Professional Documents
Culture Documents
Pamj 24 182 PDF
Uploaded by
Dexter BluesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pamj 24 182 PDF
Uploaded by
Dexter BluesCopyright:
Available Formats
Open Access
Case series
Postoperative analgesia in children when using clonidine in addition to fentanyl with
bupivacaine given caudally
Anouar Jarraya1, Sahar Elleuch1,&, Jawhar Zouari2, Mohamed Smaoui1, Sofiene Laabidi1, Kamel Kolsi1
1
Service dAnesthsie Ranimation, Hpital Hedi Chaker, Sfax, Tunisie, 2Service dAnesthsie Ranimation, Hpital Kremlin, Bictre
&
Corresponding author: Sahar Elleuch, Service dAnesthsie Ranimation, Hpital Hedi Chaker,Sfax,Tunisie
Key words: Caudal epidural, clonidine, fentanyl, pediatric, postoperative analgesia, bupivacaine
Received: 27/02/2015 - Accepted: 25/06/2015 - Published: 01/07/2016
Abstract
The aim of the study was to evaluate the efficacy of clonidine in association with fentanyl as an additive to bupivacaine 0.25% given via single shot
caudal epidural in pediatric patients for postoperative pain relief. In the present prospective randomized double blind study, 40 children of ASA-I-II
aged 1-5 years scheduled for infraumblical surgical procedures were randomly allocated to two groups to receive either bupivacaine 0.25% (1
ml/kg) with fentanyl 1 g/kg and clonidine 1g/kg (group I) or bupivacaine 0.25% (1 ml/kg) with fentanyl 1 g/kg (group II). Caudal block was
performed after the induction of general anesthesia. Postoperatively patients were observed for analgesia, sedation, hemodynamic parameters,
and side effects or complications.Both the groups were similar with respect to patient and various block characteristics. Heart rate and blood
pressure were not different in 2 groups. Significantly prolonged duration of post-operative analgesia was observed in group I (P<0.05). Side
effects such as respiratory depression, vomiting and bradycardia were similar in both groups. The adjunction of clonidine to fentanyl as additives to
bupivacaine in single shot caudal epidural in children may provide better and longer analgesia after infraumblical surgical procedures.
Pan African Medical Journal. 2016; 24:182 doi:10.11604/pamj.2016.24.182.6446
This article is available online at: http://www.panafrican-med-journal.com/content/article/24/182/full/
Sahar Elleuch et al. The Pan African Medical Journal - ISSN 1937-8688. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original
work is properly cited.
Pan African Medical Journal ISSN: 1937- 8688 (www.panafrican-med-journal.com)
Published in partnership with the African Field Epidemiology Network (AFENET). (www.afenet.net)
Page number not for citation purposes 1
Introduction HR or MAP of more than 20 % compared with baseline values
recorded just before surgical incision was considered as adequate
analgesia. An increase in HR or MAP (>20 %), 15 min after
In pediatric patients, caudal epidural is commonly used as it is a
administration of caudal anesthesia (at the time of surgical incision)
safe, reliable, and easy method to administer and is therefore the
was defined as failure of analgesia. In this case, a dose of 20 g/Kg
commonly performed procedure for intra-operative and post-
of alfentanyl was administrated. Patients, in whom caudal
operative analgesia especially for sub-umbilical surgeries in young
anesthesia failed or inadequate analgesia was present, were
children [1,2] . One of the main drawbacks of this technique is the
excluded from study. Time from caudal block to skin incision,
short duration of analgesia even with the use of long-acting local
duration of surgery and duration of general anesthesia was
anaesthetics like bupivacaine and ropivacaine [3]. The success of
recorded as well as demographic parameters (age, weight, size,
achieving prolonged duration of analgesia by the addition of an
gender). In post operative period, pain was assessed using CHEOPS
adjuvant to these local anaesthetics has kept the interest of
Score (Table 1) at H0 (at the admission in the PACU), H1, H2, H4,
anaesthesiologists alive for the search of a new adjuvant. Many
H6, H12 and H24. CHEOPS score at H12 and H24 was assessed by
adjuvants can be used to improve sensory blockade. Epidural
phone because patients leaved the PACU at H6. In the PACU, if
fentanyl has been widely used as analgesic adjuvant. It blocks fibers
patients had CHEOPS score of >7, or if they requested additional
carrying nociceptive impulses in the substantia gelatinosa on the
analgesia they were given 0.2 g/ kg of nalbuphine. After the exit of
dorsal horn of spinal cord [4]. Clonidine can also be given caudally
PACU, all patients were given 15 mg/kg of paracetamol orally 4
and it was shown that it exerts analgesic action by stimulating the
times a day. Side effects like motor blockade, nausea, vomiting,
descending noraderenergic medullospinal pathways and inhibiting
respiratory depression, pruritus, hypotension and bradycardia were
the release of nociceptive neurotransmitters in the dorsal horn of
also noted. Statistical analysis was done using student t-test and
spinal cord [5,6]. Neuraxial administration of clonidine is preferred
chi-square test. P < 0.05 was regarded as statistically significant.
as it has intense analgesic effect because of its spinal site of action
[7,8]. We conducted this study to assess the efficacy of clonidine in
prolonging the action of bupivacaine in association with fentanyl
when used for caudal epidural analgesia in children undergoing sub- Results
umbilical surgeries.
In this prospective randomized study, 40 pediatric patients, 20 in
group I and 20 in group II were included. No case of caudal block
Methods failure was noted and no patient was excluded. Both the groups
were comparable with regard to mean age, weight, gender,
duration of general anesthesia, duration of surgery and time from
After obtaining approval from local ethical committee and written
caudal block to incision (Table 2). In the preoperative period, The
informed consent from parents, 40 ASA I (American Society of
MAP, HR, and SpO2 were similar for both groups (Table 3). We
Anesthesiologists) patients aged 1-5 years, weighing 5-20 kg,
noted no case of caudal block failure and surgical analgesia in both
scheduled to undergo infraumblical surgical procedures such as
the groups was found to be adequate. No patient in either group
hernia repair or orchidopexy were enrolled in this prospective
required intraoperative rescue analgesia. No patient in either group
randomized double blind clinically controlled trial. Children with local
required additional analgesia until 6 hours postoperatively. After 6
infection of the caudal area, history of allergic reactions to local
hours, however, pain score was significantly higher in group II than
anesthetics, coagulopathy, preexisting neurological or spinal
group I (P < 0.05) (Table 4). The complications and side effects
diseases, mental retardation, neuromuscular disorders were
noted were similar in both groups. Residual motor blockade on
excluded from the study. Patients were premedicated with
arrival in PACU was seen in 2 patients in group I and 1 patient in
hydroxyzine 1 mg/kg given orally 2 hours before surgery. All
group II. One patient from each group suffered from vomiting.
patients were given general anesthesia. Anesthesia was induced
Severe complications such as respiratory depression, bradycardia,
with oxygen, nitrous oxide 50% and sevoflurane 6% with
urinary retention and pruritus were not observed in this study.
appropriate size face mask and standard monitoring (heart rate, non
invasive blood pressure and pulse oximetry). After induction of
anesthesia intravenous cannula was placed and I-Gel of appropriate
size introduced for ventilation. Anesthesia was maintained with O2- Discussion
N2O (0.5) and sevoflurane (3%-4%) with assisted respiration with
fresh gas flow of 2L/min. Patients were randomly allocated into one Caudal epidural anesthesia is a simple, frequently used technique,
of the 2 groups by opening sealed envelope. Group I received which provides very effective analgesia intra- and postoperatively in
bupivacaine 0.25% 1 ml/kg with fentanyl 1g/kg and clonidine pediatric patients undergoing infraumbilical surgeries. The search
1g/kg; while Group II received bupivacaine 0.25% 1 ml/kg with for the ideal combination of drugs for caudal anesthesia in pediatric
fentanyl 1g/kg and placebo. Caudal block was given under full patients is on. Efforts are being made to find relatively safer drugs
asepsis with 23G short bevel hypodermic needle in left lateral with minimal side effects. Several adjuvants have been used to
position. Patient was turned supine after administration of the drug. prolong the duration of analgesia of bupivacaine for caudal
The anesthetist in-charge of the patient was completely unaware of analgesia in children. Opioids, ketamine and midazolam are some of
the content of syringes. After closure of skin incision, nitrous oxide the commonly used drugs [9]. The advantage of clonidine is that it
and sevoflurane were discontinued, the I-Gel was removed and prolongs the duration of analgesia without an increase in the
patients were shifted to the post anesthesia care unit (PACU) when incidence of respiratory depression, pruritus and urinary retention
fully awake. Heart rate (HR), mean arterial pressure (MAP) and which are commonly seen with neuraxial opioids. Fentanyl, a
oxygen saturation (SpO2) were recorded before induction of lipophillic opioid is very commonly used as an additive to local
anaesthesia, after induction, before caudal anaesthesia, 10 min anesthetics in children. Although there is no debate about its
after caudal anesthesia and every 10 min thereafter till the patient beneficial effects, side effects like respiratory depression, pruritus,
was shifted to PACU. During intraoperative period adequacy of nausea, and vomiting are common [10]. Clonidine is an alpha-2
analgesia was gauged by hemodynamic stability. Absence of rise of adrenoceptor agonist, which was widely used as an anti-
Page number not for citation purposes 2
hypertensive in 70's and 80's, and presently it has been increasingly
used for sedation, premedication, and as an adjuvant analgesic. It is
also being used as an adjunct to local anesthetic in neuraxial block. Competing interests
Several mechanisms have been suggested for the clonidine-induced
prolongation of caudal analgesia with bupivacaine. The anti-
The authors declare no competing interest.
nociceptive action is due to the direct suppression of the spinal cord
nociceptive neurons by epidural clonidine. Another mechanism is
that clonidine crosses the blood brain barrier and interacts with
alpha 2 adrenoceptors at spinal and supraspinal sites to produce Authors contributions
analgesia. Clonidine also suppresses neurotransmission in peripheral
sensory A and C nerve fibres. The final mechanism suggested is All authors have contributed to this work.
pharmacokinetically mediated: clonidine induces vasoconstriction
through -2b adrenoceptors located at the peripheral vascular
smooth muscles [11]. The successful use of epidural clonidine in Tables
adults led to its evaluation in paediatric caudal epidural block. The
resulting studies have consistently shown caudal clonidine to
increase the duration of postoperative analgesia [11-15]. The main Table 1: CHEOPS score
finding of the present study is that addition of caudal clonidine Table 2: Demographic parameters
prolonged analgesia significantly (p<0.05). There was no significant Table 3: Per-operative parameters
prolongation of motor blockade with addition of clonidine. Table 4: Post-operative CHEOPS Score
Hypotension and bradycardia are expected side effect of extradural
clonidine in adults and depend on the dose administered, however
in children the hemodynamic effects of extradural clonidine are less References
pronounced than in adults [16]. In the present study, regarding
hemodynamics, we did not observe any significant difference in 1. De Beer DA, Thomas ML. Caudal additives in children-solutions
mean heart rate and MAP between the 2 groups, which or problems? Br J Anaesth. 2003 Apr;90(4):487-
corroborated to the study result obtained by Laha A et al [15]. No 98. PubMed | Google Scholar
difference was found regarding post-operative sedation between 2
groups, which matched with other study [13, 14]. Parameswari A et 2. Sethna NF, Berde CB. Pediatric Regional Anesthesia In:
al [11] also showed in his study that clonidine in a dose of 1g/kg, Gregory GA, editor.Pediatric Anesthesia. 4th ed. New York:
added to 0.25% bupivacaine for caudal analgesia and administered Churchill Livingstone Inc; 2003. pp. 267-8. PubMed | Google
as a 1ml/kg mixture in children, for sub-umbilical surgery, Scholar
significantly prolongs the duration of post-operative analgesia when
compared to 1ml/kg of 0.25% bupivacaine alone, without any side 3. Verghese ST, Hannallah RS. Postoperative pain management in
effects. Koul A et al [17] found significant prolongation of post- children. Anesthesiol Clin North America. 2005 Mar;23(1):163-
operative analgesia with an addition of clonidine with bupivacaine 84. PubMed | Google Scholar
caudally. Laha A et al [15] found in a study that the combination of
clonidine (2g/kg) and ropivacaine 0.2% was associated with an 4. Cousins MJ, Mather LE. Intrathecal and epidural administration
improved quality of post-operative analgesia compared to plain of opioids. Anesthesiology. 1984 Sep;61(3):276-
0.2% ropivacaine. 310. PubMed | Google Scholar
5. Cook B, Dayle E. The use of additives to local anaesthetic
Conclusion solutions for caudal epidural blockade.Paediatr anaesth.
1996;6(5):353-9. PubMed | Google Scholar
In conclusion, this study suggests that addition of clonidine
(1g/kg) as an adjuvant with 0.25% bupivacaine and fentanyl 6. Eisenach JC, De Kock M, Klimscha W.alpha (2)-adrenergic
through caudal route increases the duration of post-operative agonists for regional anesthesia: a clinical review of clonidine
analgesia without increasing the incidence of adverse effects. (1984-1995). Anesthesiology. 1996 Sep; 85(3):655-
74. PubMed | Google Scholar
What is known about this topic
7. Bonnet F, Boico O, Rostaing S, Loriferne JF, Saada M.
The success of achieving prolonged duration of analgesia Clonidine-induced analgesia in postoperative patients: Epidural
by the addition of an adjuvant to these local anaesthetics versus intramuscular administration. Anesthesiology. 1990 Mar;
has kept the interest of anaesthesiologists alive for the 72(3):423-7. PubMed | Google Scholar
search of a new adjuvant. Many adjuvants can be used to
improve sensory blockade; 8. Eisenach J, Detweiter D, Hood D. Haemodynamic and analgesic
The addition of clonidine (1g/kg) as an adjuvant with action of epidurally administered clonidine. Anesthesiology.
0.25% bupivacaine through caudal route increases the 1993 Feb; 78(2):277-87. PubMed | Google Scholar
duration of post-operative analgesia.
9. Vetter TR, Carvallo D, Johnson JL, Mazurek MS, Presson RG Jr.
What this study adds A comparison of single-dose caudal clonidine, morphine, or
This study suggests that addition of clonidine (1g/kg) as hydromorphone combined with ropivacaine in pediatric patients
an adjuvant with 0.25% bupivacaine and fentanyl through undergoing ureteral reimplantation. Anesth Analg. 2007
caudal route increases the duration of post-operative Jun;104(6):1356-63. PubMed | Google Scholar
analgesia without increasing the incidence of adverse
effects.
Page number not for citation purposes 3
10. Campbell FA, Yentis SM, Fear DW, Bissonnette B. Analgesic 14. Bajwa SJ, Kaur J, Bajwa SK, Bakshi G, Singh K, Panda A.
efficacy and safety of a caudal bupivacaine-fentanyl mixture in Caudal ropivacaine clonidine: A better post-operative analgesic
children. Can J Anaesth. 1992 Sep;39(7):661- approach.Indian J Anaesth. 2010 May;54(3):226-
4. PubMed | Google Scholar 30. PubMed | Google Scholar
11. Parameswari A, Dhev AM, Vakamudi M. Efficacy of clonidine as 15. Laha A, Ghosh S, Das H. Comparison of caudal analgesia
an adjuvant to bupivacaine for caudal analgesia in between ropivacaine and ropivacaine with clonidine in children:
childrenundergoing sub-umbilical surgery. Indian J Anaesth. A randomized controlled trial. Saudi J Anaesth. 2012
2010 Sep;54(5):458-63. PubMed| Google Scholar Jul;6(3):197-200. PubMed |Google Scholar
12. De Negri P, Ivani G, Visconti C, de Vivo P. How to prolong 16. Shukla U, Prabhakar T, Malhotra K. Postoperative analgesia in
postoperative analgesia after caudal anaesthesia with children when using clonidine or fentanyl with ropivacaine
ropivacaine in children: S-ketamine versus clonidine. Paediatr given caudally. J Anaesthesiol Clin Pharmacol. 2011
Anaesth. 2001 Nov;11(6):679-83.PubMed | Google Scholar Apr;27(2):205-10. PubMed | Google Scholar
13. Ivani G, De Negri P, Conio A et al. Ropivacaine-clonidine 17. Koul A, Pant D, Sod J. Caudal Clonidine in Day-Care Paediatric
combination for caudal blockade in children. Acta Anaesthesiol Surgery. Indian J Anaesth. 2009 Aug;53(4):450-
Scand. 2000 Apr;44(4):446-9. PubMed | Google Scholar 4. PubMed | Google Scholar
Table 1: Childrens Hospital Eastern Ontario Pain Scale (CHEOPS) (recommended for children 1-7 years old) - a score greater than 4
indicates pain
Item Behavioral Definition Score
Cry No cry 1 Child is not crying
Moaning 2 Child is not moaning or quietly vocalizing silent cry
Crying 2 Child is crying, but the cry is gentle or whimpering
Scream 3 child is in a full-lunged cry; sobbing may be scored with complaint or without complaint
Facial Composed 1 Neutral facial expression
Grimace 2 Score only if definite negative facial expression
Smiling 0 score only if definite negative facial expression
Child None 1 Child not talking
verbal
Other complaints 1 Child complains but not about pain ("I want to see mommy: or "I am thirsty")
Pain complaints 2 Child complains about pain
Both complaints 2 child complains about pain and about other things (e.g. It hurts; I want mommy.)
Positive 0 Child makes any positive statement or talks about other things without complaint
Torso Neutral 1 Body (not limbs) is at rest; torso is inactive
Shifting 2 Body is in motion in a shifting or serpentine fashion
Tense 2 Body is arched or rigid
Shivering 2 Body is shuddering or shaking involuntarily
Upright 2 Child is in a vertical or upright position
Restrained 2 Body is restrained
Touch Not touching 1 Child is not touching or grabbing at wound
Reach 2 Child is reaching for but not touching wound
Touch 2 Child is gently touching wound or wound area
Grab 2 Child is grabbing vigorously at wound
Restrained: 2 Child's arms are restrained
Legs Neutral 1 Legs may be in any position but are relaxed; includes gently swimming or separate-like
movements
Squirm/ kicking: 2 Definitive uneasy or restless movements in the legs and/or striking out with foot or feet
Drawn up/tensed 2 Legs tensed and/or pulled up tightly to body and kept there
Standing 2 Standing crouching or kneeling
Restrained 2 child's legs are being held down
Page number not for citation purposes 4
Table 2: demographic parameters
Parameters Group I Group II P value
Age (months) 29.1 2.4 31.2 2.2 0.751
Weight (Kg) 12.7 0.8 13.5 1.1 0.665
Gender (M/F) 18 / 2 20 /0
Duration of surgery (min) 38.5 6.5 37.1 7.1 0.633
Duration of anesthesia (min) 45 12 42 4 0.398
Time from caudal block to skin incision 92 9.5 2 0.273
(min)
Table 3: per-operative parameters
- Ti T0 T5 T15 T25 T35 Tpo
HR Group I 13323 13013 1269 12012 11911 1277 1284
Group II 1249 11914 11311 1138 10912 11911 1278
P value 0.140 0.158 0.131 0.337 0.184 0.254 0.88
Group I 57 16 56 17 4811 4611 478 489 445
MAP GroupII 56 6 60 8 518 518 508 499 489
P value 0.796 0.198 0.441 0.170 0.199 0.747 0.075
HR : heart rate; MAP : mean arterial pressure;Ti : before the anesthesia induction;T0 : at the moment of induction; T5 : at
the moment of caudal block;T15 : 10 minutes after caudal block;
T25: 25 minutes after induction; T35: 35 minutes after induction;T po : after the end of the intervention.
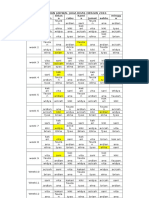
Table 4: post-operative CHEOPS Score
- H0 H1 H2 H4 H6 H12 H24
Group I 5.2 1.5 4.50.5 5.00.45 5.50.5 5.40.7 5.81 7.10.57
Group II 5.8 0.6 6.30.5 5.5 0.5 6.50.5 6.50.5 7.10.8 7.60.52
P value 0.288 0.001 0.001 0.001 0.001 0.011 0.091
H0: at the entry in PACU; H1: at the 1st post-operative hour; H2: at the 2nd post-operative hour;
H4: at the 4th post-operative hour H6: at the 6th post-operative hour; H12: at the 12th post-operative hour; H24: at the
24th post-operative hour
Page number not for citation purposes 5
You might also like
- Benefits and Risks of Antiretroviral TherapyDocument12 pagesBenefits and Risks of Antiretroviral TherapyAtgy Dhita AnggraeniNo ratings yet
- Ulkus Kornea Eng VerDocument15 pagesUlkus Kornea Eng VerDexter BluesNo ratings yet
- Activation of mTOR: A Culprit of Alzheimer's Disease?: Neuropsychiatric Disease and Treatment DoveDocument16 pagesActivation of mTOR: A Culprit of Alzheimer's Disease?: Neuropsychiatric Disease and Treatment Dovemr dexterNo ratings yet
- Jurnal Anak RirinDocument10 pagesJurnal Anak RirinDexter BluesNo ratings yet
- PRM2016 1658172 PDFDocument7 pagesPRM2016 1658172 PDFDexter BluesNo ratings yet
- SDJ 2016 09 01 PDFDocument7 pagesSDJ 2016 09 01 PDFDexter BluesNo ratings yet
- Nejmoa1514762 PDFDocument12 pagesNejmoa1514762 PDFDexter BluesNo ratings yet
- Nejmoa1606356 PDFDocument10 pagesNejmoa1606356 PDFDexter BluesNo ratings yet
- The Seven Cardinal MovementsDocument4 pagesThe Seven Cardinal MovementsDexter BluesNo ratings yet
- Childhood IQ and Bipolar Link PDFDocument9 pagesChildhood IQ and Bipolar Link PDFDexter BluesNo ratings yet
- Jurnal Anak Ririn PDFDocument10 pagesJurnal Anak Ririn PDFDexter BluesNo ratings yet
- Referat Obgyn FixDocument29 pagesReferat Obgyn FixDexter BluesNo ratings yet
- QuestionsDocument1 pageQuestionsDexter BluesNo ratings yet
- Medi 96 E5795 PDFDocument5 pagesMedi 96 E5795 PDFDexter BluesNo ratings yet
- The Seven Cardinal MovementsDocument4 pagesThe Seven Cardinal MovementsDexter BluesNo ratings yet
- Fix ObgynDocument17 pagesFix ObgynDexter BluesNo ratings yet
- Unchallengeable Miracles of QuranDocument430 pagesUnchallengeable Miracles of QuranyoursincerefriendNo ratings yet
- Clinical Guidelines Acute Rehab Management 2010 InteractiveDocument172 pagesClinical Guidelines Acute Rehab Management 2010 InteractivenathanaelandryNo ratings yet
- Rincian Jadwal Jaga Koas Obsgin 2016 Senin Selas A Rabu Kami S Jumat Sabtu Mingg UDocument1 pageRincian Jadwal Jaga Koas Obsgin 2016 Senin Selas A Rabu Kami S Jumat Sabtu Mingg UDexter BluesNo ratings yet
- 1830 PDF PDFDocument5 pages1830 PDF PDFDexter BluesNo ratings yet
- TSWJ2015 803752 PDFDocument8 pagesTSWJ2015 803752 PDFDexter BluesNo ratings yet
- Childhood IQ and Bipolar Link PDFDocument9 pagesChildhood IQ and Bipolar Link PDFDexter BluesNo ratings yet
- The Seven Cardinal MovementsDocument3 pagesThe Seven Cardinal MovementsMaria Mandid0% (1)
- Referat Obgyn FixDocument29 pagesReferat Obgyn FixDexter BluesNo ratings yet
- Mood Dynamics in Bipolar Disorder: Research Open AccessDocument9 pagesMood Dynamics in Bipolar Disorder: Research Open AccesswulanfarichahNo ratings yet
- Pruritus: An Updated Look at An Old ProblemDocument7 pagesPruritus: An Updated Look at An Old ProblemThariq Mubaraq DrcNo ratings yet
- Geriatric Itch PDFDocument16 pagesGeriatric Itch PDFDexter BluesNo ratings yet
- Jurnal Elderly 2 PDFDocument3 pagesJurnal Elderly 2 PDFDexter BluesNo ratings yet
- 10 4103@0378-6323 116725 PDFDocument14 pages10 4103@0378-6323 116725 PDFDexter BluesNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Typhoid FeverDocument9 pagesTyphoid FeverAli Al.JuffairiNo ratings yet
- Genie Z45.25 J Internal Combustion - Service Manual - Part No. 219418Document331 pagesGenie Z45.25 J Internal Combustion - Service Manual - Part No. 219418marciogianottiNo ratings yet
- ICH Topic Q 3 B (R2) Impurities in New Drug Products: European Medicines AgencyDocument14 pagesICH Topic Q 3 B (R2) Impurities in New Drug Products: European Medicines AgencyJesus Barcenas HernandezNo ratings yet
- PPEsDocument11 pagesPPEsPrithivirajan CuddaloreNo ratings yet
- Explorations in PersonalityDocument802 pagesExplorations in Personalitypolz2007100% (8)
- 01 Basic Design Structure FeaturesDocument8 pages01 Basic Design Structure FeaturesAndri AjaNo ratings yet
- Z160-250 Instruction ManualDocument182 pagesZ160-250 Instruction ManualNMA Industrial ServicesNo ratings yet
- GEK_30375M Lubrication SpecificationsDocument34 pagesGEK_30375M Lubrication SpecificationsMARITZA GABRIELA ARIZABAL MEDINANo ratings yet
- Inspection and Repair of Aircraft Integral Tanks AND Fuel CellsDocument222 pagesInspection and Repair of Aircraft Integral Tanks AND Fuel CellsgnanasekarNo ratings yet
- Crypto Hash Algorithm-Based Blockchain Technology For Managing Decentralized Ledger Database in Oil and Gas IndustryDocument26 pagesCrypto Hash Algorithm-Based Blockchain Technology For Managing Decentralized Ledger Database in Oil and Gas IndustrySIMON HINCAPIE ORTIZNo ratings yet
- 2008 Annual Debt StatementDocument12 pages2008 Annual Debt StatementEwing Township, NJNo ratings yet
- NCL ReportDocument20 pagesNCL ReportSwati Tripathi33% (3)
- PreparationDocument2 pagesPreparationmghaffarzadehNo ratings yet
- Fire & Gas Design BasisDocument2 pagesFire & Gas Design BasisAdil MominNo ratings yet
- Chapter Test A: Teacher Notes and Answers 17Document5 pagesChapter Test A: Teacher Notes and Answers 17Mmf 123 JanNo ratings yet
- Understand TSGLI BenefitsDocument2 pagesUnderstand TSGLI BenefitsJoseph LawerenceNo ratings yet
- CAPE Biology 2006 U2 P1 PDFDocument28 pagesCAPE Biology 2006 U2 P1 PDFvedant seerattanNo ratings yet
- Teardrop by Lauren KateDocument47 pagesTeardrop by Lauren KateRandom House Teens88% (16)
- MSDS Summary: Naphtha VM&PDocument6 pagesMSDS Summary: Naphtha VM&PRizki Adwitiyo 'Dito'No ratings yet
- 16-Bit UUID Numbers DocumentDocument28 pages16-Bit UUID Numbers DocumentJuan M Iñiguez RNo ratings yet
- Rtaa SB 4 - 10011991Document6 pagesRtaa SB 4 - 10011991alcomech100% (3)
- Round Warre HivesDocument16 pagesRound Warre HivesBender Rodríguez100% (1)
- Nigeria Trainers ManualDocument131 pagesNigeria Trainers ManualVivi ALNo ratings yet
- RRL CapstoneDocument3 pagesRRL CapstoneMatthew Dane SitoNo ratings yet
- PositionsDocument4 pagesPositionsMixsz LlhAdyNo ratings yet
- Bed MakingDocument14 pagesBed MakingHarold Haze Cortez100% (1)
- Marital Rape in IndiaDocument8 pagesMarital Rape in IndiaSHUBHANK SUMANNo ratings yet
- 5 Ethiopian - National - Healthcare - Quality - and - Safety - Strategy - Final - Draft-July122021Document86 pages5 Ethiopian - National - Healthcare - Quality - and - Safety - Strategy - Final - Draft-July122021Kemal MahmoudNo ratings yet
- Jobaid Investigating Causes PDFDocument16 pagesJobaid Investigating Causes PDFNina MarianaNo ratings yet