Professional Documents
Culture Documents
(1990) ARAÚJO, Oscar E FLOWERS, Franklin P KING, Mark M. Griseofulvin: A New Look at An Old Drug
Uploaded by
Cassandra VérasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(1990) ARAÚJO, Oscar E FLOWERS, Franklin P KING, Mark M. Griseofulvin: A New Look at An Old Drug
Uploaded by
Cassandra VérasCopyright:
Available Formats
GRISEOFULVIN: A NEWLOOK AT ANOLD DRUG
Oscar E. Araujo, Franklin P. Flowers, and Mark M. King
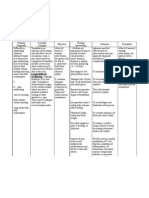
ABSTRACT: Griseofulvin is the oral antifungal agent of choice for the many non-fungal disease states have been published. It has
treatment of dermatophytoses, This article reviewsthe history, been noted by various researchers and clinicians to be use-
pharmacokinetics, adversereactions,and traditional therapeutic ful in the treatment of other disease states such as lichen
applications of griseofulvin. In addition, reports since 1960of the use
of the drug in the treatmentof Raynaud'sphenomenon, progressive planus, leprosy, scleroderma, and Raynaud's disease."
systemicsclerosis, lichenplanus, mycosisfungoides, herpes roster, These reports of effectiveness are often in the form of case
eosinophilic fasciitis, and molluscumcontagiosumare discussed, reports from the clinical setting rather than a result of con-
notingthe varyingdegreeof therapeutic success. trolled trials.
DlCP Ann Pharmacother 1990;24:851-4.
Meclumism ofAction
Even at high concentrations, griseofulvin is fungistatic
GRISEOFULVIN HASBEENONTHE MARKETfor several decades and not fungicidal. 4 It was first believed that the mecha-
having as its primary indicated use the treatment of der- nism of action of griseofulvin was the disruption of the syn-
matophyte infections. However, in the course of the last 20 thesis of chitin, a compound in fungal cell walls." The
years the drug has been reported to be useful in the therapy actual mechanism of action is still unknown, however, sev-
of a number of non-fungal disease states. The history ofthis eral theories have been proposed. One theory holds that the
versatile medication, its pharmacokinetic properties, and mechanism of action of griseofulvin lies in its ability to dis-
its application in conventional and non-conventional treat- rupt the mitotic spindle structure, thus arresting the fungal
ment regimens is reviewed. cell growth in the M-phase of its life cycle. Another pro-
posed mechanism suggests that griseofulvin may lead to
History the production of defective DNA, resulting in an inability
In 1939, Oxford et al. published a manuscript reporting of the fungal cells to replicate. 4,5
an interesting metabolic product of a strain of Penicillium The reason an oral dose of griseofulvin is effective against
received from Professor Biourge of the University of Lou- a fungal infection lying in the skin is that the drug tends to
vaine. The name proposed for this new compound was be deposited in keratin precursor cells. 5 Griseofulvin also
"griseofulvin," since the parent mold was termed Pen- shows a preference for infected cells instead of healthy
icilliumgriseofulvum.' Since its original discovery, grise- ones." In addition to its antifungal actions, griseofulvin
ofulvin has been derived from other organisms such as P. also displays certain antiinflammatory and minor vasodila-
janczewskii, P. patulum, and P. raistriki? tory effects. 5
For the next 20 years, little else was discovered about the
new compound until Gentles found that griseofulvin was
Pharmacokinetics
useful in the treatment of ringworm in guinea pigs.' Fol- ABSORPTION
lowing this revelation, a flurry of experiments was con- The absorption of griseofulvin following oral dosing is
ducted on the new compound to determine its effectiveness variable. The white, bitter compound is virtually insoluble
in the treatment of dermatophytoses, fungal infections that in water, diluted acid, or alkali. In vivo, the drug is mostly
until the advent of griseofulvin were very difficult to treat. absorbed from the duodenum, although it can also be ab-
The first experiments of the use of griseofulvin in humans sorbed from the jejunum and ileum. 4-6
were conducted in 1958 in Germany, Great Britain, and the The absorption of griseofulvin is enhanced by the reduc-
United States." tion of the particle size, thereby increasing the surface area
Since the 1960s, reports of the use of griseofulvin in of the compound." Currently, there are two formulations
of griseofulvin on the market utilizing different particle
OSCAR E. ARAUJO, Ph.D., is a Professor, DepartmentofPhannacy Practice,College sizes, and these ultramicrosize formulations are more rap-
of Phannacy; FRANKLIN P. FLOWERS, M.D., is an AssociateProfessorof Medi- idly, completely, and uniformly absorbed than the micro-
cine, Division of Dermatology, Departmentof Medicine, College of Medicine, Univer-
sity of florida, Gainesville, A..; and MARK M. KING, Phann.D., is a Community size formulations due to the polyethylene glycol added. 5.7
Pharmacist,Bartow,A... Reprints: Oscar E. Araujo,Ph.D., Box1-486,JHMHC, Gain- However, despite the claims of manufacturers that ultra-
esville, A.. 32610. microsize griseofulvin 250 mg is equivalent to 500 mg of
This article is approved for continuing education credit. the microsize preparations, there have been studies show-
ing that the plasma concentrations of the microsize forms
DICP, The Annals of Pharmacotherapy • 1990September, Volume 24 • 851
Downloaded from aop.sagepub.com at University of Otago Library on December 22, 2014
may be greater over a period of time than those obtained Therapeutic Indications
from the ultramicrosize griseofulvin. 4,7 The peak serum
DERMATOPHYTOSES
concentrations usually achieved following oral administra-
tion of 500 mg of microsize or 250 mg of ultramicrosize Since Gentles first reported the effectiveness of griseo-
griseofulvin are 0.4-2.0 IJ.g/mL and occur four to eight fulvin in eradicating ringworm infections, the drug has
hours after administration. 2-5 been used in the treatment of a number of fungal infections
Other means of increasing the absorption of griseofulvin of the hair and skin, especially tinea corporis, tinea pedis,
include the use of a high-fat diet, or preparation of an oil-in- tinea capitis, tinea barbae, tinea cruris, and tinea unguium. 2-5
water emulsion of the microsize drug. 4,7 Susceptible organisms include species of Trichophyton,
Microsporum, or Epidermophyton.r':" The response to
therapy with griseofulvin depends on the amount of kerati-
DISTRIBUTION
nization present in the infected skin surface along with the
Upon oral administration, griseofulvin becomes concen- time necessary for the natural desquamation process to
trated in the body's skin, hair, nails, liver, fat, and skeletal occur.5,10
muscles. 2-6 As mentioned earlier, the drug has a predis- Because of the site involved, treatment of fungal infec-
position for deposition into keratin precursor cells, leading tions of the toenails requires many months.v'? Hay et al.
to an unfavorable environment for fungal growth. Since the demonstrated positive results in the treatment of onychomy-
drug also displays an affinity for diseased skin, it is be- coses caused by Trychophyton rubrum by using a topical
lieved that griseofulvin disrupts the fungal cells already solution of 28% tioconazole applied twice daily, as adjunc-
present by the disruption of the cell's mitotic spindle struc- tive therapy to oral griseofulvin 500 mg bid. They reported
ture. 3,5 that when the combination of drugs was used as therapy, the
Griseofulvin appears in the skin approximately four hours chance of complete remission and more rapid improvement
after an oral dose at a concentration of 1 IJ.g/g of skin. Eight was greater than when griseofulvin was used with a base
hours after administration, it is present at a concentration of placebo. However, they also noted that despite this combina-
approximately 3 IJ.g/g. 5 tion treatment, 30 percent of the patients being treated with
An interesting property of griseofulvin is that more of the griseofulvin failed to gain complete remission even after a
drug can be found in the outer layers of the skin than one year of therapy. In all cases the patients were followed for one
would suspect from an orally administered preparation. year. Statistically significant differences (p<0.005) were
The reason for this property is believed to be that some of detected, where 69 percent of nails achieved clinical remis-
the drug is transported to the outer layers via the sweat sion when treated with griseofulvin plus tioconazole com-
glands.v" pared with 41 percent receiving oral drug plus base only."
In another study, Tanz et al. compared the effectiveness of
ELIMINATION ketoconazole 3.3-6.6 mg/kg/d versus griseofulvin 10-20
The elimination half-life of griseofulvin is variable (9- mg/kg/d for a 12-week treatment of tinea capitis caused by T.
24 hours) even within the same patient. 3,6 After an oral tonsurans. Using a randomized, double-blind study design,
dose, 50 percent of the compound is excreted in the urine they attempted to ascertain if there was a significant dif-
and 36 percent in the feces within five days.4,6 The major ference in the remission rates of 48 patients with tinea capitis.
metabolites of griseofulvin are 6-desmethyl-griseofulvin Of the 22 patients receiving ketoconazole, 16 (73 percent)
and its glucuronide conjugate. 6 were considered successfully treated, and 25 of 26 patients
(96 percent) receiving griseofulvin were cured. The re-
Adverse Reactions searchers concluded that while the results of their study
showed differences that were not statistically significant,
The most common adverse effects that occur during gri- (p<0.10) griseofulvin should remain the drug of choice."
seofulvin therapy are headaches, nausea, vomiting, anorex-
ia, abdominal cramps, flatulence, and diarrhea. Usually,
RAYNAUD~PHENOMENON
the headache is transient and resolves upon continued use
of the drug. 4,5 By taking the medicine with meals, one not In 1973, Sabri et al. conducted a double-blind, crossover
only increases the absorption of griseofulvin, but also de- clinical trial to determine the effects of griseofulvin treat-
creases the gastrointestinal discomforts associated with the ment in patients with Raynaud's phenomenon. Twenty-four
compound." patients were assigned to one of two groups, based on the
One of the more disturbing adverse effects of the drug is severity of pain associated with their disease state. Four-
the photosensitivity reaction it can induce, which may even teen patients assigned to Group A had the most severe pain
lead to a precipitation or exacerbation of lupus erythemato- and randomly received either two 500-mg tablets bid of gri-
SUS. 4 ,5,8 seofulvin (British Pharmacopeia) or a placebo. For the ten
Hypersensitivity reactions to griseofulvin include urti- patients in Group B, 500 mg of the same formulation of gri-
caria, erythema multiforme, and serum sickness." A case seofulvin or the placebo was given in the morning and
of fatal toxic epidermal necrolysis following the use of gri- again at night. Each patient was on hislher initially assigned
seofulvin has been reported, and is only the second docu- therapy for four weeks, followed by a one-week wash-out
mented case recorded in the literature." Since griseofulvin period. At the conclusion of the wash-out period, the
is derived from species of Penicillium, there is a remote patients were assigned to their alternative four-week treat-
chance of a cross-sensitivity reaction with penicillin. ment regimen (either drug or placebo). 13
Central nervous system reactions include dizziness, fa- Different treatment regimens were evaluated as a prefer-
tigue, and insomnia. On rare occasions, elevations ofpor- ence by the patient as to clinical success at the end of the
phyrin have been reported with griseofulvin therapy.5 study. Ten of the patients in Group A preferred the treat-
852 • DICP, The Annals of Pharmacotherapy • 1990 September, Volume 24
Downloaded from aop.sagepub.com at University of Otago Library on December 22, 2014
Griseofulvin
ments with griseofulvin and four expressed no preference. seven-patient study and no improvement of the disease in
In Group B, five of the ten patients expressed a preference the r~maining two patients. The patients were given griseo-
for the griseofulvin treatment, three patients for the place- fulvin 500 mg for 2Yz months. It is conceivable that the
bo, and two expressed no preference. Physician assessment negative clinical results were related to the fact that therapy
showed no significant differences between griseofulvin and was carried out for only ten weeks."
pl~cebo. The authors suggest that griseofulvin may help
relieve the symptoms of Raynaud's phenomenon by in-
MYCOS~ FUNGOIDES
creasing the blood flow in small arteries and that the effect
appears to be dose-related. 13 Griseofulvin also has been shown to have a possible role
in the treatment of mycosis fungoides. Shelley reported on
PROGRESSrvESYSTEMUCSCLEROS~ a patient with well-delineated, bilateral, erythematous,
The effectiveness of griseofulvin in the treatment of pro- scaling atrophic plaques in the axillae and bathing suit area.
gressive systemic sclerosis (PSS) has been observed. Ferri The patient was diagnosed as having mycosis fungoides
et al. treated 33 patients with a fine-particle griseofulvin and treated with nitrogen mustard for a period of ten days.
preparation in doses of 375-500 rng/d for 18-84 (mean 33) A papulosquamous area developed in the patient's groin
months. Patients were followed at 12-month intervals and and the nitrogen mustard was discontinued. The new le-
evaluated at the end of the treatment. Both the observers sions were diagnosed as tinea cruris, and griseofulvin ther-
and the patients noted a definite improvement in the con- apy was initiated at a dose of 500 mg bid."
dition of the skin. Increased skin elasticity, hair growth, After a month of treatment, the plaques of mycosis
and better joint mobility were observed in 85 percent of the fungo ides had resolved and griseofulvin dosing was con-
patients. As noted by the authors, this study was open- tinued for three years. When the drug was discontinued, the
ended and did not allow a definite assessment of griseoful- plaques reappeared. Griseofulvin therapy was reinstituted,
vin's true effectiveness in the treatment ofPSS. 14 However, and the plaques again subsided after one month. It was sug-
the drug seems to counteract skin thickening and improve gested that the griseofulvin may inhibit chronic infections
skin elasticity as indicated by chest expansion. No mecha- leading to antigen release, which may be responsible for the
nism of action was proposed. plaques of mycosis fungoides." Similar results were re-
ported a few months later by Thomsen." Although the
LICHEN PLANUS
data for this novel treatment is sparse it should be kept in
mind for patients recalcitrant to traditional treatment.
An accidental observation led to the use of griseofulvin
in the treatment of lichen planus when a patient being HERPES roSTER
treated for a concomitant tinea corporis infection showed
clinical improvement of his lichen planus. These observa- Griseofulvin has also been used for herpes zoster. Jou-
tions led Sehgal et al. to conduct a double-blind study of 44 bert treated four patients experiencing severe pain from the
patients who received a treatment regimen of either griseo- disease. After treatment with griseofulvin, dramatic im-
fulvin fine particles 500 mg or placebo for an eight-week provement was observed in all patients. 20 Castelli et al. con-
period. At the end of the trial, patients were assessed clini- ducted a placebo-controlled trial of 57 patients with con-
cally and histologically for improvement. 15 firm.ed herpes zoster. They were randomly assigned to
Complete clinical improvement, defined as a decrease in receive one of four treatments: methisoprinol (inosine pran-
pruritus, a decrease in scaling, and a flattening of lesions obex) I g qid, griseofulvin 125 mg qid, griseofulvin and
followed by postinflammatory pigmentation, was observed methisoprinol concomitantly at the above doses, or a placebo
in 81.8 percent of the patients receiving griseofulvin versus qid. Griseofulvin alone afforded no improvement of the con-
none in the placebo group. A partial clinical improvement dition and the methisoprinol-griseofulvin combination
was noted in 18.2 percent of the drug-treatment group as provided significantly more pain relief than either treatment
opposed to 22.7 percent partial improvement in the placebo alone." The mechanism for this potentiation is not clear,
group. Histological improvement was noted only in the gri- but the effect of griseofulvin on the immune system may
seofulvin patients, where the histopathology of lichen planus interact positively with the immunomodulating action of
could no longer be observed. The authors theorized that the methisoprinol.
drug may have interfered with nucleic acid metabolism vital
to the keratinization process to produce these dramatic re- EOSINOPHILIC FASCDTIS
sults." Giordano et al. reported the case of a 25-year-old man suf-
Levy et al. have published a study of 26 patients with fering from eosinophilic fasciitis who was treated with grise-
lichen planus who were treated with two griseofulvin fine ofulvin for eight months. Significant clinical improvement
particle 125-mg tablets bid for three weeks to six months. occurred, where previous treatment with corticosteroids and
At two-week intervals, the patients were assessed for sub- azathioprine had failed. Eosinophils, gammaglobulins, and
jective (decreased pruritus) and objective (appearance of the erythrocyte sedimentation rate decreased after only one
lesions) improvement. After the treatment period, the hour of treatment. The authors suggested that griseofulvin
patients were followed for an additional six months to two may prove to be an effective alternative to corticosteroid
years. An overall resolution of the lesions was noted in therapy in eosinophilic fasciitis.P
80-90 percent of all patients with initial improvement
observed in two weeks."
Not all of the reports using griseofulvin for the treatment MOLLUSCUM CONTAGIOSUM
of lichen planus are positive. Bagan et al. observed a wors- Treatment of molluscum contagiosum with griseofulvin
ening of the lesions of lichen planus in five patients in a was reported by Singh and Kanwar in a study of five pa-
DICP. The Annals of Pharmacotherapy • 1990 September, Volume 24 • 853
Downloaded from aop.sagepub.com at University of Otago Library on December 22, 2014
tients who had extensive viral infections. The patients were 14. FERRI C, BERNINI L, BOMBARDlERI S, PASERO G. Long-term griseoful-
given griseofulvin 500 mg/d for four to six weeks. Each vin treatment for progressive systemic sclerosis. Scand J Rheumatol
patient saw a complete disappearance of the lesions within 1986;15:356-62.
15. SEHGAL VN, BIKHCHANDANI R, KORANNE RV, NAYAR M, SAXENA
this time. The researchers reported complete resolution of HMK. Histopathological evaluation of griseofulvin therapy in lichen
the lesions, and no recurrences of their condition were planus, a double-blind controlled study. Dermatologica 1980;161:
noted in eight months of follow-up. 23 22-7.
16. LEVY A, STEMPLER D. YUZUK S. SCHEWACH-MILLET M, RONEN M.
Summary Communication: treatment of lichen planus with griseofulvin (letter).
Int J DermatoI1986;25:405.
Since its discovery 50 years ago, griseofulvin has been 17. BAGAN N. SILVESTRE FJ, MESTRE S, GISBERT C, BERMEJO A, AGRA-
used in the treatment of various skin conditions. Although MUNT1. Treatmentof lichen planus with griseofulvin; report of seven
many nonfungal diseases have shown some response to gri- cases. Oral SurgMed OralPathoI1985;60:608-10.
18. SHELLEY WB. Demethylchlortetracycline and griseofulvin as examples
seofulvin therapy, the major impact of the compound still of specific treatment for mycosis fungoides. Br J Dermatol 1981;
lies in its ability to effectively treat susceptible species of 104:477-80.
dermatophytes (tineas). It must also be stated that most of 19. THOMSEN K. Correspondence: mycosis fungoides responding to
the studies have limited data to support the use of griseoful- tetracyclineand griseofulvin (letter). Br J DermatoI1981;105:483-4.
vin routinely to treat these nonfungal diseases. Nonethe- 20. JOUBERT JD. Correspondence: griseofulvin in the treatment of herpes
less, the drug should be kept in mind as a potential treatment zoster (letter). S Afr Med J 1978;54(6):224.
21. CASTELLI M, ZANCA A. GIUBERTONI G, ZANCA A, BERTOLINI A.
alternative for the several conditions discussed.s> Griseofulvin-methisoprinol combination in the treatment of herpes
zoster. PharmacolRes Commun 1986;18:991-6.
References 22. GIORDANO M. ARA M, CICALA C, VALENTINI G. CHIANESE U. Corre-
I. OXFORD AE, RAlSTRICK H, SIMONART P. Griseofulvin, C. 7H I70.CI, a spondence: griseofulvin for eosinophilic fasciitis (letter). Arth Rheu-
metabolic product of Pennicillium Griseo-fulvum Dierckx. Biochem J matoI1980;23:1331-2.
1939;33:240-8. 23. SINGH 01' KANWAR AJ. Griseofulvintherapyin molluscumcontagiosum
2. ANDERSON DW. Griseofulvin: biology and clinical usefulness. Ann (letter). Arch DermatoI1977;113: 1615.
Allergy 1965;23:103-10.
3. GENTLES Jc. Experimental ringworm in guinea pigs: oral treatment with
griseofulvin. Nature 1958;182:476-7.
4. BECKER LE.Griseofulvin. DermatolClin 1984;2:115-20. EXTRACTO
5. MCEVOY GK, ed. Drug information 88. Bethesda, MD: American La griseofulvina sigue siendo el agente antift1ngico oral de elecci6n
Society of Hospital Pharmacists, 1988:76-8. para eI tratamiento de dermat6fitosis. Este articulo revisa la
6. UN C-C,MAGAT J, CHANG R, MCGLOTTEN J, SYMCHOWICZ S. Absorp- historia, farmacocinetica, reacciones adversas, y aplicaciones
tion, metabolism and excretion of 14C-griseofulvin in man. J Phar- terapeuticas tradicionales de la griseofulvina asf como su empleo
macol Exp Ther 1973;187:415-22. con resultados variables en el tratamiento del fen6meno de
7. STRAUGHN AB,MEYER MC,RAGHOW G, ROTENBERG K. Bioavailabil- Raynaud, esclerosis sistemica progresiva, liquen plano, micosis
ity of microsize and ultramicrosize griseofulvin products in man. J fungoides, herpes zoster, fascitis eosinofflica, y molluscum
Pharmacokinet Biopharm 1980;8:347-62. contagiosum.
8. BLANK H. Commentary: treatment of dermatomycoses with griseoful- CARMEN CAO
vin. Arch DermatoI1982;118:834-6.
9. MION G. VERDON R, LEGULLUCHE Y. CARSIN H. GARCIE A,
GUlLBAUD 1. Fataltoxicepidermalnecrolysisafter griseofulvin(letter).
Lancet 1989;2:1331. RESUME
10. HAY RJ,CLAYTON YM, GRIFFITHS WAD, OOWD PM.A comparativedou-
ble blind study of ketoconazole and griseofulvin in dermatophytosis. La griseofulvine est toujours un agent antifongique de choix pour Ie
BrJ DermatoI1985;112:691-6. traitement des dermatophytoses. Cet article revise l'historique, la
II. HAY RJ, CLAYTON YM, MOORE MK. A comparison of tioconazole 28% pharmacocinetique, les reactions adverses et les applications
nail solution versus base as an adjunct to oral griseofulvin in patients therapeutiques traditionnelles de la griseofulvine. De plus on y
with onychomycosis. Clin Exp DermatoI1987;12: 175-7. discute des rapports existants depuis 1960 sur son utilisation dans Ie
12. 1J\NZ RR,HEBERT AA.ESTERLY NB.Treatingtinea capitis: should keto- traitement du phenomene de Raynaud, de la sclerose systemique
conazole replace griseofulvin? J Pediatr1988;1/2:987-91. progressive, du lichen plan, de la mucosite fongoide, de l'herpes
13. SABRI S, ROBERTS VC, HIGGINS RF, COTTON LT, WILLIAMS Dl, WIL- zoster, de la fascitite eosinophilique et du molluscum contagiosum
SON Le. A double-blind clinical trial of griseofulvin in patients with en y denotant Ie degre variable de succes therapeutique.
Raynaud's phenomenon. PostgradMed J 1973;49:641-3. CHANTAL GUEVREMONT
854 • DICP, The Annals of Pharmacotherapy • 1990 September, Volume 24
Downloaded from aop.sagepub.com at University of Otago Library on December 22, 2014
You might also like
- (2016) MCEVENUE, Giancarlo KIM, Ashley BINHAMMER, Paul. Surgical Excision of Mycosis Fungoides Using Thumb-Sparing ReconstructionDocument5 pages(2016) MCEVENUE, Giancarlo KIM, Ashley BINHAMMER, Paul. Surgical Excision of Mycosis Fungoides Using Thumb-Sparing ReconstructionCassandra VérasNo ratings yet
- (2017) ESAU, Daniel. Viral Causes of Lymphoma - The History of Epstein-Barr - Virus and Human T-Lymphotropic VirusDocument6 pages(2017) ESAU, Daniel. Viral Causes of Lymphoma - The History of Epstein-Barr - Virus and Human T-Lymphotropic VirusCassandra VérasNo ratings yet
- Tazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaDocument5 pagesTazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaCassandra VérasNo ratings yet
- Bmi s16553Document8 pagesBmi s16553Cassandra VérasNo ratings yet
- Tazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaDocument5 pagesTazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaCassandra VérasNo ratings yet
- (2016) HASBACH, Andrea E., STERN, Adam W. Pagetoid Reticulosis (Epitheliotropic Cutaneous T-Cell Lymphoma) in An Adult Alpaca (Vicugna Pacos)Document4 pages(2016) HASBACH, Andrea E., STERN, Adam W. Pagetoid Reticulosis (Epitheliotropic Cutaneous T-Cell Lymphoma) in An Adult Alpaca (Vicugna Pacos)Cassandra VérasNo ratings yet
- (2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Document5 pages(2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Cassandra VérasNo ratings yet
- (2016) HASBACH, Andrea E., STERN, Adam W. Pagetoid Reticulosis (Epitheliotropic Cutaneous T-Cell Lymphoma) in An Adult Alpaca (Vicugna Pacos)Document4 pages(2016) HASBACH, Andrea E., STERN, Adam W. Pagetoid Reticulosis (Epitheliotropic Cutaneous T-Cell Lymphoma) in An Adult Alpaca (Vicugna Pacos)Cassandra VérasNo ratings yet
- A CD30 ( ) Transformed Mycosis Fungoides Case Responding Very Well To Systemic Bexarotene and MethotrexateDocument3 pagesA CD30 ( ) Transformed Mycosis Fungoides Case Responding Very Well To Systemic Bexarotene and MethotrexateCassandra VérasNo ratings yet
- (2016) MORIN, Catherine Besner Et Al. Tazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaDocument100 pages(2016) MORIN, Catherine Besner Et Al. Tazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaCassandra VérasNo ratings yet
- (2016) TSAI, Jeng-Dau Et Al. Risk of Stroke in Patientes With Mycosis Fungoides: A Nationwide Population-Based Cohort StudyDocument2 pages(2016) TSAI, Jeng-Dau Et Al. Risk of Stroke in Patientes With Mycosis Fungoides: A Nationwide Population-Based Cohort StudyCassandra VérasNo ratings yet
- (2017) ESAU, Daniel. Viral Causes of Lymphoma - The History of Epstein-Barr - Virus and Human T-Lymphotropic VirusDocument6 pages(2017) ESAU, Daniel. Viral Causes of Lymphoma - The History of Epstein-Barr - Virus and Human T-Lymphotropic VirusCassandra VérasNo ratings yet
- (2015) TAWDY, Amira El Et Al. Assessment of Tissue Level of Histone Deactylase-2 (HDAC-2) in Patients With Mycosis FungoidesDocument4 pages(2015) TAWDY, Amira El Et Al. Assessment of Tissue Level of Histone Deactylase-2 (HDAC-2) in Patients With Mycosis FungoidesCassandra VérasNo ratings yet
- (2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaDocument12 pages(2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaCassandra VérasNo ratings yet
- Tazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaDocument5 pagesTazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaCassandra VérasNo ratings yet
- (2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Document4 pages(2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Cassandra VérasNo ratings yet
- (2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Document5 pages(2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Cassandra VérasNo ratings yet
- Tazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaDocument5 pagesTazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaCassandra VérasNo ratings yet
- (2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaDocument12 pages(2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaCassandra VérasNo ratings yet
- Tazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaDocument5 pagesTazarotene 0.1% Cream As Monotherapy For Early-Stage Cutaneous T-Cell LymphomaCassandra VérasNo ratings yet
- (2015) TAWDY, Amira El Et Al. Assessment of Tissue Level of Histone Deactylase-2 (HDAC-2) in Patients With Mycosis FungoidesDocument4 pages(2015) TAWDY, Amira El Et Al. Assessment of Tissue Level of Histone Deactylase-2 (HDAC-2) in Patients With Mycosis FungoidesCassandra VérasNo ratings yet
- (2016) HASBACH, Andrea E., STERN, Adam W. Pagetoid Reticulosis (Epitheliotropic Cutaneous T-Cell Lymphoma) in An Adult Alpaca (Vicugna Pacos)Document4 pages(2016) HASBACH, Andrea E., STERN, Adam W. Pagetoid Reticulosis (Epitheliotropic Cutaneous T-Cell Lymphoma) in An Adult Alpaca (Vicugna Pacos)Cassandra VérasNo ratings yet
- (2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Document5 pages(2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Cassandra VérasNo ratings yet
- (2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Document4 pages(2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Cassandra VérasNo ratings yet
- (2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaDocument12 pages(2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaCassandra VérasNo ratings yet
- (2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Document5 pages(2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Cassandra VérasNo ratings yet
- (2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaDocument12 pages(2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaCassandra VérasNo ratings yet
- (2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Document4 pages(2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Cassandra VérasNo ratings yet
- (2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Document5 pages(2017) GHAZAWI, Feras M. Et Al. Distribution and Clustering of Cutaneous (CTCL) - Cases in Canada During 1992 To 2010Cassandra VérasNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Milk Microbiology: Viable Count Method Dye Reduction Test Direct Microscopic CountDocument14 pagesMilk Microbiology: Viable Count Method Dye Reduction Test Direct Microscopic CountDayledaniel SorvetoNo ratings yet
- 171-199 Embryologic and Anatomic Basis of Duodenal Surgery PDFDocument29 pages171-199 Embryologic and Anatomic Basis of Duodenal Surgery PDFРоман МошнягаNo ratings yet
- Life Processes Class 10 Notes BiologyDocument8 pagesLife Processes Class 10 Notes BiologyEashurock KnigamNo ratings yet
- Breathing Exercise StepDocument45 pagesBreathing Exercise StepFebri Ayu MentariNo ratings yet
- 24 - Pharyngeal Arches and Its DerivativesDocument32 pages24 - Pharyngeal Arches and Its DerivativesDr.B.B.GosaiNo ratings yet
- Triage Lecture DR F Mesa GaerlanDocument55 pagesTriage Lecture DR F Mesa Gaerlanapi-19431894100% (1)
- Animal Farm Chapter 7 Summary: Windmill Destroyed, Hens Rebel Against OrdersDocument3 pagesAnimal Farm Chapter 7 Summary: Windmill Destroyed, Hens Rebel Against OrdersLianne ChuaNo ratings yet
- Difficulty in SwallowingDocument1 pageDifficulty in SwallowingmawelNo ratings yet
- Feline Behaviour and Welfare PDFDocument211 pagesFeline Behaviour and Welfare PDFNourhan ELmarawanyNo ratings yet
- Evidence Sports and Animals ResueltoDocument2 pagesEvidence Sports and Animals ResueltoJuank PrzNo ratings yet
- Accelerated Orthodontics A ReviewDocument9 pagesAccelerated Orthodontics A ReviewvijayprabugNo ratings yet
- Applications OF ANIMAL BEHAVIOURDocument7 pagesApplications OF ANIMAL BEHAVIOURUsama ElahiNo ratings yet
- Prevalensi AtopiDocument33 pagesPrevalensi AtopiAnova FatimahNo ratings yet
- SexpediaDocument43 pagesSexpediaYouth organization "Lentvari park renaissance"No ratings yet
- Functions of Blood and ComponentsDocument15 pagesFunctions of Blood and ComponentsayuNo ratings yet
- Orbital Bone Anatomy and Orbital FracturesDocument9 pagesOrbital Bone Anatomy and Orbital Fracturesm29hereNo ratings yet
- Ban 'Unhealthy' Dog Breeds, Say VetsDocument2 pagesBan 'Unhealthy' Dog Breeds, Say VetsNicholay AtanassovNo ratings yet
- 2014 Price List Medical Training ManikinsDocument45 pages2014 Price List Medical Training ManikinsNovie NursantyNo ratings yet
- AIDocument45 pagesAImit_thakkar_2No ratings yet
- Grammar Meets ConversationDocument3 pagesGrammar Meets ConversationnilofanilofaNo ratings yet
- StrongyloidiasisDocument24 pagesStrongyloidiasisIzhra Margate0% (1)
- Lung AnatomyDocument16 pagesLung AnatomywhyseejoshNo ratings yet
- Dr. Esperanza Cabral ModuleDocument54 pagesDr. Esperanza Cabral ModuleNazarine TorresNo ratings yet
- NCP-Fluid Volume DeficitDocument2 pagesNCP-Fluid Volume Deficitanon_207994234100% (1)
- Class 12 Physical EducationDocument31 pagesClass 12 Physical EducationSohan KarmakarNo ratings yet
- BloodDocument5 pagesBloodKyla CarbonelNo ratings yet
- 2.1. Cells Tissues Organs PDFDocument41 pages2.1. Cells Tissues Organs PDFRobert YabutNo ratings yet
- Chapter 8 NotesDocument4 pagesChapter 8 Notesbrady.anderson3017No ratings yet
- PriapismDocument7 pagesPriapismHilma Rizka HermayeniNo ratings yet
- Materi Digestive SystemDocument13 pagesMateri Digestive Systembetta putriNo ratings yet