Professional Documents
Culture Documents
Jurnal Anak Ririn
Uploaded by
Dexter BluesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal Anak Ririn
Uploaded by
Dexter BluesCopyright:
Available Formats
Original Article
Nasal High-Flow Therapy for
Primary Respiratory Support in
Preterm
Calum Infants
T. Roberts, M.B., Ch.B., Louise S. Owen, M.D., Brett J. Manley, Ph.D.,
Dag H. Frisland, Ph.D., Susan M. Donath, M.A., Kim M. Dalziel, Ph.D., Margo
A. Pritchard, Ph.D., David W. Cartwright, M.B., B.S., Clare L. Collins, M.D.,
Atul Malhotra, M.D., and Peter G. Davis, M.D., for the HIPSTER Trial
Investigators*
ABSTRACT
From Neonatal Services and Newborn BACKGROUND
Research Centre, Royal Womens Hospi Treatment with nasal high-flow therapy has efficacy similar to that of
- tal (C.T.R., L.S.O., B.J.M., D.H.F.,
nasal con- tinuous positive airway pressure (CPAP) when used as
P.G.D.), the Departments of Obstetrics
and Gyn - aecology (C.T.R., L.S.O., postextubation support in neonates. The efficacy of high-flow therapy
B.J.M., P.G.D.) and Paediatrics (S.M.D.) as the primary means of respiratory support for preterm infants with
and School of Population and Global respiratory distress has not been proved.
Health (K.M.D.), University of
Melbourne, Critical Care and METHODS
Neurosciences (L.S.O., P.G.D.) and In this international, multicenter, randomized, noninferiority trial, we
Clinical Epidemiology and Biostatistics assigned 564 preterm infants (gestational age, =28 weeks 0 days) with
Unit (S.M.D.), Murdoch Childrens Re - early respiratory distress who had not received surfactant replacement
search Institute, Neonatal Services,
Mercy Hospital for Women (C.L.C.), and to treatment with either nasal high-flow therapy or nasal CPAP. The
Monash Newborn, Monash Childrens primary outcome was treatment failure within 72 hours after
Hospital, and Department of Paediatrics, randomization. Noninferiority was determined by calculat- ing the
Monash University (A.M.), Melbourne,
VIC, and the School of Nursing,
absolute difference in the risk of the primary outcome; the chosen
Midwifery and Paramedicine, Australianmargin of noninferiority was 10 percentage points. Infants in whom
Catholic Uni - versity (M.A.P.), Mater high-flow therapy failed could receive rescue CPAP; infants in whom
Research Institute (M.A.P.) and the CPAP failed were intubated and mechanically ventilated.
Department of Paediat - rics (D.W.C.),
University of Queensland, and Womens RESULTS
and Newborn Services, Royal BrisbaneTrial recruitment stopped early at the recommendation of the
and Womens Hospital (D.W.C.), independent data and safety monitoring committee because of a
Brisbane, QLD all in Austra - lia; and
the Department of Pediatrics, Innlandet
significant difference in the pri- mary outcome between treatment
Hospital Trust, Lillehammer, Norway groups. Treatment failure occurred in 71 of 278 infants (25.5%) in the
(D.H.F.). Address reprint requests to Dr.high-flow group and in 38 of 286 infants (13.3%) in the CPAP group
Owen at the Newborn Research Cen - (risk difference, 12.3 percentage points; 95% confidence interval [CI],
tre, Level 7, Royal Womens Hospital,
* A complete
Locked list ofParkville,
Bag 300, investigators in the 5.8 to 18.7; P<0.001). The rate of intubation within 72 hours did not
VIC 3052,
High
Austra Flow
- lia,Nasal
or at Cannulae as Primary differ sig- nificantly between the high-flow and CPAP groups (15.5%
louise . owen@
Support
thewomens in the Treatment
. org . au. of Early Respiand
- 11.5%, respec- tively; risk difference, 3.9 percentage points; 95%
ratory Distress (HIPSTER) Trial is pro-
vided in the Supplementary Appendix, CI, -1.7 to 9.6; P = 0.17), nor did the rate of adverse events.
available at NEJM.org. CONCLUSION
Drs. Roberts and Owen contributed S
When used as primary support for preterm infants with respiratory
equal - ly to this article.
distress, high- flow therapy resulted in a significantly higher rate of
N E n g l J M e d 2 0 16 ; 37
5 : 11 4 2 - 51 . D O I: 10 . 10 treatment failure than did CPAP. (Funded by the National Health and
56/NEJMoa16
Copyright 20160Massachusetts
369 4 Medical Medical Research Council and others; Australian New Zealand Clinical
Society.
Trials Registry number, ACTRN12613000303741.)
1142 n engl j med 375;12 nejm.org September 22, 2016
Nasal High-Flow Therapy in Preterm
Infants
I n 2014, there were more than 380,000
preterm births (i.e., births at a gestational
age of <37 weeks) in the United States, Study Design and Oversight
account-
Preterm ing for approximately
infants have a risk of 10%
Methods
the of all1 Nine neonatal intensive care units in
births that year.
respiratory distress syndrome. The Australia and Norway participated in the
introduction of endotra- cheal ventilation study. The hu- man research ethics
has improved the survival rate among committee at each partici- pating center
preterm infants but is associated with an approved the study. All authors vouch for
increased risk of complications such as the accuracy and completeness of the
broncho- pulmonary 2 dysplasia. data
and isand for the fidelity
available with theoffull
thetext
study
17 to the
of this
Clinicians aim to use noninvasive pro- tocol,
article which was
at NEJM.org. published
The study hadpreviously
no
respiratory support to minimize the risk ofcommercial sup- port, and the respiratory
such complica- tions. The most widely device manufacturers had no input in
used noninvasive ap- proach, nasal study design, data accrual, data analysis,
continuous positive airway pres- sure or manuscript preparation and no ac- cess
(CPAP), has been shown to be an effectiveto the study data.
alternative to endotracheal ventilation 3,4 as
primary
Treatment respiratory
with heated, support for preterm
humidified, high- Patients
infants.
flow nasal cannulae (high-flow therapy) is Infants were eligible for inclusion if they
an increas- ingly popular means of were born at a gestational age of 28 weeks
noninvasive respiratory support. Surveys 0 days to 36 weeks 6 days, were less than
have shown that approximately two thirds24 hours old, and had not previously
of neonatal
and 5intensive care units in the
in Australia and New Zea- land received endotracheal ventilation or
United States therapy. This approach hassurfactant treatment and if the attending
used high-flow
6
several reported advantages over CPAP, clinician had decided to commence or
including
and reduced reduced rates
in- fant painof
7-9nasal trauma
scores. continue noninvasive respiratory support.
Surveys show that it is pre- ferred by
10 In- fants were ineligible if there was an
parents 11
and nursing staff. 12 urgent need for intubation and ventilation
In a previous randomized trial comparing (as determined by the attending clinician)
high-flow therapy with CPAP as respiratoryor if they had already met the criteria for
sup- port after extubation in infants born at treatment failure, had a known major
a gesta- tional age of less than 32 weeks, congenital abnormality or pneumothorax,
we found that high-flow therapy was or had received
Recruitment 4 hours or more of CPAP
and Consent
noninferior support.
This findingtowas CPAP in preventing
consistent
8
with the The parents of all participating infants
treatment
results of otherfailure.
randomized trials of provided written informed consent. At all
neonatal respiratory support after extu- sites, antepar- tum consent was sought
bation.
Previous
7,9
studies comparing high-flow when possible. If ante- partum consent was
therapy with CPAP as primary support have obtained, infants were randomly assigned
not shown significant differences in to a study group as soon as they met the
treatment-failure or intubation rates. eligibility criteria. If antepartum consent
However,
reported theseinterim studies
data, were small, single-was not sought, parents of eligible in- fants
13,14
center
15 trials, 9 were approached at the earliest opportunity
or constituted a substudy of a
of a recent Cochrane Review after birth. In addition, at the lead center
larger trial.
The authors
sug- gested that additional, adequately (the Royal Womens Hospital, Melbourne,
powered ran- domized trials assessing Australia), the human research ethics
high-flow therapy as primary respiratory committee approved a retrospective
support
16 should be under- taken.
We performed an international, multi- consent process (see Section 2.2 in the
center, randomized, controlled trial to testSupplementary
Randomization Appendix, available at
the hypothesis that high-flow therapy NEJM.org).
A computer-generated randomization
would be non- inferior to CPAP as primary sequence with variable block sizes was
respiratory support for preterm infants used. Infants were stratified according to
(gestational age, =28 weeks 0 days) with gestational age (<32 weeks vs. =32 weeks)
early respiratory distress. and study center. Sequentially
n engl j med 375;12 nejm.org September 22, 2016 1143
new england journal
T he of
medicine
numbered, sealed, opaque envelopes could be ordered at the discretion of the
containing the treatment assignment were treating clinician. If further support was
opened as soon as both eligibility and required after discontinuation of
consent criteria had been met. respiratory support, the ran- domly
Study Intervention assigned treatment was reinitiated, except
Eligible infants were randomly assigned tothat infants in the high-flow group with
treat- ment with either high-flow therapy or previ- ous treatment failure could receive
CPAP. Infants weighing 1250 g or less CPAP at the treating clinicians discretion.
received caffeine (intravenous loading Study Outcomes
dose, 20 mg per kilogram of body weight) The primary outcome was treatment failure
on the first day of life. Other aspects of with- in 72 hours after randomization.
care were provided according to indi- vidual Treatment was considered to have failed if
unit protocols. Infants randomly assigned an infant receiving maximal support (high-
to the high-flow group received an initial flow therapy at a gas flow of 8 liters per
gas flow of 6 to 8 liters per minute, from minute or CPAP at a pressure of 8 cm of
either the Optiflow Junior (Fisher and Paykel water) met one or more of the following
Healthcare) or Precision Flow (Vapotherm)criteria: a fraction of inspired oxygen of 0.4
device. The size of the nasal can- nulae or higher, a pH of 7.2 or less plus a partial
was determined according to the manufac- pressure of carbon dioxide greater than 60
turers instructions in order to maintain a mm Hg (8.0 kPa) in a sample of arterial or
leak at the nares. The maximum free-flowing capillary blood obtained at
permissible gas flow was 8 liters per least 1 hour after commence- ment of the
minute, as recommended by the assigned treatment, or either two or more
manufacturer. Infants assigned to high- episodes of apnea requiring positive-pres-
flow therapy who met the criteria for sure ventilation within a 24-hour period or
treatment failure could receive CPAP as six or more episodes requiring any
rescue therapy, initiated at 7 to 8 cm of intervention within a 6-hour period. Infants
water. Infants who con- tinued to meet with an urgent need for intubation and
treatment-failure criteria were intubated mechanical ventilation (as deter- mined by
and ventilated. In the infants randomly the treating clinician) were also con-
assigned to CPAP, the starting pressure was sidered to have treatment failure.
6 to 8 cm of water, achieved with a Prespecified secondary outcomes included
ventilator, an underwater bub- ble the reason (or reasons) for treatment
system, or a variable-flow device. failure, the use of mechanical ventilation
Treatment was delivered through either within 72 hours after randomization or at
short binasal prongs or a nasal mask, any time during admission, nasal trauma,
according to the protocol at each other complications, including
participating center, with sizing determined complications of prematurity, and other
according to the manufacturers mea- sures of the use of respiratory support
recommenda- tions. The maximum and of neonatal health. An additional
permissible pressure was 8 cm of water. secondary The complete out-list
18
comeof pre-
wasspecified
the cost of care,
Infants treated with CPAP who met the secondary
calculated on the basis provided
outcomes is in infants
of data for the at
criteria for treatment failure were intu- study
all protocol and
participating in Section
Australian 2.3(435
units in the
bated and ventilated. Changes in Supple- mentary
infants) (Section 4.1Appendix. Serious mentary
in the Supple- adverse
respiratory support were made in steps of Appendix). 1
events were defined as death before
liter per minute (for high-flow therapy) or 1 hospital discharge and pneumothorax or
cm of water (for CPAP). All infants were other air leak during the assigned
evaluated at least daily. Weaning from treatment. Data were collected until death
noninva- sive respiratory support was or discharge home.
considered if there was clinical Statistical Analysis
improvement and the infants were On the basis of data from the participating
receiving a fraction of inspired oxygen of Aus- tralian centers, we estimated that
0.3 or lower, whereas discontinuation of treatment fail- ure within 72 hours after
noninvasive support was considered in randomization would
infants who were re- ceiving a fraction of
1144 inspired oxygen of 0.3 or lower,
n engl j med with
375;12 gas
nejm.org September 22, 2016
flow of 4 liters per minute (in the high-flow
group) or pressure of 5 cm of water (in the
CPAP group); earlier cessation of support
Nasal High-Flow Therapy in Preterm
Infants
occur in 17% of infants assigned to receivesignificant difference (P<0.001) in the rate
CPAP. We prespecified a noninferiority of the primary outcome between treatment
margin for high-flow treatment of 10 groups.
percentage points above the failure rate for
CPAP treatment. High- flow therapy would Re su l ts
be considered noninferior to CPAP if the Duration and Cessation of Recruitment
difference in the risk of treatment failure Infants were recruited from May 27, 2013,
and the upper limit of the two-sided 95% to June 16, 2015. On June 12, 2015, after
confidence interval were less than 10% and reviewing the primary outcome data for
the lower limit of the 95% confidence the first 515 re- cruited infants, the
interval was below zero. For the 17,19study to independent data and safety monitoring
have 90% this
We chose power, a sample
margin of 750 infants
of noninferiority aftercommittee recommended that the trial be
was required.
considering the following factors: high-flowstopped, since there was a highly sig-
ther- apy is already widely accepted in nificant difference (P<0.001) in the rate of
many neonatal intensive care units; infantsthe primary outcome between treatment
in whom high-flow treatment failed could groups and continued recruitment was
receive CPAP treatment, which we extremely unlikely to show the
hypothesized would obviate the need for noninferiority of high-flow therapy to CPAP.
intubation and ventilation in some infants; The steering committee stopped recruit-
and the primary study outcome was short-ment on June 16, 2015.
Study Patients
term efficacy, rather than death or In total, 583 infants were randomly
disability (a lower margin of noninferiority assigned to a treatment group (289 to the
would be required for death or disability). high-flow group and 294 to the CPAP
The neonatologists and par- ent group) (Fig. 1). Nineteen infants were
representatives who were consulted duringexcluded because they did not meet the
the design phase of the trial agreed to thiseligibility criteria or their parents did not
non- inferiority margin. The primary and provide consent. The remaining 564 infants
secondary outcomes were analyzed on an (278 in the high-flow group and 286 in the
intention-to-treat basis. A pre- specified CPAP group) were followed until hospital
subgroup analysis on the basis of ges- discharge or death and were included in
tational age (<32 weeks or 19 =32 weeks) and the analysis. Demo- graphic and clinical
)a were performed for both the primary
per-protocol analysis (not prespecified but characteristics of the moth- ers and infants
outcome and thefor
intuba- tion ratetrials
within 72
recom- mended noninferiority
hours after randomization. For the primarywere similar in the two groups (Table 1).
outcome and dichotomous sec- ondary Primary Outcome
outcomes, we calculated a risk difference Treatment failure within 72 hours after
(with a two-sided 95% confidence interval)random- ization occurred in 71 of the 278
in percentage points between treatment infants (25.5%) in the high-flow group and
groups. We used chi-square tests to in 38 of the 286 in- fants (13.3%) in the
compare dichotomous outcomes and the CPAP group (risk difference, 12.3
appropriate parametric test (Students t- percentage points; 95% confidence
test) or nonparametric test (difference in interval, 5.8 to 18.7; P<0.001). Treatment
medians estimated by quantile regression)failure was sig- nificantly more common in
to compare continuous outcomes. All the high-flow group than in the CPAP group
analyses were performed with the use of both among infants with a gestational age
Stata/IC
an inde-software,
pendent ver-
datasion
and13.1
safety
17 of less than 32 weeks and among those
(StataCorp). As specified in the trial
monitoring committee, consisting of two with a gestational age of 32 weeks or
protocol,
neonatologists and a statisti- cian, greater atduring
Intubation randomization (Table
the First 72 Hours2).
reviewed outcome data when the primaryafter Randomization
outcome was available for 250 infants andThere was no significant between-group
when it was available for 500 infants. The differ- ence in intubation rates within 72
committee could recommend stopping thehours after randomization, either in the
trial if there were safety concerns or if overall study popula- tion or in the
there was a highly gestational-age subgroups (Table 2).
n engl j med 375;12 nejm.org September 22, 2016 1145
new england journal
T he of
medicine
3349 Infants admitted to NICU
were screened for eligibility
2256 Were ineligible 1636 Did not receive noninvasive
respiratory support 393 Were intubated, received
surfactant, or both 92 Were =24 hr of age 51 Had major
congenital anomaly or air leak 46 Met treatment-failure
criteria with CPAP of 8 cm water 36 Had received =4 hr
of CPAP treatment 2 Received palliative care in the
delivery room
1093 Were eligible
510 Did not undergo randomization 395 Had parents
who were not approached 264 Had parents who were
unavailable or a research team that was not notified 81
Had language or social factors 18 Were in another study,
prohibiting participation 17 Were transferred to another
hospital 13 Had a clinician who made the decision 2
Were in a NICU that did not have high-flow equipment
available 113 Had parents who declined prospective
consent 2 Had parents who consented but clinicians who
decided against randomization
583 Underwent randomization
289 Were assigned to high-flow treatment 294 Were assigned to CPAP treatment 206
201 Had parents who provided Had parents who provided prospective
prospective consent 88 Had parents who consent 88 Had parents who were
were approached for retrospective consent approached for retrospective consent
8 Were excluded 5 Had parents
11 Were excluded 5 Had parents
who declined retrospective
who declined retrospective
consent 2 Were ineligible and
consent 2 Had parents who
under- went randomization in
withdrew prospective consent 4
error 1 Underwent
Were ineligible and under- went
randomization without
randomization in error
prospective parental consent
278 Infants were followed until death 286 Infants were followed until death
or discharge and included in the or discharge and included in the
primary intention-to-treat analysis primary intention-to-treat analysis
F i g ur e 1 . Num b e r s o f In f an t s W h o We r e S c r e e n e d , A s s i g n e d t o a S t u d y G r o up, an
d In c l born
Infants u d eatdaingestational
t h e P r im a rofy 28
age A nweeks
a l ys 0i s . to 36 weeks 6 days were screened for eligibility. CPAP
days
denotes continuous positive airway pressure, and NICU neonatal intensive care unit.
1146 n engl j med 375;12 nejm.org September 22, 2016
Nasal High-Flow Therapy in Preterm
Infants
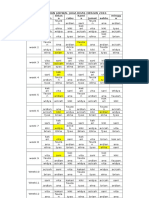
Table 1. Baseline Characteristics of the Mothers and
Infants.*
Characteristic High-Flow Group (N = 278) CPAP Group (N = 286)
Mothers
White race no. (%) 217 (78.1) 225 (78.7) Primigravida no. (%) 117 (42.1) 119 (41.6) Exposure to
antenatal glucocorticoids no. (%) 224 (80.9) 229 (80.4) Cesarean section no. (%) 204 (73.4) 200 (69.9)
Prolonged rupture of membranes =24 hr before delivery no. (%) 33 (11.9) 37 (12.9) Obstetrical diagnosis of
chorioamnionitis no. (%) 22 (8.0) 13 (4.6)
Infants
Gestational age No. of weeks 32.02.1 32.02.2 <32 wk no. (%) 140 (50.4) 149 (52.1) Birth weight g
1737580 1751599 Male sex no. (%) 157 (56.5) 156 (54.5) Multiple birth no. (%) 109 (39.2) 109 (38.1)
Median Apgar score at 5 min (IQR) 8 (89) 9 (89) Median postnatal age at randomization (IQR) hr 1.4
(0.62.9) 1.3 (0.72.8) Treatment with CPAP before randomization No. of infants (%) 157 (56.5) 166 (58.0)
Median duration (IQR) hr 1.6 (0.82.7) 1.5 (0.62.5) Arterial or capillary blood pH before randomization
7.260.07 7.270.07 Partial pressure of arterial or capillary carbon dioxide before
randomization mm Hg 55.210.8 55.39.8
Median fraction of inspired oxygen at time of randomization (IQR) 0.21 (0.210.28) 0.21 (0.210.30) Caffeine
received in first 24 hr of life no. (%) 109 (39.2) 125 (43.7)
* Plusminus values are means SD. There were no significant differences between the groups. CPAP denotes
continuous positive airway pressure, and IQR interquartile range. Race was reported by the investigators. Data
on exposure to antenatal glucocorticoids were missing for 1 infant in each treatment group. Obstetrical diagnosis of
chorioamnionitis was not known for 2 infants in the high-flow group and 3 in the CPAP group. The Apgar score was
not known for 2 infants in the high-flow group. Blood gases were not measured before randomization in 297 infants:
145 in the high-flow group and 152 in the CPAP group.
Per-Protocol Analysis Secondary Outcomes and Adverse
Results were similar in an analysis of the Events
The most common reason for treatment
543 infants (264 in the high-flow group and failure was a fraction of inspired oxygen of
279 in the CPAP group) who were treated 0.4 or higher (Table 3). Treatment failure
as specified by the protocol (Table 2). A due to an urgent need for intubation
total of 21 infants were excluded from thisoccurred more frequently in the CPAP group
analysis because either they did not than in the high-flow group (18.4% vs.
receive the assigned treatment (14 infants) 5.6%, P = 0.03). The median duration of
or the assigned treatment was changed respiratory support was 1 day longer in the
during the primary-outcome period without high- flow group than in the CPAP group (4
the protocol-specified criteria for treatment
vs. 3 days, P = 0.005), and infants in the
failure or nasal trauma having been met (7high-flow group were significantly more
infants). likely to receive supple-
n engl j med 375;12 nejm.org September 22, 2016 1147
new england journal
T he of
medicine
Table 2. Primary Outcome, Intubation within 72 Hours, and Outcomes in the Subgroup and Per-
Protocol Analyses.
Outcome High-Flow Group (N = 278) CPAP Group (N = 286) Risk Difference (95% CI)* P Value
no./total no. (%) percentage points
Primary intention-to-treat
analysis
Treatment failure within 72 hr 71/278 (25.5) 38/286 (13.3) 12.3 (5.8 to 18.7) <0.001 Gestational age <32 wk
46/140 (32.9) 27/149 (18.1) 14.7 (4.8 to 24.7) 0.004 Gestational age =32 wk 25/138 (18.1) 11/137 (8.0) 10.1 (2.2
to 18.0) 0.01 Intubation within 72 hr 43/278 (15.5) 33/286 (11.5) 3.9 (-1.7 to 9.6) 0.17 Gestational age <32 wk
30/140 (21.4) 24/149 (16.1) 5.3 (-3.7 to 14.3) 0.25 Gestational age =32 wk 13/138 (9.4) 9/137 (6.6) 2.9 (-3.5 to
9.3) 0.38
Per-protocol
analysis
Treatment failure within 72 hr 64/264 (24.2) 36/279 (12.9) 11.3 (4.8 to 17.8) <0.001 Intubation within 72 hr 39/264
(14.8) 33/279 (11.8) 2.9 (-2.8 to 8.7) 0.31
* Positive values favor the CPAP group, and negative values favor the high-flow group. Apparent discrepancies in
some of the risk differences are due to rounding.
mental oxygen during their admission of treatment failure than did CPAP when
(78.1% vs. 69.6%, P = 0.02). Respiratory used as primary respiratory support for
diagnoses in the participating infants are preterm infants born at 28 weeks 0 days of
reported in Section 3.3 in the gestation or later and treated in neonatal
Supplementary Appendix. There was no intensive care units. Enroll- ment was
significant difference between treatment stopped after a planned interim analy- sis
groups in the rate of death before dis- (after 75% of the target sample had been
charge (Table 4). Nasal trauma was re- cruited), on the recommendation of the
significantly more common in the CPAP data and safety monitoring committee,
group than in the high-flow group (18.5% owing to the between-group difference in
vs. 8.3%, P<0.001). The frequency of rates of treatment failure. The difference in
pneumothorax or other air leak from the the primary outcome was significant in
lung was also significantly higher in the both the primary intention-to- treat
CPAP group during the assigned treatmentanalysis and the per-protocol analysis. Our
(2.1% vs. 0.0%, P = 0.02) but not overall results contrast with those of studies of
(3.6% in the high-flow group and 2.8% in high-flow therapy initiated after
the CPAP group, P = 0.59). Rates of other extubation, which have consistently shown
Unlike 7-9,16
the infants in the trials of
complications of prematurity did not differthat the effi- cacy of high-flow treatment is
postextubation high-flow therapy, no
significantly between the groups. The similar to that of CPAP.
infants in our study received surfactant
respiratory-support devices and nasal
before7-9random- ization.
interfaces that were used initially in each The higher rate of treatment failure
treatment group are shown in Section 3.2 among infants receiving high-flow therapy
in our study may reflect its reduced
in the Supplementary Appendix. The
calculated total cost of the tertiary hospi- effectiveness in infants with surfactant-
tal stay (in U.S. dollars) per infant did not deficient lungs. Although high-flow therapy
does
the provide
higher,
20-22 some
more distending
consistent pressure,
pres- sures
differ significantly between the CPAP and
high-flow groups ($32,036 and $29,785, produced during CPAP may account for the
respectively; P = 0.40). (Detailed difference in treatment-failure rates that
information about the cost-effective- ness we re- port. We chose to include only
analysis is provided in Sections 4.2 and 4.3infants with a gestational age of at least 28
Discussion weeks, on the basis of increased rates of
in the Supplementary Appendix.)
In this multicenter, randomized trial, high-treatment failure reported in infants with a
flow treatment resulted in a significantly lower gestational age who re- ceived 8 high-
higher rate flow therapy after extubation.
1148 n engl j med 375;12 nejm.org September 22, 2016
Nasal High-Flow Therapy in Preterm
Infants
A
total
(95% Treat
Medi AnyMediDisch of 40
CI) P Apne Fracti
RespiUrgeClinic
MediSurfa MediDisch WeigMediMedi
an ment infant
Value a on ofratory nt iansan ctant receian arged an arged ht atan an
may
9/71inspiracidoneed timetreatno. of ved age home
decisi age home disch
no. of
no. of s
have
ed sis for on to mentdays durinat withat withargedaysdays
(12.7) were
of failed exclu
Differ 2/38oxyg9/71intub 4/71treat g cessa oxygstartgastri gin in
for
ence (5.3)en (12.7) (5.6)mentno. respir admition en of c- 2540
ation tertiar
any ded:
more
in =0.46/384/712/38failur(%) atory ssion
7.4 (- (IQR)therafull- tube424 y hospi the
supp py than 38
Medi 3.1 to
53/71(15.8)
(5.6)
(5.3)e 40 suck feedi2551care tal
ort one infant
an 17.9)(74.6)
-3.1 7/380.4 (-
after(14.4) no. daysno. feeding 492cente(IQR)
reaso
NA 30/38 (-17.1
(18.4)
8.5 to
rando30 durin (%) 2 (0 (%)ng no. NA r 37 s who
g n. were
0.22(78.9)to -12.8 9.3)mizati(10.5) 217 to 5)1 (IQR) (%)NA (IQR) (23 to
admi Clinic disch
-4.3 10.8)(-26.2
NA on 3.9 (- (78.1)
2 (0(0.4) 21 0.77 2050)
ssion 199 to 6)2 days(7.6) (10 to ians arged
(-20.7
NA to 0.94(IQR) 1.5 to 38
decisi
to 0.650.7) hr9.3)(IQR) (69.6) NA (0.7) 3217 35) (22 to home
4 (2 ons with
Differ
Perc 12.1) NA 7.8 NA 8.5 0.0 (-
-0.3 (18 to(6.0) 19 50)
to
ence
enta NA 0.03 (1.9 0.16to 7) (1.3 0.7 to (-1.543) 1.6 (- (10 to NA gastri
(95% 3 (2 chan c-
ge-in 0.62 to to 0.7) to 32 2.5 to 34) -1.0
CI) to 6) 15.7) ge tube
Risk
Point 21.5) 1.00 0.9) (17 to
5.8) NA (-5.4
NA treat feedi
9.0 NA NA 45) NA 1.0 (-
to
1.0 ment ng
(2.8 0.02 0.58NA 0.45 2.3 to 3.4) The 3
(0.3 were (21 in
to 0.0 (- 4.3) 0.66 infant
to made the
25.2) 3.9 to 0.56
1.7) in s whohigh-
NA 3.9) were
0.005 relati flow
-1.2 1.00
CPA on to dischgroup
(-10.1
P (N = the argedand
to
Grou286) work home17 in
6.3)
p of with the
0.65
breatoxyg CPA
hing, en P
withotheragroup
High- ut py (1) and
Flow fulfilli in thethe 2
Grou(N = ng high- infant
p 278) any flow s who
prespgroup died
ecifieand
Positi 2 2
The
ve d in the
infant
treat-CPA
value s who
Table s P died
3. favor group befor
Reas the ) e
ons CPA were disch
for P exclu
arge
Treat group ded. (1 in
ment , and each
Failu negat treat
re ive ment
Reas value
and on for group
Othe s ) befor
treat favor e
r ment were
Seco the exclu disch
failur high-
ndar e ded. arge
y flow (1 in
no./to group each
Outc tal
omes Suppl . treat
no. emen * NA ment
.* (%) denot
tal group
oxyg es ).
not ment-
en failur
thera applic
py able. e
criteri
Outc a.
ome
n engl j med 375;12 nejm.org September 22, 2016 1149
new england journal
T he of
medicine
Table 4. Adverse
Events.
Event High-Flow Group (N = 278) CPAP Group (N = 286) Risk Difference (95% CI)* P Value
no. of infants (%) percentage points
Death before discharge 1 (0.4) 1 (0.4) 0.0 (-1.0 to 1.0) 0.98 Oxygen supplementation, respiratory support, or both
at postmenstrual age of 36 wk 17 (12.1) 17 (11.4) 0.7 (-6.7 to 8.2) 0.85
Pneumothorax or other air leak syndrome During assigned treatment 0 6 (2.1) -2.1 (-3.8 to -0.4) 0.02 Any time during admission 10
(3.6) 8 (2.8) 0.8 (-2.1 to 3.7) 0.59 Postnatal glucocorticoid treatment for lung disease 1 (0.4) 3 (1.0) -0.7 (-2.1 to 0.7) 0.33 Nasal
trauma 23 (8.3) 53 (18.5) -10.3 (-15.8 to -4.7) <0.001 Patent ductus arteriosus treated with medication or
surgical ligation 11 (4.0) 6 (2.1) 1.9 (-1.0 to 4.7) 0.20
Confirmed sepsis 7 (2.5) 13 (4.5) -2.0 (-5.1 to 1.0) 0.19 Necrotizing enterocolitis, Bells stage II or III 2 (0.7) 0 0.7 (-0.3 to 1.7)
0.15 Isolated intestinal perforation 0 1 (0.3) -0.3 (-1.0 to 0.3) 0.32 Laser surgery for retinopathy of prematurity 0 1 (0.7) -0.7 (-2.0
to 0.6) 0.33 Intraventricular hemorrhage, grade 3 or 4 4 (2.9) 1 (0.7) 2.2 (-0.9 to 5.2) 0.15 Cystic periventricular leukomalacia 3
(2.1) 2 (1.3) 0.8 (-2.2 to 3.8) 0.60
* Positive values favor the CPAP group, and negative values favor the high-flow group. Data are reported for the 289 infants born
at a gestational age of less than 32 weeks (140 infants in the high-flow group and 149 in the CPAP group). The criteria for
confirmation of sepsis were a positive blood culture and treatment with intravenous antibiotics for 48 hours or longer. Modified
Bells criteria stages range from I to III, with higher stages indicating greater disease severity.
In our study, intubation rates did not differBlinding of the intervention was not
significantly between the groups, probablypossible; therefore, to minimize bias, we
be- cause the use of CPAP as rescue used prespeci- fied, objective criteria to
therapy for in- fants with treatment failure determine the primary outcome. We
in the high-flow group meant that acknowledge that the use of CPAP as
subsequent intubation was not required in rescue therapy may have influenced the
39% of those infants (28 of 71). We rates of secondary outcomes in the high-
included rescue CPAP in our trial design flow group. Furthermore, over half of the
because in our
almost half previous
of the 8 noninferiority study
infants in whom high- infants assigned to this group had received
of high-flow
flow treatmenttreatment after
failed did notextubation,
require CPAP for a brief period (median, 1.6 hours)
intubation after receiving rescue CPAP. before randomization, which may also have
Although CPAP was associated with a lower influenced the outcomes. Our study
rate of treatment failure than was high-flow population was limited to preterm infants in
therapy, intubation rates did not differ neonatal intensive care units. Further
signifi- cantly between the two treatment studies are required to determine the
groups; in addition, infants in the high-flowsafety and efficacy of high-flow therapy in
group had a significantly lower rate of nasal nontertiary fa- cilities and resource-limited
trauma. How- ever, infants in the high-flowsettings, as well as in term infants. We
group were more likely to receive brief conclude that high-flow treatment results in
supplemental oxygen, and the median a significantly higher rate of treatment
duration of respiratory support was 1 day failure than does CPAP, when used as
longer in this group. The clinical impor- primary support
Supported for preterm
by grants from infants
the National with
Health and
Medical Re- search
respiratory Council (1079089 and Centre of
distress.
tance of these findings is uncertain. Research ExcellenceNew-
1150 n engl j med 375;12 nejm.org September 22, 2016
Nasal High-Flow Therapy in Preterm
Infants
born Medicine Grant 1060733), the Royal Brisbane Disclosure forms provided by the authors are
and Womens Hospital Foundation, and the available with the full text of this article at NEJM.org.
participating neonatal units. Dr. Davis reports We thank the families of all infants who participated
receiving travel support from Fisher and Paykel. No in the study and the staff members who cared for
other potential conflict of interest relevant to this them.
article was reported.
References
1. Hamilton BE, Martin JA, Ostermanified high-flow nasal cannula versus 16 . Wilkinson D, Andersen C,
MJK, Curtin SC. Births: preliminary na- sal CPAP for respiratory support ODonnell CP, De Paoli AG, Manley
data for 2014. Natl Vital Stat Rep in neo- nates. Pediatrics 2013; BJ. High flow nasal cannula for
2015; 64(6): 1-19. 10 . Osman
131(5): M, Elsharkawy A, Abdel-respiratory support in preterm
e1482-90.
2. Chess PR, DAngio CT, Pryhuber Hady H. Assessment of pain during infants. Cochrane Database Syst
GS, Maniscalco WM. Pathogenesis of application of nasal-continuous 1 7. Roberts
Rev 2016; 2:CT, Owen LS, Manley BJ,
CD006405.
bron - chopulmonary dysplasia. positive airway pres - sure and Do- nath SM, Davis PG. A
Semin Perinatol 2006; 30: 171-8. heated, humidified high-flow nasal multicentre, ran- domised
3. SUPPORT Study Group of the cannulae in preterm infants. J Peri - controlled, non-inferiority trial,
Eunice Kennedy Shriver NICHD 11 . Klingenberg
natol C, Pettersen M,
2015; 35: 263-7. comparing high flow therapy with
Neonatal Re - search Network. EarlyHansen EA, et al. Patient comfort nasal continuous positive airway
CPAP versus surfac- tant in during treat - ment with heated pressure as primary support for
extremely preterm infants. N Engl J humidified high flow nasal cannulae preterm infants with respiratory
4.
MedMorley
2010;CJ, Davis
362: PG, Doyle LW, versus nasal continuous positive distress (the HIPSTER trial): study
1970-9.
Brion LP, Hascoet J-M, Carlin JB. airway pressure: a randomised 18 . Drummond
protocol. BMJ OpenMF, 2015;
Sculpher 5(6):MJ,
Nasal CPAP or intubation at birth for cross-over trial. Arch Dis Child FetalTorrance
e008483. GW, OBrien BJ, Stoddart
very preterm in - fants. N Engl J 12
Neo. Roberts CT,2014;
- natal Ed Manley
99:BJ, Dawson GL. Methods for the economic
F134-7.
5.
MedHochwald O, Osiovich
2008; 358: 700-8. H. The use of
JA, Davis PG. Nursing perceptions ofevaluation of health care
high flow nasal cannulae in neonatalhigh- flow nasal cannulae treatmentprogrammes. 3rd ed. Oxford,
in - tensive care units: is clinical for very preterm infants. J Paediatr 19 . Piaggio
England: G, Elbourne
Oxford UniversityDR,Press,
Pocock
practice con- sistent with the Child Health 2014; 50: 806-10. SJ, Evans SJ, Altman DG. Reporting
2005.
evidence? J Neonat Perinat Med 13 . Nair G, Karna P. Comparison of of non - inferiority and equivalence
6. Hough
2010; JL, Shearman AD, Jardine the effects of Vapotherm and nasal randomized trials: extension of the
3: 187-91.
LA, Davies MW. Humidified high flow CPAP in respiratory distress. CONSORT 2010 statement. JAMA
nasal cannulae: current practice in Presented at the Pe - diatric Academic 2 0. Kubicka
2012; 308: ZJ, Limauro J, Darnall RA.
2594-604.
Australasian nurseries, a survey. J Societies Meeting, Balti- more, May Heated, humidified high-flow nasal
Paediatr Child Health 2012; 48: 106- 1417, 2005. abstract (http:// www can - nula therapy: yet another way
13.Collins CL, Holberton JR, Barfield 14
7. . Iranpour R, Sadeghnia
.abstracts2view .com/ pas/ ).A, to deliver continuous positive airway
C, Davis PG. A randomized Hesaraki M. High-flow nasal cannulapressure? Pe - diatrics 2008; 121: 82-
controlled trial to compare heated versus nasal continuous positive 21 8. . Spence KL, Murphy D, Kilian C,
humidified high-flow nasal cannulaeairway pressure in the management Mc- Gonigle R, Kilani RA. High-flow
with nasal continuous pos - itive of respiratory distress syndrome. J nasal cannula as a device to provide
airway pressure postextubation in Isfahan Med School 2011; 29: 761- continuous positive airway pressure in
premature infants. J Pediatr 2013; 15 71.. Ciuffini F, Pietrasanta C, infants. J Peri - natol 2007; 27: 772-5.
8. Manley
162(5): BJ, Owen LS, Doyle LW, etLavizzari A, et al. Comparison
949-54.e1. 22 . Wilkinson DJ, Andersen CC,
al. High-flow nasal cannulae in verybetween two different modes of Smith K, Holberton J. Pharyngeal
preterm infants after extubation. N non-invasive ventilatory support in pressure with high-flow nasal
Engl J Med 2013; 369: 1425-33. preterm newborn infants with cannulae in premature infants. J
9. Yoder BA, Stoddard RA, Li M, Kingrespira - tory distress syndrome mild Perinatol
Copyright 2008;
2016 28: 42-7.
Massachusetts Medical
J, Dirnberger DR, Abbasi S. Heated, to moderate: preliminary data. Society.
humid - Pediatr Med Chir 2014; 36: 88.
ARTICLE METRICS NOW
AVAILABLE
Visit the article page at NEJM.org and click on the Metrics tab
to view comprehensive and cumulative article metrics
compiled from multiple sources, including Altmetrics. Learn
more at www.nejm.org/page/article-metrics-faq.
n engl j med 375;12 nejm.org September 22, 2016 1151
You might also like
- High-Flow Nasal Cannulae in Very Preterm Infants After ExtubationDocument9 pagesHigh-Flow Nasal Cannulae in Very Preterm Infants After ExtubationRiska Diene PratiwiNo ratings yet
- Cpap Vs SurfactanteDocument10 pagesCpap Vs SurfactanteAngelicia Varela MuñozNo ratings yet
- 2010 Early CPAP Vs Surfactant in EPTI NEJMDocument10 pages2010 Early CPAP Vs Surfactant in EPTI NEJMFiorella VilcaNo ratings yet
- Epinephrine and Dexamethasone in Children With BronchiolitisDocument11 pagesEpinephrine and Dexamethasone in Children With BronchiolitisAdelina Wahyuni LubisNo ratings yet
- A Randomized Trial of High-Flow Oxygen Therapy in Infants With BronchiolitisDocument11 pagesA Randomized Trial of High-Flow Oxygen Therapy in Infants With BronchiolitisErwin YanthoNo ratings yet
- Tratamiento de Broquiolitis ArticuloDocument11 pagesTratamiento de Broquiolitis ArticulojorgepinotNo ratings yet
- Journal Pone 0000192Document5 pagesJournal Pone 0000192TriponiaNo ratings yet
- SurE vs InSurE Surfactant TherapyDocument44 pagesSurE vs InSurE Surfactant TherapySubash PaudealNo ratings yet
- Non Invasive Versus Invasive Respiratory Support in Preterm InfantsDocument25 pagesNon Invasive Versus Invasive Respiratory Support in Preterm InfantshosnameskarNo ratings yet
- IJN - Volume 11 - Issue 4 - Pages 50-56nbnDocument7 pagesIJN - Volume 11 - Issue 4 - Pages 50-56nbnfitriNo ratings yet
- PILLOW 2012_Innovation in Surfactant Therapy II-surfactant Administration by Aerosolization.Document8 pagesPILLOW 2012_Innovation in Surfactant Therapy II-surfactant Administration by Aerosolization.Rafael JustinoNo ratings yet
- Jurnal Pubme 1 RdsDocument13 pagesJurnal Pubme 1 Rdsriri risna aNo ratings yet
- Buonsenso Et Al-2018-Pediatric PulmonologyDocument9 pagesBuonsenso Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- Evidence Support and Guidelines For Using Heated, Humidified, High-Flow Nasal Cannulae in NeonatologyDocument13 pagesEvidence Support and Guidelines For Using Heated, Humidified, High-Flow Nasal Cannulae in NeonatologylilyNo ratings yet
- 33 - 10.1080@14767058.2020.1735339Document8 pages33 - 10.1080@14767058.2020.1735339Rosa PerezNo ratings yet
- SA PerformanceDocument8 pagesSA Performancefernin96No ratings yet
- Trends in Use of Neonatal CPAP - A Population-Based StudyDocument7 pagesTrends in Use of Neonatal CPAP - A Population-Based StudyGabrielaNo ratings yet
- SDR Segun EdadDocument9 pagesSDR Segun EdadLuzbenia ChaparroNo ratings yet
- Systematic Review Found That Using Thin Catheters to Deliver Surfactant to Preterm Neonates 2020Document26 pagesSystematic Review Found That Using Thin Catheters to Deliver Surfactant to Preterm Neonates 2020renzoNo ratings yet
- Mechanical Ventilation of The Premature NeonateDocument16 pagesMechanical Ventilation of The Premature NeonateHaitham HafezNo ratings yet
- A Randomized Placebo-Controlled Pilot Trial of Early Targeted Non-Steroidal AntiInflammatory Drugs in Preterm Infants With A Patent Ductus ArteriosusDocument22 pagesA Randomized Placebo-Controlled Pilot Trial of Early Targeted Non-Steroidal AntiInflammatory Drugs in Preterm Infants With A Patent Ductus ArteriosusGlydenne Glaire Poncardas GayamNo ratings yet
- Bubble CPAP Vs Ventilatory CPAPDocument9 pagesBubble CPAP Vs Ventilatory CPAPRyan Rahman OesmanNo ratings yet
- Canadian Guidelines 2021Document7 pagesCanadian Guidelines 2021Radu CiprianNo ratings yet
- Impact of Prophylactic Continuous Positive Airway Pressure On Transient Tachypnea of The Newborn and Neonatal Intensive Care Admission in Newborns Delivered by Elective Cesarean SectionDocument8 pagesImpact of Prophylactic Continuous Positive Airway Pressure On Transient Tachypnea of The Newborn and Neonatal Intensive Care Admission in Newborns Delivered by Elective Cesarean SectionFabiano SilvaNo ratings yet
- Guidelines For Surfactant Replacement Therapy in NeonatesDocument7 pagesGuidelines For Surfactant Replacement Therapy in NeonatesFer45No ratings yet
- DANI 2012_Surfactant replacement in preterm infants with RDSDocument4 pagesDANI 2012_Surfactant replacement in preterm infants with RDSRafael JustinoNo ratings yet
- Non Invasive HFO Time For Consideration 2017Document3 pagesNon Invasive HFO Time For Consideration 2017OsmanyNo ratings yet
- Ramgolam2018 PDFDocument10 pagesRamgolam2018 PDFmortazaqNo ratings yet
- El Farrash2018Document27 pagesEl Farrash2018YULISSA FLORES RONDONNo ratings yet
- Articulo Tesis 9Document8 pagesArticulo Tesis 9Lourdes MarcosNo ratings yet
- Effectiveness of IntrapleuralDocument9 pagesEffectiveness of IntrapleuralteowijayaNo ratings yet
- HHDocument9 pagesHHzainul umariNo ratings yet
- Jarvis 2014Document6 pagesJarvis 2014lalaNo ratings yet
- Comparison of Urokinase and Video-Assisted Thoracoscopic Surgery For Treatment of Childhood EmpyemaDocument7 pagesComparison of Urokinase and Video-Assisted Thoracoscopic Surgery For Treatment of Childhood EmpyemaDr Nilesh NagdeveNo ratings yet
- RCCM 200601-027ocDocument7 pagesRCCM 200601-027ocDiego AndradeNo ratings yet
- Home-Made Continuous Positive Airways Pressure Device May Reduce Mortality in Neonates With Respiratory Distress in Low-Resource SettingDocument5 pagesHome-Made Continuous Positive Airways Pressure Device May Reduce Mortality in Neonates With Respiratory Distress in Low-Resource SettingNovi AryandaNo ratings yet
- The Effect of Extended Continuous Positive Airway Pressure on Lung VolumesDocument15 pagesThe Effect of Extended Continuous Positive Airway Pressure on Lung Volumesblufire78No ratings yet
- Wright Et Al 2022 PDFDocument9 pagesWright Et Al 2022 PDFRadu CiprianNo ratings yet
- NakatoIJP Volume6 Issue9 Pages8215-8223Document9 pagesNakatoIJP Volume6 Issue9 Pages8215-8223Siti HumairahNo ratings yet
- 2012 Randomized Controlled Trial of Restrictive Fluid Management in TTNDocument14 pages2012 Randomized Controlled Trial of Restrictive Fluid Management in TTNyaritzaalviarezNo ratings yet
- Pediatric Sedation Pearls: Presedation Airway Assessment Joshua Nagler, MD Children's Hospital, Boston, MADocument11 pagesPediatric Sedation Pearls: Presedation Airway Assessment Joshua Nagler, MD Children's Hospital, Boston, MAPSD12345No ratings yet
- Ajrcccm 2004Document9 pagesAjrcccm 2004kichilla1No ratings yet
- Increase 1.Document10 pagesIncrease 1.Maria Jose Contreras SilvaNo ratings yet
- Dargaville 2021Document10 pagesDargaville 2021Radu CiprianNo ratings yet
- RCP y Resultados A Corto Plazo en Prematuros. JPedDocument8 pagesRCP y Resultados A Corto Plazo en Prematuros. JPedSheila Patricia Castro ErazoNo ratings yet
- Shortacting-sedativeanalgesic-drugs-protect-against-development-of-ventilatorassociated-events-in-children-Secondary-analysis-of-the-EUVAE-study_2021_American-Association-for-Respiratory-CareDocument8 pagesShortacting-sedativeanalgesic-drugs-protect-against-development-of-ventilatorassociated-events-in-children-Secondary-analysis-of-the-EUVAE-study_2021_American-Association-for-Respiratory-CareevyNo ratings yet
- Background: Corresponding AuthorDocument8 pagesBackground: Corresponding AuthorPratiwi UmbohNo ratings yet
- Randomized Trial of Laryngeal Mask Airway Versus Endotracheal Intubation For Surfactant DeliveryDocument6 pagesRandomized Trial of Laryngeal Mask Airway Versus Endotracheal Intubation For Surfactant DeliveryKelompok 8 PF HTTNo ratings yet
- Risks and Outcomes of Infants with Transient Tachypnea of the NewbornDocument5 pagesRisks and Outcomes of Infants with Transient Tachypnea of the NewbornVerushka CrespoNo ratings yet
- Pediatric Critical Care MedicineDocument107 pagesPediatric Critical Care Medicinerahmawatusayu100% (1)
- Usg Pada TB PulmoDocument8 pagesUsg Pada TB Pulmoaradana wahyudaNo ratings yet
- Articulos BronquiolitisDocument18 pagesArticulos BronquiolitisLaura López Del Castillo LalydelcaNo ratings yet
- 1466 FullDocument15 pages1466 FullMelvy RozaNo ratings yet
- ProneDocument8 pagesPronesophiaNo ratings yet
- Neonatal Noninvasive Ventilation Techniques: Do We Really Need To Intubate?Document25 pagesNeonatal Noninvasive Ventilation Techniques: Do We Really Need To Intubate?sing terriblyNo ratings yet
- Premedication With Fentanyl For Less Invasive SurfDocument19 pagesPremedication With Fentanyl For Less Invasive SurfRochnald PigaiNo ratings yet
- Fisiologia de Semin - Fetal - Neon - Med - 2016 - Jun - 21 (3) - 174Document7 pagesFisiologia de Semin - Fetal - Neon - Med - 2016 - Jun - 21 (3) - 174MASIEL AMELIA BARRANTES ARCENo ratings yet
- 114 How Parents To Technology Dependent Children Experience The Transition From A Hospital Stay To Professional Home Care NursingDocument1 page114 How Parents To Technology Dependent Children Experience The Transition From A Hospital Stay To Professional Home Care NursingDaniella AwurumibeNo ratings yet
- Anesthetic Management for the Pediatric Airway: Advanced Approaches and TechniquesFrom EverandAnesthetic Management for the Pediatric Airway: Advanced Approaches and TechniquesDiego PreciadoNo ratings yet
- Activation of mTOR: A Culprit of Alzheimer's Disease?: Neuropsychiatric Disease and Treatment DoveDocument16 pagesActivation of mTOR: A Culprit of Alzheimer's Disease?: Neuropsychiatric Disease and Treatment Dovemr dexterNo ratings yet
- Ulkus Kornea Eng VerDocument15 pagesUlkus Kornea Eng VerDexter BluesNo ratings yet
- Benefits and Risks of Antiretroviral TherapyDocument12 pagesBenefits and Risks of Antiretroviral TherapyAtgy Dhita AnggraeniNo ratings yet
- Medi 96 E5795 PDFDocument5 pagesMedi 96 E5795 PDFDexter BluesNo ratings yet
- Childhood IQ and Bipolar Link PDFDocument9 pagesChildhood IQ and Bipolar Link PDFDexter BluesNo ratings yet
- Nejmoa1514762 PDFDocument12 pagesNejmoa1514762 PDFDexter BluesNo ratings yet
- SDJ 2016 09 01 PDFDocument7 pagesSDJ 2016 09 01 PDFDexter BluesNo ratings yet
- Nejmoa1606356 PDFDocument10 pagesNejmoa1606356 PDFDexter BluesNo ratings yet
- Pamj 24 182 PDFDocument5 pagesPamj 24 182 PDFDexter BluesNo ratings yet
- PRM2016 1658172 PDFDocument7 pagesPRM2016 1658172 PDFDexter BluesNo ratings yet
- The Seven Cardinal MovementsDocument4 pagesThe Seven Cardinal MovementsDexter BluesNo ratings yet
- Jurnal Anak Ririn PDFDocument10 pagesJurnal Anak Ririn PDFDexter BluesNo ratings yet
- 1830 PDF PDFDocument5 pages1830 PDF PDFDexter BluesNo ratings yet
- QuestionsDocument1 pageQuestionsDexter BluesNo ratings yet
- Referat Obgyn FixDocument29 pagesReferat Obgyn FixDexter BluesNo ratings yet
- Clinical Guidelines Acute Rehab Management 2010 InteractiveDocument172 pagesClinical Guidelines Acute Rehab Management 2010 InteractivenathanaelandryNo ratings yet
- The Seven Cardinal MovementsDocument4 pagesThe Seven Cardinal MovementsDexter BluesNo ratings yet
- Fix ObgynDocument17 pagesFix ObgynDexter BluesNo ratings yet
- Unchallengeable Miracles of QuranDocument430 pagesUnchallengeable Miracles of QuranyoursincerefriendNo ratings yet
- Rincian Jadwal Jaga Koas Obsgin 2016 Senin Selas A Rabu Kami S Jumat Sabtu Mingg UDocument1 pageRincian Jadwal Jaga Koas Obsgin 2016 Senin Selas A Rabu Kami S Jumat Sabtu Mingg UDexter BluesNo ratings yet
- Mood Dynamics in Bipolar Disorder: Research Open AccessDocument9 pagesMood Dynamics in Bipolar Disorder: Research Open AccesswulanfarichahNo ratings yet
- Referat Obgyn FixDocument29 pagesReferat Obgyn FixDexter BluesNo ratings yet
- Childhood IQ and Bipolar Link PDFDocument9 pagesChildhood IQ and Bipolar Link PDFDexter BluesNo ratings yet
- 10 4103@0378-6323 116725 PDFDocument14 pages10 4103@0378-6323 116725 PDFDexter BluesNo ratings yet
- The Seven Cardinal MovementsDocument3 pagesThe Seven Cardinal MovementsMaria Mandid0% (1)
- Jurnal Elderly 2 PDFDocument3 pagesJurnal Elderly 2 PDFDexter BluesNo ratings yet
- Pruritus: An Updated Look at An Old ProblemDocument7 pagesPruritus: An Updated Look at An Old ProblemThariq Mubaraq DrcNo ratings yet
- Geriatric Itch PDFDocument16 pagesGeriatric Itch PDFDexter BluesNo ratings yet
- TSWJ2015 803752 PDFDocument8 pagesTSWJ2015 803752 PDFDexter BluesNo ratings yet
- Final Result - Nursing Officer Central Hospitals-2019-NETDocument17 pagesFinal Result - Nursing Officer Central Hospitals-2019-NETprashanthNo ratings yet
- G 3Document17 pagesG 3Bernadette Dangate MalbasNo ratings yet
- SRM Case Studys C05-007Document8 pagesSRM Case Studys C05-007Aqfaq UdeenNo ratings yet
- Access For Dialysis - Surgical and Radiologic ProceduresDocument436 pagesAccess For Dialysis - Surgical and Radiologic ProceduresAriadna Mariniuc100% (1)
- Sultanate of Oman Ministry of Health: Requirements For Health EstablishmentsDocument15 pagesSultanate of Oman Ministry of Health: Requirements For Health Establishmentsazamk saidNo ratings yet
- 4 RehabilitationmanagementDocument20 pages4 RehabilitationmanagementRabia SaeedNo ratings yet
- Green Hospitals Presentation E-BulletinDocument49 pagesGreen Hospitals Presentation E-BulletinIvan Rangga GunawanNo ratings yet
- Shija Hospital Daily Records - Organizational Study.Document47 pagesShija Hospital Daily Records - Organizational Study.PRK21MS1017 FRANCIS DANY MUKIRI0% (1)
- A Psychoanalyst On The CouchDocument165 pagesA Psychoanalyst On The CouchFrancois RaffoulNo ratings yet
- Oxylog 3000 PlusDocument172 pagesOxylog 3000 PlusrossiNo ratings yet
- App 04 BDocument79 pagesApp 04 Bdoyeonkim21100% (1)
- Analysis of The Patient Transportation Department DilemmaDocument12 pagesAnalysis of The Patient Transportation Department DilemmaJomo MerrittNo ratings yet
- Resume AgDocument2 pagesResume Agapi-342017249No ratings yet
- Communication Barrier Between Nurse and Patient at The Hospital: A Systematic ReviewDocument6 pagesCommunication Barrier Between Nurse and Patient at The Hospital: A Systematic ReviewSilvister MendonsaNo ratings yet
- KetorolacDocument16 pagesKetorolacniken retnoNo ratings yet
- People 360 CVDocument4 pagesPeople 360 CVLey AndeNo ratings yet
- NLE NP1 QuestionsDocument38 pagesNLE NP1 QuestionsLouie John AbilaNo ratings yet
- MOU Templates Combined With Guidance 12.12.14 For Dist FINAL - 0Document6 pagesMOU Templates Combined With Guidance 12.12.14 For Dist FINAL - 0DaniNo ratings yet
- Nursing Practice and The Law 2Document17 pagesNursing Practice and The Law 2'Neil PuzonNo ratings yet
- UNIT 1 I Will Become A MidwifeDocument2 pagesUNIT 1 I Will Become A MidwifeKirana TumiNo ratings yet
- Patricia Ramirez: ProfileDocument2 pagesPatricia Ramirez: Profileapi-195511923No ratings yet
- BMC-Pharmacist-22-10-2023-D ANSWERDocument4 pagesBMC-Pharmacist-22-10-2023-D ANSWERPratyush swarnkarNo ratings yet
- FM 4-02 Health Services Support in CombatDocument189 pagesFM 4-02 Health Services Support in CombatMark Cheney100% (1)
- Workplace Words and Phrases Chinese MandarinDocument6 pagesWorkplace Words and Phrases Chinese MandarinAhmadSandyPerwiraNo ratings yet
- Instillation of Normal Saline in Endotracheal SuctioningDocument2 pagesInstillation of Normal Saline in Endotracheal SuctioningChiyouaLoverz Tharaztic JRsNo ratings yet
- Resume Canada - NurseDocument2 pagesResume Canada - NurseDiana KalengaNo ratings yet
- JoyceDocument48 pagesJoycetinnnnnnnnnnnnnNo ratings yet
- Pain AssessmentDocument3 pagesPain Assessmentapi-363993259No ratings yet
- Running Head - Case Analysis of Reading Rehabilitation HospitalDocument13 pagesRunning Head - Case Analysis of Reading Rehabilitation HospitalashiNo ratings yet
- High Eficency Particular Air Filter: Multizone DopairDocument2 pagesHigh Eficency Particular Air Filter: Multizone DopairarmanNo ratings yet