Professional Documents
Culture Documents
Careplan Weebly 1
Uploaded by
api-379909348Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Careplan Weebly 1
Uploaded by
api-379909348Copyright:
Available Formats
Careplan
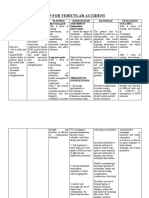
NURSING DIAGNOSES EXPECTED PATIENT ASSESSMENT interventions: ACTION interventions: TEACHING interventions:
OUTCOMES (S. M. A. R. T.)
Constipation r/t weakness Pt will increase fluid intake -Assess usual pattern of -Nurse will provide pt -Teach pt to eat a
of muscles, inadequate by drinking 1.5 to 2 L of defecation, including time of with 100g of prune healthy diet with
fluid intake, decreased water daily while awake for 7 day, amount, consistency and juice daily to adequate intake of whole
autonomic nervous system days ending on 11/01/2017. frequency of stool. incorporate fiber, grains and fiber.
activity AEB Parkinsons sorbitol, and
Disease, pt drinking only -Evaluate all the medications polyphenol into pts -Teach pt keep a 7-day
720 mL of fluid in 8 hours pt is taking in order to diet and promote a diary of bowel habits to
despite being reminded, pt determine if one could have laxative effect. include date/time, length
stated my legs get sore adverse effect of constipation of time on toilet,
easily, and pt not and monitor pts water jug -Encourage pt to do consistency,
defecating in over 24 level in room to see how much physical activity like amount/frequency of
hours. they usually are drinking. walking the halls and stool, and any straining
Monitor pt fluid intake during doing waist twists. to promote pt adherence
meals too. and understanding.
-Nurse will
administer laxative or -Teach pt how to adopt
BRC bowel protocol the best posture for
drugs PRN. defecationkeep knees
slightly higher than hips,
feet flat on the floor, and
lean forward with elbows
on knees.
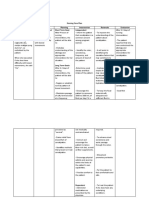
Risk for injury r/t tremors Pt stand up and hold onto -Monitor pts ability to -Nurse will monitor -Teach pt to do deep
in hands and legs, fatigue Rolling Walker while doing tolerate activity and use all 4 the pt while breathing exercises to
after therapy twisting side stretches/ extremities noting pulse, skin performing her help with lung expansion
sessions/walking the reaches for a minimum of 2 color, and B/P before and standing and and to help relieve pts
hallways, slowed reactions minutes three times a day at after PT sessions and while stretching exercise anxiety/ tremor intensity/
while using RW assistive 0930, 1300, and 2030 for 7 doing independent transfers. for 2 minutes three fatigue when ambulating.
times a day to ensure
device, and altered gait days ending on 11/01/2017.
-Assess pt room for any pt performs task. -Teach pt to stand up
(Parkinsons Disease).
possible hazards in the Nurse will execute slowly using the RW and
environment ie. room clutter, passive and active to sit down slowly
bed position, if the overhead ROM exercises on making sure to grab arm
lights work, or if furniture is pts legs to avoid
rests on chairs before
blocking pts walking muscle fatigue and
lowering themself to add
pathway. cramping.
extra support and to
-Nurse will monitor avoid lightheadedness.
for orthostatic
hypotension while pt
is moving and
transferring.
References
Ackley, B. J., Ladwig, G. B., & Makic, M. B. (2017). Nursing diagnosis handbook: An evidence-based
guide to planning care (11th ed.). St. Louis, MO: Elsevier.
Lewis, S. L., Bucher, L., Heitkemper, M. M., & Harding, M. M. (2017). Medical-surgical nursing:
Assessment and management of clinical problems(10th ed.). St. Louis, MO: Elsevier, Inc.
You might also like
- PT102 - Tilt Table:IPC:Traction - NotesDocument4 pagesPT102 - Tilt Table:IPC:Traction - NotesDeo Sivan PacificoNo ratings yet
- This Study Resource Was: Nursing Diagnosis Intervention/Actions Outcomes/EvaluationDocument3 pagesThis Study Resource Was: Nursing Diagnosis Intervention/Actions Outcomes/EvaluationMagnala RosierNo ratings yet
- Nursing Care Plan for Constipation ReliefDocument3 pagesNursing Care Plan for Constipation ReliefWonie booNo ratings yet
- Careplan Weebly 2Document1 pageCareplan Weebly 2api-379909348No ratings yet
- Pair Treatment Plan 2Document8 pagesPair Treatment Plan 2api-403931768No ratings yet
- Bowel Incontinence ConstipationDocument3 pagesBowel Incontinence ConstipationMatty-b AskalaniNo ratings yet
- Submitted By: BSN 3Y2-9B: Nursing Care Plan (O.B.)Document5 pagesSubmitted By: BSN 3Y2-9B: Nursing Care Plan (O.B.)K-anne CherubicNo ratings yet
- Act2 - Additional Info and QuestionsDocument4 pagesAct2 - Additional Info and QuestionsMika SaldanaNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care Planapi-381428737No ratings yet
- Crutch WalkingDocument4 pagesCrutch WalkingJamby CastillonNo ratings yet
- Case IcuDocument5 pagesCase IcuTrisha SuazoNo ratings yet
- ABUEVA GULFAN NCP 1 Primary AldosteronismDocument2 pagesABUEVA GULFAN NCP 1 Primary AldosteronismAmy Rose AbuevaNo ratings yet
- Nursing Care Plan ConstipationDocument2 pagesNursing Care Plan ConstipationkazelleNo ratings yet
- Beginner - Intermediate: 4 Weeks To Total Hip MobilityDocument14 pagesBeginner - Intermediate: 4 Weeks To Total Hip Mobility714 BaliNo ratings yet
- Beginner - Intermediate: 4 Weeks To Total Hip MobilityDocument14 pagesBeginner - Intermediate: 4 Weeks To Total Hip MobilityHubert SelormeyNo ratings yet
- Pregnancy Walking WorkoutDocument2 pagesPregnancy Walking WorkoutnaturalchildbirthNo ratings yet
- Health AssessmentDocument13 pagesHealth AssessmentImee TolentinoNo ratings yet
- ASSESSMENT HEALTH NURSING INTERVENTION EVALUATIONDocument3 pagesASSESSMENT HEALTH NURSING INTERVENTION EVALUATIONtflorenzNo ratings yet
- NCP Ineffective Tissue PerfusionDocument2 pagesNCP Ineffective Tissue PerfusionYasminGianneDeOcampoBarizoNo ratings yet
- English 4Document14 pagesEnglish 4Dewi HastutiNo ratings yet
- Nursing Problem Explanation Goal Intervention Rationale Evaluation SubjectiveDocument1 pageNursing Problem Explanation Goal Intervention Rationale Evaluation SubjectiveZed P. EstalillaNo ratings yet
- Surgical Appendectomy Nursing CareDocument3 pagesSurgical Appendectomy Nursing CareRoel John Atamosa CasilacNo ratings yet
- Diarrhea: University of Santo Tomas-LegazpiDocument4 pagesDiarrhea: University of Santo Tomas-LegazpiJOSHUA DICHOSONo ratings yet
- Understanding Constipation and Establishing Normal Bowel FunctionDocument1 pageUnderstanding Constipation and Establishing Normal Bowel FunctionLoverMind CabaronNo ratings yet
- Nursing Process Septate UterusDocument6 pagesNursing Process Septate UterusJay PaulNo ratings yet
- Gann KDocument4 pagesGann Kapi-570554822No ratings yet
- 2 NCP Impaired Swallowing EditedDocument4 pages2 NCP Impaired Swallowing EditedLeonardo Montemayor100% (3)
- NCP Mugar Leptospirosis TLJPHDocument2 pagesNCP Mugar Leptospirosis TLJPHFRANZI ALYANNA MUGARNo ratings yet
- 2 NCP Impaired Swallowing EditedDocument4 pages2 NCP Impaired Swallowing EditedZharm MayNo ratings yet
- Worksheet CCJM Post OpDocument3 pagesWorksheet CCJM Post Opapi-631170779No ratings yet
- Nursing Care Plan for Patient with ConstipationDocument2 pagesNursing Care Plan for Patient with ConstipationAbby GonzalesNo ratings yet
- Nursing Care Plan Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentDocument2 pagesNursing Care Plan Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentEva Marielle CezaldoNo ratings yet
- ConstipationDocument4 pagesConstipationprincess_bee100% (1)
- Prioritization of Problems Rank Problem Identified: San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument5 pagesPrioritization of Problems Rank Problem Identified: San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesTom CuencaNo ratings yet
- NCM 107 Skills Lab NCPDocument1 pageNCM 107 Skills Lab NCPMoises Clerick BalloguingNo ratings yet
- Date/Time Focus Data, Action, and ResponseDocument2 pagesDate/Time Focus Data, Action, and ResponseHerbert BantilanNo ratings yet
- Palliative Care Management of ConstipationDocument5 pagesPalliative Care Management of ConstipationnehaNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care PlanCatherine Joy VillapandoNo ratings yet
- Hirschsprung Disease (Congenital Aganglionic Megacolon) : By: Romeo Benjamin D. Laurente Group 4 BSN-2ADocument11 pagesHirschsprung Disease (Congenital Aganglionic Megacolon) : By: Romeo Benjamin D. Laurente Group 4 BSN-2ARob Romeo Benjamin LaurenteNo ratings yet
- Providing Range of Motion ExercisesDocument5 pagesProviding Range of Motion ExercisesURS- Divine CabanizasNo ratings yet
- Top 3 NCP For CASE-PRES PDFDocument9 pagesTop 3 NCP For CASE-PRES PDFSmartieNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluatio NDocument2 pagesAssessment Diagnosis Planning Intervention Rationale Evaluatio NAngelou MortosNo ratings yet
- Risk For Constipation Nursing Care Plan Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective Data: Independent: Goal MetDocument10 pagesRisk For Constipation Nursing Care Plan Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective Data: Independent: Goal MetHydie Mae AlcabedosNo ratings yet
- Lumbar Strain: Dr. Lipy Bhat PT Faculty, Physiotherapy SrhuDocument38 pagesLumbar Strain: Dr. Lipy Bhat PT Faculty, Physiotherapy SrhuKapil LakhwaraNo ratings yet
- MalariaDocument3 pagesMalariasuciNo ratings yet
- Spinal Cord Injury: Causes, Symptoms, TreatmentDocument17 pagesSpinal Cord Injury: Causes, Symptoms, TreatmentPreciousmae Talay JavierNo ratings yet
- III. Nursing Care Plan: Assessment Diagnosis Goal Intervention EvaluationDocument4 pagesIII. Nursing Care Plan: Assessment Diagnosis Goal Intervention EvaluationSTEPHANIE JOSUENo ratings yet
- CT TractionDocument3 pagesCT TractionLaira CañeteNo ratings yet
- Spinal Bifida Ncp-Impaired Physical MobilityDocument3 pagesSpinal Bifida Ncp-Impaired Physical MobilityNicole cuencos0% (1)
- NHS UK Rotator Cuff RepairDocument5 pagesNHS UK Rotator Cuff RepairmertNo ratings yet
- Rotator Cuff RepairDocument5 pagesRotator Cuff RepairAdhitya TaslimNo ratings yet
- Strengthening Glutes and Core to Fix Computer Guy PostureDocument6 pagesStrengthening Glutes and Core to Fix Computer Guy PostureMinghua GuoNo ratings yet
- Pilates Stretch Class FormatDocument3 pagesPilates Stretch Class FormatDieu Thu NguyenNo ratings yet
- Pelvic Floor Exercises: A Guide For Men AboutDocument3 pagesPelvic Floor Exercises: A Guide For Men AboutemagooNo ratings yet
- Mock First Soap NoteDocument7 pagesMock First Soap Noteapi-372150835No ratings yet
- Nursing Care Plan StrokeDocument2 pagesNursing Care Plan StrokeA HNo ratings yet
- Dialysis-NCPDocument2 pagesDialysis-NCPJennifer AlamonNo ratings yet
- NURSING CARE PLAN FOR DIARRHEADocument2 pagesNURSING CARE PLAN FOR DIARRHEAKrizha Angela NicolasNo ratings yet
- BSN2 C Ihps NCP FinalDocument7 pagesBSN2 C Ihps NCP FinalAdrian DecolongonNo ratings yet
- If they could talk about walking again: Canine Cruciate Surgery Rehabilitation Program: A 10 week detailed program of specific approaches, exercises, massage, and restoring balance to get the best results after your pet has undergone surgery for cruciate ligament repair. Tracking sheets for each week.From EverandIf they could talk about walking again: Canine Cruciate Surgery Rehabilitation Program: A 10 week detailed program of specific approaches, exercises, massage, and restoring balance to get the best results after your pet has undergone surgery for cruciate ligament repair. Tracking sheets for each week.No ratings yet
- Research FinalDocument8 pagesResearch Finalapi-381116979No ratings yet
- Weebly ResumeDocument1 pageWeebly Resumeapi-379909348No ratings yet
- Langan Ethics Paper March19 2018Document6 pagesLangan Ethics Paper March19 2018api-379909348No ratings yet
- Careplan 3 WeeblyDocument1 pageCareplan 3 Weeblyapi-379909348No ratings yet
- Pediatric Endocrine Review - Part 5Document27 pagesPediatric Endocrine Review - Part 5Vicheth SenNo ratings yet
- African American Vegan Starter GuideDocument40 pagesAfrican American Vegan Starter GuideVegan Future89% (19)
- Co - Occurring Conditions FinalDocument25 pagesCo - Occurring Conditions FinalAshleyNo ratings yet
- Reh Prevod SpineDocument4 pagesReh Prevod SpineErmin HamidovicNo ratings yet
- Mansonella PerstansDocument8 pagesMansonella PerstansRobert BishopNo ratings yet
- ECT - Patient LeafletDocument4 pagesECT - Patient LeafletSarah GrixtiNo ratings yet
- Mental Illness and The MediaDocument4 pagesMental Illness and The Mediaprincess.carol8No ratings yet
- Introduction to Medical Terminology for Respiratory Care StudentsDocument58 pagesIntroduction to Medical Terminology for Respiratory Care StudentsChristina GonezNo ratings yet
- ANOLOGYDocument17 pagesANOLOGYManoj RaviNo ratings yet
- Psychological Criticism - DobieDocument24 pagesPsychological Criticism - DobieAngie AlalNo ratings yet
- Adult Combined ScheduleDocument13 pagesAdult Combined ScheduleJustin Ng SincoNo ratings yet
- Safe Back-To-School Program Minimum Safety Health Standard Plan For The SY 2020-2021 Frequently Asked QuestionsDocument3 pagesSafe Back-To-School Program Minimum Safety Health Standard Plan For The SY 2020-2021 Frequently Asked QuestionsSusan Loida SorianoNo ratings yet
- PAR-Q FormsDocument3 pagesPAR-Q FormsEric RyuNo ratings yet
- Seminars in Arthritis and RheumatismDocument9 pagesSeminars in Arthritis and RheumatismNoNo ratings yet
- Questões - Questoes de Vestibular3 PDFDocument6 pagesQuestões - Questoes de Vestibular3 PDFVictor Araujo PontesNo ratings yet
- NCM 106 Pharmacology Task Performace Written Assignment Format For FINALSDocument5 pagesNCM 106 Pharmacology Task Performace Written Assignment Format For FINALSNoemie DanaoNo ratings yet
- Emergency Drugs Used in O.S. Common Drug Interactions in O.S. Practice Oral SurgeryDocument52 pagesEmergency Drugs Used in O.S. Common Drug Interactions in O.S. Practice Oral SurgeryFourthMolar.comNo ratings yet
- Sensitivity To Wheat, Gluten and FODMAPs in IBS - Facts or Fiction - GutDocument19 pagesSensitivity To Wheat, Gluten and FODMAPs in IBS - Facts or Fiction - GutAlexandra NeeNo ratings yet
- Introduction to Epidemiology and Public HealthDocument22 pagesIntroduction to Epidemiology and Public HealthIbrar Faisal0% (1)
- The Femal Lower Genital Tract and CervixDocument70 pagesThe Femal Lower Genital Tract and CervixHussein MreydemNo ratings yet
- Breast FeedingDocument52 pagesBreast Feeding071263galina100% (1)
- Decoding Schizophrenia PDFDocument8 pagesDecoding Schizophrenia PDFAvengingBrain100% (2)
- TOP RANK REVIEW ACADEMY NURSING REVIEWDocument9 pagesTOP RANK REVIEW ACADEMY NURSING REVIEWRalph Pampola100% (2)
- Spinal StenosisDocument14 pagesSpinal StenosisHONGJYNo ratings yet
- A 21-Year-OldDocument2 pagesA 21-Year-OldNini Angelica SiringanNo ratings yet
- HTTP - Portable Gbadvance File Pokemon EmeraldDocument193 pagesHTTP - Portable Gbadvance File Pokemon EmeraldmeibookNo ratings yet
- Module in Chapter 3Document21 pagesModule in Chapter 3Laiza Mae Autor100% (1)
- Food AdulterationDocument82 pagesFood AdulterationSwarup DasNo ratings yet
- 11th Zoology EM Practical NotesDocument11 pages11th Zoology EM Practical NotesBhavana Gopinath100% (1)
- KWL Chart AssignmentDocument2 pagesKWL Chart AssignmentTyler Gray-BurrellNo ratings yet