Professional Documents
Culture Documents
Cutaneous Larva Migran
Uploaded by
giviCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cutaneous Larva Migran
Uploaded by
giviCopyright:
Available Formats
Case report
Cutaneous larva migrans syndrome: a case report
Emilia Tekely, Beata Szostakiewicz, Bartomiej Wawrzycki, Grayna Kdziela-Wypyska, Maria Juszkiewicz-Borowiec,
Aldona Pietrzak, Grayna Chodorowska
Department of Dermatology, Venereology and Peadiatric Dermatology, Medical University of Lublin, Poland
Head: Prof. Grayna Chodorowska MD, PhD
Postep Derm Alergol 2013; XXX, 2: 119121
DOI: 10.5114/pdia.2013.34164
Abstract
Cutaneous larva migrans (CML) is a frequent parasitic infestation caused by migration of animal hookworm larvae
into the human epidermis. This skin disease is common in warmer climates among people, who have contact with
contaminated soil. Clinical manifestation of CML is an itchy, erythematous, linear tract, which appears days to even
months after exposure to infested sand or soil. Diagnosis is established on the clinical presentation. We describe
a case of CML acquired during a holiday in Brazil.
Key words: creeping eruption, cutaneous larva migrans, hookworm infection.
Introduction
Cutaneous larva migrans (CML) also known as creep- parasitic penetration a red itchy papule may be noticed,
ing eruption is one of the most frequent skin diseases which with time raises above the skin surface [10, 13, 14].
among travelers returning from tropical countries [1-4]. Cuta- As the larva migrates a linear wandering erythema, that
neous larva migrans is caused by incidental infestation of is clearly separated from its surrounding, appears [1-3, 6,
a human by animal nematode larvae usually thriving dogs 8, 11, 13]. The tunnels left by the migrating parasite des-
and cats [1, 2, 4-16]. The parasites are found mostly in trop- iccate and are covered with a scab [13]. It is worth notic-
ical and subtropical regions like the Caribbean, South and ing that the nematode may survive in the skin for many
Central America, Southern-East Asia and Africa [6, 9, 10, months [2, 4, 5, 10, 12, 14].
11, 13]. The most common parasite species causing creep- We report a case of cutaneous larva migrans on the right
ing eruption are Ancylostoma braziliense, Ancylostoma can- foot, in a 2-year-old Polish girl, who returned from a trip
inum, Necator americanus, Uncinaria stenocephala and to Brazil.
Strongyloides stenocephala [5, 7-9, 13, 14]. The parasite
infects a human through the penetration of undamaged
skin. Commonly affected sites include feet, thighs and but- Case report
tocks but any part of the body, which has direct contact A 2-year-old girl was presented to our Department in
with contaminated and wet soil e.g. on beaches or in sand- May 2011 because of linear wandering erythema, which
pits, can be involved [2, 4, 6, 10, 12-16]. Nematode larvae appeared on the girls right heel. A few days earlier the girls
in an incidental human host do not complete their full life mother had noticed an itchy reddened spot in the form of
cycle, but stay confined to the epidermis and less often the a papule on the right foot. The lesion had been rapidly
upper dermis [1, 2, 4, 5, 7-11, 13-15]. The parasite migrates increasing in size forming a serpiginous erythema and pru-
at the rate of a few millimeters to a few centimeters per ritus had become more intense. Examination revealed
day forming a tortuous, serpiginous tunnel rising above the a slightly raised erythematous serpentine lesion and
skin surface with a length of a few to even more than 10 cm a local edema on the right foot (Figures 1 and 2). During
[3, 6-8, 12-14, 17]. The parasite migration causes severe pru- the examination, the patients mother informed us of their
ritus, which often leads to epidermal damage and sec- recent trip to a hot zone country (Brazil) from which they
ondary infections [1-7, 10, 11, 13, 14]. Initially, at the site of had returned a week before.
Address for correspondence: Emilia Tekely MD, Department of Dermatology, Venereology and Peadiatric Dermatology,
Medical University of Lublin, 13 Radziwiowska St, 20-080 Lublin, Poland, phone: +48 81 532 36 47, e-mail: emiliatekely@wp.pl
Received: 10.01.2013, accepted: 28.02.2013.
Postpy Dermatologii i Alergologii XXX; 2013/2 119
E. Tekely, B. Szostakiewicz, B. Wawrzycki, G. Kdziela-Wypyska, M. Juszkiewicz-Borowiec, A. Pietrzak, G. Chodorowska
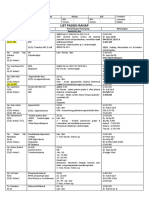
Figure 2. Local edema with slighty raised erythematous ser-
Figure 1. Linear wandering erythema on the right heel pentine lesion on the right foot
Peripheral blood analysis and total IgE level were with- tact with soil or sand contaminated by feces of infected
in normal ranges. Parasitological examination of feces was animals are affected. In a warm, humid environment, nema-
negative. The location and characteristic presentation of tode larvae can survive and be infective for several weeks
linear serpiginous skin lesions on the right foot as well as or even several months. Due to the fact that humans are
the patients stay in the South America made it possible accidental hosts the parasites are unable to complete their
to diagnose her with cutaneous larva migrans syndrome. life cycle. The larvae secrete protease and hyaluronidase,
The girl was also referred to the Outpatient Clinic of Child which facilitate the penetration through epidermis to
Infectious Diseases, where the diagnosis of CML was con- achieve internal organs [4, 7, 14]. Hence, a raised, prurit-
firmed. ic, erythematous, linear track, which appears usually
The patient was treated with oral albendazole (200 mg/ a few days after infestation, is a typical clinical manifes-
day for 3 days) and freezing the leading edge of the cuta- tation. In most cases, the diagnosis of cutaneous larva
neous track with solid carbon dioxide. Due to severe pru- migrans is based on the typical skin findings and the pre-
ritus the girl received also oral and topical antihistamine vious travel history with a real possibility of exposure
drugs, i.e. desloratadine (2.5 mg/day for 3 days) and di- [2, 3, 6, 8, 14-16]. One should be aware of the presence of
metindene applied on her right foot. A few hours after the atypical clinical presentation of CML. This knowledge can
freezing session numerous wheals were noticed and prevent misdiagnosis, which often leads to insufficient or
therefore the patient received dexamethasone i.m. for delayed treatment.
3 consecutive days. The lesion totally disappeared with- Uncommon clinical presentations of CML include
in a few days after treatment was initiated. [2, 4, 13, 14, 17]:
hair follicle inflammation known as hookworm folliculitis
most frequently in the buttocks area,
Discussion diffuse multifocal papulo-vesicular eruption localized
One of the most frequent helminthic infections among mainly on the chest, back and abdomen,
travelers returning from tropical and subtropical regions migrating urticaria.
of the world is cutaneous larva migrans. This tropically The complications of cutaneous larva migrans include
acquired dermatosis was described for the first time in the secondary bacterial infections, local or general allergic reac-
19th century [14]. Cutaneous larva migrans is caused by acci- tions and very rarely parasites migration to internal
dental, percutaneous migration of animal hookworm lar- organs [2, 7, 10, 11, 13].
vae within the human skin. Ancylostoma braziliense is one Effective treatment of hookworm-related CML is based
of the most common species in tropical and subtropical on oral or topical antihelminthics. Ivermectin, albendazole
regions, which affects people of all ages. Lesions are locat- and tiabendazole are drugs, which are acceptable for sys-
ed on the feet, legs and buttocks in the adults while chil- temic treatment. First-line treatment are ivermectin and
dren can be infected also on the genitals and hands [16]. albendazole. Ivermectin is well tolerated and highly effec-
In most instances, the skin areas, which have direct con- tive but contraindicated in children younger than 5 years
120 Postpy Dermatologii i Alergologii XXX; 2013/2
Cutaneous larva migrans syndrome: a case report
[14]. It is taken at a single dose of 200 g/kg, while the aver- 15. Roest MAB, Ratnavel R. Cutaneous larva migrans contracted
age dose is 12 mg. Albendazole is also efficient at a daily in England: a reminder. Clin Exp Dermatol 2001; 26: 389-90.
dosage between 400 mg and 800 mg for 1 to 7 days. Thi- 16. Black MD, Grove DI, Butcher AB, et al. Cutaneous larva migrans
in infants in the Adelaide Hills. Australas J Dermatol 2010; 51:
abendazole is not recommended because of a relatively high
281-4.
incidence of the following side effects: dizziness, nausea, 17. Veraldi S, Bottini S, Carrera C, et al. Cutaneous larva migrans
vomiting and intestinal cramps [6, 7, 14]. In cases when oral with folliculitis: a new clinical presentation of this infection.
drugs are contraindicated, ointments with 10% albenda- JEADV 2005; 19: 628-30.
zole or 10-15% thiabendazole should be considered [18]. 18. Caumes E. Efficacy of albendazole ointment on cutaneous lar-
Topical application of ointment 3 times daily for 5 to 10 days va migrans in 2 young children. CID 2004; 38: 1647-8.
on the affected skin is comparable to the oral treatment
for CML [14, 18]. Nowadays, physical modalities such as
cryotherapy with carbon dioxide or liquid nitrogen are used
in exceptional cases [1, 8, 11, 13, 15]. The response to an anti-
helmintic drug and rapid resolution of the lesion confirmed
the initial diagnosis of cutaneous larva migrans [13, 15].
Traveling has become accessible and universal among
people in the world leading to an increase in the number
of tropical dermatosis e.g. cutaneous larva migrans.
Nowadays, health education should be focused on tourists,
who are planning a trip to hot zone countries, endemic areas
for CML. They should be advised to wear shoes in sandy
areas, to use deckchairs or mattresses on beaches and to
avoid beaches where animals are present.
References
1. Caumes E. Treatment of cutaneous larva migrans. CID 2000;
30: 811-4.
2. Perman MJ. 10-year old boy present with a pruritic, blister-
ing eruption. Infectious Disease News 2010; 23: 18.
3. Gutte R, Khopkar U. Cutaneous larva migrans (creeping erup-
tion). Indian Dermatol Online J 2011; 2: 48.
4. Malvy D, Ezzedine K, Pistone T, et al. Extensive cutaneous lar-
va migrans with folliculitis mimicking multimetameric her-
pes zoster presentation in an adult traveler returning from
Thailand. J Travel Med 2006; 13: 244-7.
5. Jackson A, Heukelbach J, Calheiros CML, et al. A study in a com-
munity in Brazil in which cutaneous larva migrans is endem-
ic. CID 2006; 43: 8-13.
6. Lesniak R. Cutaneous larva migrans. Dermatol Nurs 2008; 6:
471-2.
7. Blackwell V, Vega-Lopez F. Cutaneous larva migrans: clinical
features and management of 44 cases presenting in the
returning traveler. Br J Dermatol 2001; 145: 434-7.
8. French SJ, Lindo JF. Severe cutaneous larva migrans in trav-
eler to Jamaica, West Indies. J Travel Med 2003; 10: 249-50.
9. Kienast A, Bialek R, Hoeger PH. Cutaneous larva migrant in
northern Germany. Eur J Pediatr 2007; 166: 1183-5.
10. Yavuzer K, Ak M, Karadag AS. A case report of cutaneous lar-
va migrans. EAJM 2010; 42: 40-1.
11. Watkins J. Cutaneous larva migrans: diagnosis and man-
agement. British Journal of School Nursing 2009; 7: 325-7.
12. Siriez JY, Angoulvant F, Buffet P, et al. Individual variability of
the cutaneous larva migrans (CML) incubation period. Pedi-
atr Dermatol 2010; 2: 211-2.
13. Kacprzak E, Silny W. Cutaneous larva migrans syndrome in
travelers returning from warm climate countries. Postep Derm
Alergol 2004; XXI: 24-9.
14. Heukelbach J, Feldmeier H. Epidemiological and clinical
characteristics of hookworm-related cutaneous larva migrans.
Lancet Infect Dis 2008; 8: 302-9.
Postpy Dermatologii i Alergologii XXX; 2013/2 121
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- English 2.2 FPT PolytechnicDocument10 pagesEnglish 2.2 FPT PolytechnicKieu Mai Trang (FPL HCM)0% (1)
- (Salim Ross) PUA 524 - Introduction To Law and The Legal System (Mid Term)Document4 pages(Salim Ross) PUA 524 - Introduction To Law and The Legal System (Mid Term)Salim RossNo ratings yet
- Ijerph 19 09026Document36 pagesIjerph 19 09026giviNo ratings yet
- International Journal of Surgery: Emma J. Noble, Ros Harris, Ken B. Hosie, Steve Thomas, Stephen J. LewisDocument6 pagesInternational Journal of Surgery: Emma J. Noble, Ros Harris, Ken B. Hosie, Steve Thomas, Stephen J. LewisChristopher AdhisasmitaNo ratings yet
- MSL 2019 68Document10 pagesMSL 2019 68giviNo ratings yet
- 496 1971 1 PBDocument16 pages496 1971 1 PBaliNo ratings yet
- Refleksi Kasus VesicolitiasisDocument14 pagesRefleksi Kasus VesicolitiasisgiviNo ratings yet
- List Pasien Ranap: Tanggal: 24 November 2021 Dokter: GiviDocument18 pagesList Pasien Ranap: Tanggal: 24 November 2021 Dokter: GivigiviNo ratings yet
- Asamrew (2020) Level of Patient Satisfaction With Inpatient Services and Its Determinants A Study of A Specialized Hospital in EthiopiaDocument12 pagesAsamrew (2020) Level of Patient Satisfaction With Inpatient Services and Its Determinants A Study of A Specialized Hospital in EthiopiaDiego RiveraNo ratings yet
- MSL 2019 68Document10 pagesMSL 2019 68giviNo ratings yet
- Ijerph 19 09026Document36 pagesIjerph 19 09026giviNo ratings yet
- Tanggal: Nama KaryawanDocument1 pageTanggal: Nama KaryawangiviNo ratings yet
- Data by Name Lansia Desa TambakDocument41 pagesData by Name Lansia Desa TambakgiviNo ratings yet
- High Myopia JournalDocument7 pagesHigh Myopia JournalindahpratiwiindraNo ratings yet
- Jadwal QR Bulan AprilDocument12 pagesJadwal QR Bulan AprilgiviNo ratings yet
- Hasil Nilai Pre Post TestDocument1 pageHasil Nilai Pre Post TestgiviNo ratings yet
- Morikawa2016Document6 pagesMorikawa2016giviNo ratings yet
- Data Desbin ExcelDocument125 pagesData Desbin ExcelGindy AuliaNo ratings yet
- Jurnal 3Document13 pagesJurnal 3giviNo ratings yet
- Jurnal 3Document8 pagesJurnal 3giviNo ratings yet
- Jurnal 3Document7 pagesJurnal 3giviNo ratings yet
- Jurnal 2Document9 pagesJurnal 2giviNo ratings yet
- 2 PDFDocument7 pages2 PDFgiviNo ratings yet
- Jurnal 3Document7 pagesJurnal 3giviNo ratings yet
- Jurnal Obgyn 1 PDFDocument8 pagesJurnal Obgyn 1 PDFgiviNo ratings yet
- Jurnal GynDocument6 pagesJurnal GyngiviNo ratings yet
- 89 1473095747Document6 pages89 1473095747giviNo ratings yet
- Jurnal Obgyn 1 PDFDocument8 pagesJurnal Obgyn 1 PDFgiviNo ratings yet
- Jurnal GynDocument6 pagesJurnal GyngiviNo ratings yet
- Jurnal GynDocument6 pagesJurnal GyngiviNo ratings yet
- Iwwusa Final Report IdsDocument216 pagesIwwusa Final Report IdsRituNo ratings yet
- Repair Max II Pump 310894lDocument20 pagesRepair Max II Pump 310894lAndreina FajardoNo ratings yet
- 1.9 Bernoulli's Equation: GZ V P GZ V PDocument1 page1.9 Bernoulli's Equation: GZ V P GZ V PTruong NguyenNo ratings yet
- Harajuku: Rebels On The BridgeDocument31 pagesHarajuku: Rebels On The BridgeChristian Perry100% (41)
- RCC Lintel and Slab PlanDocument3 pagesRCC Lintel and Slab PlanSaurabh Parmar 28No ratings yet
- Gardiner 1979Document16 pagesGardiner 1979Oswaldo Manuel Ramirez MarinNo ratings yet
- JASA SREVIS LAPTOP Dan KOMPUTERDocument2 pagesJASA SREVIS LAPTOP Dan KOMPUTERindimideaNo ratings yet
- Implementing a JITD system to reduce bullwhip effect and inventory costsDocument7 pagesImplementing a JITD system to reduce bullwhip effect and inventory costsRaman GuptaNo ratings yet
- Atomic Structure - One Shot by Sakshi Mam #BounceBackDocument231 pagesAtomic Structure - One Shot by Sakshi Mam #BounceBackchansiray7870No ratings yet
- Slope Stability Analysis MethodsDocument5 pagesSlope Stability Analysis MethodsI am AngelllNo ratings yet
- Quality of Good TeacherDocument5 pagesQuality of Good TeacherRandyNo ratings yet
- Chair Locker Provides Storage and Space SavingsDocument32 pagesChair Locker Provides Storage and Space SavingsElza S. GapuzNo ratings yet
- New Wordpad DocumentDocument6 pagesNew Wordpad DocumentJonelle D'melloNo ratings yet
- Purnanandalahari p3D4Document60 pagesPurnanandalahari p3D4anilkumar100% (1)
- Stress-Busting Plan for Life's ChallengesDocument3 pagesStress-Busting Plan for Life's Challengesliera sicadNo ratings yet
- Advanced Financial Accounting Chapter 2 LECTURE - NOTESDocument14 pagesAdvanced Financial Accounting Chapter 2 LECTURE - NOTESAshenafi ZelekeNo ratings yet
- Psyclone: Rigging & Tuning GuideDocument2 pagesPsyclone: Rigging & Tuning GuidelmagasNo ratings yet
- ATB Farmacología 2Document194 pagesATB Farmacología 2Ligia CappuzzelloNo ratings yet
- Learn R For Applied StatisticsDocument457 pagesLearn R For Applied StatisticsyasortyNo ratings yet
- Good Evil EssayDocument2 pagesGood Evil EssayuniquebythemillionsNo ratings yet
- Family Culture and Traditions PaperDocument7 pagesFamily Culture and Traditions PaperAmit JindalNo ratings yet
- ZO 503 Physiological Chemistry by Dr.S.S.KunjwalDocument22 pagesZO 503 Physiological Chemistry by Dr.S.S.KunjwalAbhishek Singh ChandelNo ratings yet
- Case Study No. 11 - Hydroelectric Power Plant in The PhilippinesDocument26 pagesCase Study No. 11 - Hydroelectric Power Plant in The PhilippinespicefeatiNo ratings yet
- 2017 Grade 9 Math Challenge OralsDocument3 pages2017 Grade 9 Math Challenge OralsGracy Mae PanganibanNo ratings yet
- Polifur 1K Synthetic Top Coat MSDS Rev 2 ENDocument14 pagesPolifur 1K Synthetic Top Coat MSDS Rev 2 ENvictorzy06No ratings yet
- The Issue of Body ShamingDocument4 pagesThe Issue of Body ShamingErleenNo ratings yet
- Ezequiel Reyes CV EngDocument1 pageEzequiel Reyes CV Engezequiel.rdNo ratings yet
- Douglas Frayne Sargonic and Gutian Periods, 2334-2113 BCDocument182 pagesDouglas Frayne Sargonic and Gutian Periods, 2334-2113 BClibrary364100% (3)