet
- Fulltext - Ajr v8 Id1153Document1 pageFulltext - Ajr v8 Id1153sarhang talebaniNo ratings yet
- 3.casual or Causal Relationship Between Periodontal Infection and Non Oral DiseaseDocument3 pages3.casual or Causal Relationship Between Periodontal Infection and Non Oral DiseaseEstherNo ratings yet
- Prolonged Breastfeeding Is Associated With Lower.30Document3 pagesProlonged Breastfeeding Is Associated With Lower.30ingridspulerNo ratings yet
- 2.prevalence and Impact of - Myocardial InjuryDocument14 pages2.prevalence and Impact of - Myocardial Injuryrest_a2003No ratings yet
- Periodontitis y Covid 19 Traduci RsDocument20 pagesPeriodontitis y Covid 19 Traduci RsALEXANDROV JOSMELNo ratings yet
- Cardiovascular Disease and The Role of Oral BacteriaDocument14 pagesCardiovascular Disease and The Role of Oral BacteriaOdonto BrunaNo ratings yet
- Periodontal Disease, Edentulism, and Pancreatic Cancer: A Meta-AnalysisDocument11 pagesPeriodontal Disease, Edentulism, and Pancreatic Cancer: A Meta-AnalysisSmaranda GavrilNo ratings yet
- Diabetes Mellitus - Considerations For DentistryDocument11 pagesDiabetes Mellitus - Considerations For DentistryJaime Ruiz Jr.No ratings yet
- Bidirectional AssociationDocument10 pagesBidirectional AssociationAndrea MorenoNo ratings yet
- Dental and Periodontal Disease in Patients With Inflammatory Bowel DiseaseDocument8 pagesDental and Periodontal Disease in Patients With Inflammatory Bowel DiseasemulooNo ratings yet
- 906 2757 1 PB 2 PDFDocument19 pages906 2757 1 PB 2 PDFReza Fachrial SyaifulNo ratings yet
- Sinusitis and Pneumonia Hospitalization After Introduction of Pneumococcal Conjugate VaccineDocument11 pagesSinusitis and Pneumonia Hospitalization After Introduction of Pneumococcal Conjugate VaccineHanida Rahmah TaminNo ratings yet
- Periodontitis and Diabetes Mellitus: EditorialDocument3 pagesPeriodontitis and Diabetes Mellitus: EditorialNovita ApramadhaNo ratings yet
- 1 s2.0 S1473309916000268 MainDocument12 pages1 s2.0 S1473309916000268 MainLachlan PetersonNo ratings yet
- Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19Document9 pagesPulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19Riandhani UpitariniaNo ratings yet
- Optimize soil preparation with a versatile mini tillerDocument2 pagesOptimize soil preparation with a versatile mini tillerRickson Viahul Rayan C100% (1)
- Shavuot 5774Document4 pagesShavuot 5774Andrea KingNo ratings yet
- Household Chemical Poisoning GuideDocument9 pagesHousehold Chemical Poisoning GuideAshley DayagNo ratings yet
- RL Procedure Hard Natural Rubber PT - SURYA SAKTI SUKSESDocument7 pagesRL Procedure Hard Natural Rubber PT - SURYA SAKTI SUKSESMuhammad ZakiNo ratings yet
- wk4 Stdconferencereflection ElmoreajaDocument4 pageswk4 Stdconferencereflection Elmoreajaapi-316378224No ratings yet
- 803 Service ManualDocument196 pages803 Service Manualвася рогов100% (1)
- Grade 3 Science: PlantsDocument5 pagesGrade 3 Science: PlantsMauie Flores100% (3)
- Boge Screw UsaDocument40 pagesBoge Screw UsaAir Repair, LLC100% (1)
- TDDDocument4 pagesTDDJay VibhaniNo ratings yet
- MBBS Final Part-I (Winter Session) Time Table (Jan 2023)Document1 pageMBBS Final Part-I (Winter Session) Time Table (Jan 2023)crystal mindNo ratings yet
- High Flyers / Answer Key G / Unit 4: GrammarDocument8 pagesHigh Flyers / Answer Key G / Unit 4: GrammarDian Novyta AriantiNo ratings yet
- Study To Assess The Effectiveness of Planned Teaching Programme Regarding Knowledge of Traffic Rules Among Higher Secondary Students 15 18 Years in Selected Schools of DehradunDocument14 pagesStudy To Assess The Effectiveness of Planned Teaching Programme Regarding Knowledge of Traffic Rules Among Higher Secondary Students 15 18 Years in Selected Schools of DehradunEditor IJTSRDNo ratings yet
- E1cc E3ccDocument219 pagesE1cc E3ccSARAMQRNo ratings yet
- Treating and Preventing Ear Infections in ChildrenDocument4 pagesTreating and Preventing Ear Infections in ChildrenbehrangNo ratings yet
- Manual NSD70D EnglishDocument155 pagesManual NSD70D Englishnarvis1No ratings yet
- English Dept Guidebook: Grammar & Exercises for Level 4Document57 pagesEnglish Dept Guidebook: Grammar & Exercises for Level 4KIngLyonLuis100% (1)
- 1.4 Market FailureDocument42 pages1.4 Market FailureRuban PaulNo ratings yet
- Derm CodingDocument8 pagesDerm CodingVinay100% (1)
- PDI Quality Manual Rev 4 - 1.0 Table of ContentsDocument1 pagePDI Quality Manual Rev 4 - 1.0 Table of ContentslouieNo ratings yet
- CCE Format For Class 1 To 8Document5 pagesCCE Format For Class 1 To 8Manish KaliaNo ratings yet
- Non-Directive Counselling RogersDocument5 pagesNon-Directive Counselling RogersSanjeev ChaudharyNo ratings yet
- Medical TourismDocument18 pagesMedical TourismdhnaushNo ratings yet
- Adapted Sports & Recreation 2015: The FCPS Parent Resource CenterDocument31 pagesAdapted Sports & Recreation 2015: The FCPS Parent Resource CenterkirthanasriNo ratings yet
- Concept of Health and IllnessDocument24 pagesConcept of Health and IllnessHydra Olivar - Pantilgan100% (1)
- MANUAL Health O Meter Scale 800KLDocument2 pagesMANUAL Health O Meter Scale 800KLElkin MaldonadoNo ratings yet
- Product and Service Costing: Job-Order System: Questions For Writing and DiscussionDocument22 pagesProduct and Service Costing: Job-Order System: Questions For Writing and Discussionsetiani putriNo ratings yet
- Caffeine's Effect on Daphnia Heart RateDocument2 pagesCaffeine's Effect on Daphnia Heart RateMianto NamikazeNo ratings yet
- Sir PapsDocument15 pagesSir PapsRey Niño GarciaNo ratings yet