Professional Documents
Culture Documents
Handbook of Sexual Dysfunction
Uploaded by
Renato SánchezCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Handbook of Sexual Dysfunction
Uploaded by
Renato SánchezCopyright:
Available Formats
• A leading cause of life-threatening perinatal infections in United States.
• 15–30% of women are asymptomatic carriers.
• Infection rate has decreased from 1.8/1000 in 1990 to 0.34/1000 live births in 2004.
• Early onset infection (80% within 6 hours of delivery)—4% neonatal mortality of term infants INFECTIOUS DISEASES Mastitis and Breast Abscess
and 23% mortality in preterm infants.
Table 7.1. Procedures
INFECTIOUS DISEASESfor collecting clinical specimens for culture of group B Streptococcus
Group B Streptococcus(GBS)
Drug Regimens
at 35–37 weeks’ gestation Table 7.5. Drug regimens for the treatment of mastitis
• Swab the lower vagina (vaginal introitus), followed by the rectum (i.e., insert swab through the anal sphincter) using Cephalexin (Keflex) 500 mg orally every 6 hr for 7 days
Table 7.2. Comparison of key points in the 2002 and 2010 centers for disease control and
the same swab or two different swabs. Cultures should be collected in the outpatient setting by the health care Amoxicillin/Clavulante potassium (Augmentin) 875 mg orally every 12 hr for 7 days
prevention
provider or,guidelines for theinstruction,
with appropriate prevention of patient
by the perinatal group
herself. B streptococcal
Cervical, diseaseor perineal specimens
perianal, perirectal, Azithromycin (Zithromax) 500 mg initially, then 250 mg orally daily for 5–7 days
are not acceptable, and a speculum should not be used for culture collection.
Topic in the Guidelines Key Points Unchanged from 2002 Key Points Changed from 2002 Dicloxacillin 250–500 mg orally every 8 hr for 7 days
• Place the swab(s) into a nonnutritive transport medium. Appropriate transport systems (e.g., Stuart’s or Amies with or
Clindamycin 300 mg orally every 8 hr for 7 days
Universal
withoutscreening
charcoal)forare commercially
Universal screening at 35–37
available. weeks of
GBS isolates Permissive
can remain viable statement for media
in transport limited role of
for several days at
GBS roomacidtemperature;
amplificationhowever,
gestation remains the
the recovery sole strategy
of isolates for IAP.
declines nucleic
over one to four days, especially at elevated tempera- Source: Reproduced with permission from Hager, W. David. Managing mastitis. Cont Ob/Gyn. 2004:Jan;33-47.
teststures,
for intrapartum
which can lead to false-negative results. When feasible, specimens should be refrigerated before processing. Cont Ob/Gyn is a copyrighted publication of Advanstar Communications Inc. All rights reserved.
GroupforBGBS
testing Streptococcus INFECTIOUS DISEASES
• Specimen requisitions should indicate clearly that specimens are for group B streptococcal testing. Patients who state
Preterm delivery New and separate algorithms for preterm
that they are allergic to penicillin should be evaluated for risk for anaphylaxis. If a woman is determined to be at high Prevention
labor and for PPROM (see Fig. 7.1 and
risk for anaphylaxis,* susceptibility testing for clindamycin and erythromycin
Fig. 7.2)
should be ordered. • Avoid cracked or fissured nipples.
Patient allergic to penicillin?
GBS*Patients
specimen collection
with a history ofRectovaginal swab specimens
any of the following collected penicillin
after receiving Transport options clarifiedare considered to be at
or a cephalosporin • Use plain water to clean nipple area (No. soap or alcohol).
and
highprocessing at 35–37
No weeks
risk for anaphylaxis: anaphylaxis, of gestation
angioedema, remains the
respiratory distress, or urticaria.
Identification Yes expanded to include
options • Increase duration of nursing gradually to avoid soreness.
recommendation. use of chromogenic media and nucleic acid
Source: Reproduced from Verani JR, McGee L, Schrag SJ; Division of Bacterial Diseases, National Center for Immu- • Use breast shield or topical cream to help healing of cracked nipples.
amplification
nization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC). testsPrevention of perinatal group B • Place finger in corner of baby’s mouth during feeding to break sucking force.
streptococcal Penicillin
disease— G,revised guidelines
5 million fromdose,
units IV initial CDC, 2010. MMWR Recomm
a historyRep.
Laboratories
Patient with 2010
oftoany
report Nov
GBS
of the 19;59(RR-
in 10):1-36.
concentrations
following • Treat recurrent mastitis promptly but continue breastfeeding.
then 2.5–3.0 million units† every 4 hr until delivery of greater
after receiving thanororaequal
penicillin to 104 CFU
cephalosporin? § in urine INFECTIOUS DISEASES 2015 CDC STI Treatment Guidelines
or culture specimens (previously, it was GBS “in
Anaphylaxis Patient Information: What to Do If You Develop Mastitis?
any concentration”)
Ampicillin, 2 g IV initial dose, Angioedema Table 7.6. Patient information: what to do if you develop mastitis
Intrapartum antibiotic Penicillin
4 hrremains drug of choice with RespiratoryDefinition
distressof high risk for anaphylaxis is
prophylaxis
then 1 g IV every until delivery
ampicillin as an alternative. Cefazolin Urticariaclarified
Bacterial Vaginosis
If you have symptoms that suggest you have mastitis, you’ll need to heed the following advice:
remains the drug of choice for penicillin Minor change in penicillin dose permitted Table 7.36. 2015 CDC guidelines for treatment of bacterial vaginosis
allergy without anaphylaxis, angioedema, • Continue
Treatment is breastfeeding,
recommended starting on the affected
for all symptomatic side. women.
pregnant
No
respiratory distress, or urticaria. Erythromycin
Yes is no longer recommended
under any circumstances • If your baby doesn’t feed well or will not feed on the affected breast, empty the breast using a piston-type, hospital
387
GBS isolates from women at high risk of
D- test recommended to detect inducible 7 Recommended
breast pump.Regimens
anaphylaxis should be tested for uscep- • If possible, remain in bed
tibility to 2clindamycin and erythromycin. resistance in isolates tested for susceptibility
¶
Metronidazole 500 mg orallyfortwice
the first
a day48 for
hr. 7 days
Cefazolin, g IV initial dose, Isolate susceptible
to to clindamycin
clindamycin and erythromycin • Drink more fluids.
then 1Vancomycin
g IV every 8use is recommended
hr until delivery if and erythromycin**? Metronidazole gel 0.75%, one full applicator (5 g) intravaginally, once a day for 5 days
isolate is resistant to either clindamycin or • Reduce your
Clindamycin salt intake.
cream 2%, one full applicator (5 g) intravaginally at bedtime for 7 days
erythromycin. • Take acetaminophen or ibuprofen to reduce fever and discomfort so milk letdown will occur and the breast can be emptied.
Other obstetric No Data are not sufficient
Yes to make recommen- Alternative Regimens:
• Apply moist heat to speed up milk letdown and ease soreness; cool packs may be used initially to decrease swelling.
management issues dations regarding the timing of procedures Tinidazole 2 g orally oncetodaily
intended to facilitate progression of labor, • Apply gentle massage moveforthe
2 milk
daysforward and increase drainage from the infected area.
such as amniotomy, in GBS-colonized Tinidazole 1 g orally
• Avoid breast shells once dailyfitting
and tight- for 5bras.
days
Vancomycin, 1 g IV women.Clindamycin, 900 mg IV Clindamycin
• Avoid tight300 mg orally
clothing twice daily
and underwire for 7 days
bras.
every 12 hr until delivery everyantibiotic
8 hr until prophylaxis
delivery Clindamycin bedtime for 3 days*
Intrapartum is optimal • Wash yourovules
hands100 mghandling
before intravaginally once atbreast.
the infected
if administered at least 4 hours before
• Lanolin creamsovules
*Clindamycin may beuseused to treat nipples.
an oleaginous base Your physician
that might may latex
weaken prescribe medication
or rubber if you
products develop
(e.g., a fungal
condoms and vaginal
delivery; therefore, such procedures should
dd 387 Figure 7.4. Recommended regimens for intrapartum antibiotic prophylaxis forif possible.
prevention of infection
12/1/16 8:26ofAM
contraceptive the nipple. Use of such products within 72 hours following treatment with clindamycin ovules is not
diaphragms).
be timed accordingly,
recommended.
• Make sure your baby is in a comfortable nursing position that does not pull excessively on your nipple; if necessary,
early-onset group B streptococcal (GBS) disease* No medically necessary obstetric procedure
talk to a Reproduced
Source: lactation consultant to evaluate
from Workowski your
KA, nursing
Bolan GA.technique.
Sexually transmitted diseases treatment guidelines, 2015.
IV, intravenously. should be delayed in order to achieve
* Broader spectrum agents, including an agent active against GBS, 4might hoursbe of necessary for treatment
GBS prophylaxis before of delivery. INFECTIOUS
MMWR
• If you Recomm DISEASES
Rep.
have a fever, 2015
the Jun may
doctor 5;64(RR-03):1-137. 2015
prescribe antibiotics for 7–10 days. CDC aSTI
Schedule Treatment
follow- Guidelines
up appointment PID
in 7 days
chorioamnionitis. so that the doctor can check for an abscess. If your symptoms don’t respond within 48 hr of antibiotic treatment,
Newborn management Algorithm now applies to all newborns,
INFECTIOUS
† Doses ranging DISEASES
from 2.5 to 3.0 million units are acceptable for the doses whether administered every
Intra-
or not from GBS- 4 hoursmothers.
Amniotic
positive following
Infection Trichomoniasis
notify the physician.
the initial dose. The choice of dose within that range should be guided byClarificationwhich formulations of penicillin G are Table
Table 7.43.
7.37.
Source:
2015
Reproduced
CDC
2015with
CDC guidelines
guidelines
permission
for
for treatment
treatment
from Hager,
of pelvic
W. David.ofManaging
inflammatory
trichomoniasis disease (PID)
mastitis. Cont Ob/Gyn. 2004:Jan;33-47.
of “adequate” IAP. See full
readily available to reduce the need for pharmacies to specially prepare doses. CDC guidelines for details. Cont Ob/Gyn is a copyrighted publication of Advanstar Communications Inc. All rights reserved.
Parenteral Regimens
INTRA-
CDC, Centers
AMNIOTIC INFECTION
§ Penicillin-allergic patients with a history of anaphylaxis, angioedema, respiratory distress, or urticaria following Non-pregnant Patient Recommended Regimens
administration of for Disease
penicillin orControl and Prevention;
a cephalosporin CFU, colony-
are considered forming
to be units;
at high riskGBS, group B streptococci;
for anaphylaxis and shouldIAP, not Cefotetan 2 g IV
Metronidazole 2 every 12inhours
g orally PLUSdose
a single Doxycycline 100 mg orally or IV every 12 hours
Definition
intrapartum antibiotic
receive penicillin, prophylaxis;
ampicillin, PROM, premature
or cefazolin rupture of membranes.
for GBS intrapartum prophylaxis. For penicillin-allergic patients who do not
Cefoxitin 22g gIVorally
everyin6ahours
have a history
Source: of those with
Reproduced reactions, cefazolin
permission from is the preferred
American agent
College because pharmacologic
of Obstetricians data suggest
and Gynecologists Committeeit achieves
on Tinidazole singlePLUS
doseDoxycycline 100 mg orally or IV every 12 hours
•Obstetric
A bacterial infection of the chorion, amnion, and amniotic fluid often diagnosed during
Practice. ACOG
effective intraamniotic Committee Opinion
concentrations. VancomycinNo. and
485:clindamycin
Prevention of early-onset
should group Bforstreptococcal
be reserved disease
penicillin-allergic womenin
a Clindamycin 900 mg IV every 8 hours PLUS Gentamicin loading dose IV or IM (2 mg/kg), followed by a maintenance
Alternative Regimens:
prolonged
newborns.
at high riskObstet labor.
Gynecol. 2011 Apr;117(4):1019-27. Copyright © 2011 The American College of Ohstetricians
for anaphylaxis.
dose (1.5 mg/kg) every 8 hours. Single daily dosing (3–5 mg/kg) can be substituted.
398
and¶Gynecologists.
If laboratory facilities are adequate, clindamycin and erythromycin susceptibility testing should be performed Metronidazole 500 mgRegimen:
Alternative Parenteral orally twice a day for 7 days
Diagnosis
on prenatal GBS isolates from penicillin-allergic women at high risk for anaphylaxis. If no susceptibility testing is Pregnant Patient Recommended Regimens
Ampicillin/Sulbactam 3 g IV every 6 hours PLUS Doxycycline 100 mg orally or IV every 12 hours
•performed,
Maternal or the results are not
temperature available
100.4° at theC
F/38.0° time of labor,
with vancomycin
no other obvious is source
the preferred agentofforthe
and one GBS intrapar-
following
388
tumadditional
prophylaxis findings:
for penicillin-allergic women at high risk for anaphylaxis. Metronidazole 2
Recommended g orally in a singleRegimens
Intramuscular/Oral dose
◦ ** Resistance to erythromycin is often but not always associated with clindamycin resistance. If an isolate is
Fetal tachycardia Source: Reproduced
Ceftriaxone 250 mg IMfrom
in a Workowski
single dose KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015.
◦
resistant to erythromycin, it might have inducible resistance to clindamycin, even if it appears susceptible to clinda-
Maternal tachycardia
mycin. If a GBS isolate is susceptible to clindamycin, resistant to erythromycin, and testing for inducible clindamycin
MMWR Recomm Rep. 2015 Jun 5;64(RR-03):1-137.
PLUS
◦ Abdominal
resistance tenderness
has been performed and is negative (no inducible resistance), then clindamycin can be used for GBS Doxycycline 100 mg orally twice a day for 14 days
◦ Foul-prophylaxis
intrapartum smelling amniotic fluid
instead of vancomycin. WITH* or WITHOUT
◦ Leukocytosis
Source: Reproduced from Verani JR, McGee L, Schrag SJ; Division of Bacterial Diseases, National Center for Immu-
Metronidazole 500 mg orally twice a day for 14 days
◦
nizationPositive
and Respiratory
amniotic Diseases,
fluid Centers
culturefor Disease Control and Prevention (CDC). Prevention of perinatal group B
streptococcal disease—revised guidelines from CDC, 2010. MMWR Recomm Rep. 2010 Nov 19;59(RR-10):1-36.
INFECTIOUS DISEASES Antibiotic Prophylaxis
Cefoxitin 2 g IM in a single dose and Probenecid, 1 g orally administered concurrently in a single dose
INFECTIOUS DISEASES
Risk Factors Febrile Morbidity and Endomyometritis
shp-gordon-batch3.indd 398 PLUS 12
• Prolonged rupture of membranes 393 ANTIBIOTIC PROPHYLAXIS
Doxycycline 100 mg orally twice a day for 14 days
WITH or WITHOUT
•FEBRILE
Multiple MORBIDITY
vaginal exams in labor
AND and internal monitoring
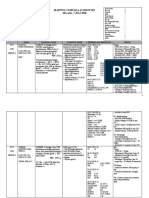
ENDOMYOMETRITIS Table Antimicrobial
7.48. 500 prophylactic regimens by procedure
3.indd 388 Metronidazole
12/1/16 8:28 AM mg orally twice a day for 14 days
Definition
Antibiotics Other parenteral third-generation cephalosporin (e.g., ceftizoxime
Procedure or cefotaxime)Dose (Single Dose)
Antibiotic
• Mezlocillin
Two 4 g IVelevations
temperature q4–6hrs or topiperacillin 3–4 gF;IV
>38° C (100.4° q4hrs the first 24 hours after delivery)
outside PLUS
Hysterectomy Cefazolin† 1 g or 2 g‡ IV
• Ticarcillin/clavulanic
or acid 3.1 g IV q6hrs Doxycycline 100 mg orally twice a day for 14 days
§
• Ampicillin/sulbactam
A temperature of >38.7° 3 gCIV(101.5°
q4–6hrs F) at any time WITH* or WITHOUT
Urogynecology procedures, including those involving mesh Clindamycin plus 600 mg IV
• Ampicillin 2 g IV q6hrs and gentamicin 1.5 mg/kg load then 1.0 mg/kg q8hrs (if delivery by Metronidazole 500 mg orally twice a day for 14 days gentamicin or 1.5 mg/kg IV
Etiology
cesarean section, add clindamycin 900 mg IV q6hrs) 448 quinolone or || 400 mg IV
* The recommended third-generation cephalsporins are limited in the coverage of anaerobes. Therefore, until it is
• Seven Ws of febrile morbidity known that extended anaerobic coverage is not important aztreonam
for treatment of acute 1 g IV
PID, the addition of metronidazole to
Comments
◦Womb (endomyometritis) treatment regimens with third-generation cephalosporins should be considered.
◦
§
Metronidazole plus 500 mg IV
ndd 393 • Some
Windclinicians continue
(atelectesis, antibiotics for 24–48 hours afebrile following delivery.
pneumonia) 12/1/16 8:29 IfAM
allergy precludes the use of cephalosporin therapy, if the community prevalence and individual risk for gonorrhea
◦
• Chorioamnionitis is notinfection
Water (urinary tract an indication for cesarean delivery.
or pyelonephritis) gentamicin
are low, and if follow-up is likely, use of fluoroquinolones for 14 days or 1.5500
(levofloxacin mg/kg IV
mg orally once daily, ofloxacin
◦
• Fetal
Walkoutcome is improved
(deep vein by maternal
thrombosis antibiotic
or pulmonary therapy and ↓ temperature. Give IV fluids
embolism)
daily) can be considered
daily) with||metronidazole
400 mg twice daily, or moxifloxacin 400 mg orally once quinolone 400formg
14IVdays (500 mg orally, twice
◦
andWound
acetaminophen for maternal
(wound infection, and fetal
episiotomy resuscitation.
infection) Laparoscopy None
◦
• Always consider
Weaning other
(breast sources of maternal
engorgement, fever (pyelonephritis,
mastitis, breast abscess) pneumonia, appendicitis).
Source: Reproduced from Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015.
Diagnostic
MMWR Recomm Rep. 2015 Jun 5;64(RR-03):1-137.
◦
• Watch for postpartum
Wonder (drug fever— hemorrhage and dystocia secondary to inadequate uterine action.
wonder drugs) Operative Patient with mastitis or breast engorgement
• Chorioamnionitis may represent a risk factor for cerebral palsy. Tubal
Evaluation MRSA Infections
Sterilization
INFECTIOUS DISEASES
• Physical examination including pelvic exam to rule out hematoma or retained membranes shp-gordon-batch3.indd 448 Laparotomy
Laparotomy Breast segment swollen,
None firm, tender
None 12
• Complete blood count with differential, urinalysis, urine, and blood cultures as indicated MRSA INFECTIONS
Hysteroscopy None
• Chest X-ray, ultrasound as indicated Diagnostic
Chills
Table 7.49. Rates of resistance and dosing of oral agents for treatment of community acquired
Operative No evidence of infection
Treatment MRSAFever to 102°–104° F
infections
Flu-like symptoms
Endometrial ablation
• Cefotetan 1–2 g IV q12hrs
Resistance Typical Adult Oral
Essure
• Mezlocillin 4 g IV q4–6hr or piperacillin 3–4 g IV q4hrs Antimicrobial Agent or Chromotubation
Rates Dosing Doxycycline¶ Comments
Hysterosalpingogram 100 mg orally,
Probable twice daily for 5 days
simple
• Ticarcillin/clavulanate 3.1 g IV q6hrs Infectious mastitis
• Ampicillin/sulbactam 3 g IV q4–6hrs
Clindamycin
IUD insertion 3–24% 300 TIDNone breastbeengorgement
D-test should performed. Excellent
activity against strep. Increasing resistance
• Gentamicin 1.5 mg/kg load then 1.0 mg/kg q8hrs (or 5 mg/kg q24hrs) and clindamycin 900 Endometrial biopsy None
a concern.
mg IV q6hrs (plus ampicillin 2 g IV q6hrs as needed to cover enterococcus) 456
Induced abortion/dilation
Doxycycline Minocycline and evacuation
1
9–24% 100 mgDoxycycline
BID 100 mgand
Doxycycline orally 1 hour before
minocycline. procedure
probably
Perform breast-milk
100 mgMetronidazole
BID activeand 200 tetracycline
against mg orally after procedure
resistant strains.
Comments
394 cultures, leukocyte counts,
Trimethoprim-sulfamethoxazole 0–10%and bacterial
1–2 DScounts
(160/800
500 mg orally, twice daily for 5 days
Low resistance rates in community, reason-
• Continue IV antibiotics until 24–48 hours afebrile and improved physical exam. Urodynamics None
mg) BID able option for empiric therapy.
• Oral antibiotics following IV antibiotics have not been shown to be of proven value. Rifampin <1%device.
IV, intravenously; IUD, intrauterine 600 mg QD Should not be used alone; potential for 7
• If unresponsive following 48–72 hours of IV antibiotics, reexamine the patient. *A convenient time to administer antibiotic prophylaxis is
significant drug interactions.
just before induction of anesthesia.
◦ Consider broadening antibiotic coverage to cover enterococcus if using gentamicin and Fusidic acid <5%Continue nursing
500 mg or
express cefoxitin,
†Acceptable alternatives include cefotetan, milk
TIDmanually Should not be used alone; limited experi-
cefuroxime, or ampicillin-
ence sulbactam.
in children.
clindamycin. ‡A 2-g dose is recommended in women Avoidwith
milka stasis
◦ Consider pelvic abscess. Linezolid
220 lb.
<1% bodymg
600
• hot
mass
PO index
BID greaterExpensive.
compresses
than 35 or weight greater than 100 kg or
◦ Consider septic pelvic thrombophlebitis. §1Antimicrobial
Rates shown are for tetracycline and are • hot
likely to soaks
be <5% or less for doxycycline
agents of choice in women with a history of immediate hypersensitivityand to
minocycline.
penicillin.
◦ Consider drug fever. ||Source: Reproduced
Ciprofloxacin with permission
or levofloxacin from DeLeo FR, Otto M, Kreiswirth BN, Chambers HF. Community-associated
or moxifloxacin.
shp-gordon-batch3.indd 456 methicillin-resistant Staphylococcus aureus. Lancet. 2010 May 1;375(9725):1557-68. Copyright © 2010 Elsevier.
¶If patient has a history of pelvic inflammatory disease or procedure demonstrates dilated fallopian tubes. No
12
Treat iswith
prophylaxis antibiotics
indicated for a study without dilated tubes. Symptoms still present after 48 hours
3.indd 394 12/1/16 11:08 AM Reproduced with permission from ACOG Committee on Practice Bulletins—Gynecology. ACOG Practice
Source:
Bulletin No. 104: Antibiotic prophylaxis for gynecologic procedures. Obstet Gynecol. 2009 May;113(5):1180-9.
Copyright © 2009 The American College of Obstetricians and Gynecologists.
You might also like
- Grabovoi Numbers for Healing and RegenerationDocument23 pagesGrabovoi Numbers for Healing and RegenerationAna BrunetteNo ratings yet
- Understanding Urinary Tract Infections and Kidney StonesDocument4 pagesUnderstanding Urinary Tract Infections and Kidney StonesJamesNo ratings yet
- Prevention of Group B Streptococcal Early-Onset Disease in Newborns - ACOGDocument66 pagesPrevention of Group B Streptococcal Early-Onset Disease in Newborns - ACOGxemdoan044No ratings yet
- The Effect of Probiotics in Prevention of Necrotising Enterocolitis in Preterm Neonates in Comparison With Control GroupDocument4 pagesThe Effect of Probiotics in Prevention of Necrotising Enterocolitis in Preterm Neonates in Comparison With Control GroupchachaNo ratings yet
- csDMARD Safety in Pregnancy and LactationDocument10 pagescsDMARD Safety in Pregnancy and Lactationyuliana160793No ratings yet
- Azithromycin Vs Erythromycin For The Management of Preterm Premature Rupture of MembranesDocument8 pagesAzithromycin Vs Erythromycin For The Management of Preterm Premature Rupture of Membranesizza istqmhNo ratings yet
- Chirorab Prescribing InformationDocument2 pagesChirorab Prescribing Informationsr bNo ratings yet
- Drug Study Batch 3 - Kristele Marie Joy CuaDocument26 pagesDrug Study Batch 3 - Kristele Marie Joy CuaKristele Marie Joy CuaNo ratings yet
- Diagnosis Treatment and Prevention of Typhoid Fever in Adults 2017Document11 pagesDiagnosis Treatment and Prevention of Typhoid Fever in Adults 2017Khayla Ray RondobioNo ratings yet
- 2.14 Management of GBS Positive in PregnancyDocument2 pages2.14 Management of GBS Positive in PregnancyZarif SyafiqNo ratings yet
- Antibiotic treatment of common bacterial gastroenteritisDocument1 pageAntibiotic treatment of common bacterial gastroenteritisfionaNo ratings yet
- Infeksi Saluran KemihDocument2 pagesInfeksi Saluran KemihFredNo ratings yet
- Tetanus Immune Globulin (Human) : Revision Date: May 27, 2013Document3 pagesTetanus Immune Globulin (Human) : Revision Date: May 27, 2013DrscottmccallNo ratings yet
- Azithromycin Medication PDFDocument1 pageAzithromycin Medication PDFmp1757No ratings yet
- DocumentDocument5 pagesDocumentPRECIOUS LOVE LAGRIMASNo ratings yet
- Uterine Adenocarcinoma in Mice Treated NDocument5 pagesUterine Adenocarcinoma in Mice Treated NAmeer MohammadNo ratings yet
- Cephalexin Drug Study RNpedia ComDocument2 pagesCephalexin Drug Study RNpedia ComTaraKyleUyNo ratings yet
- Cefuroxime Drug Study GuideDocument12 pagesCefuroxime Drug Study GuideAUBREY MARIE . GUERRERONo ratings yet
- National Immunization Program (NIP) : Mary Ann E. Lopez MAN RN LPTDocument26 pagesNational Immunization Program (NIP) : Mary Ann E. Lopez MAN RN LPTJanaica JuanNo ratings yet
- Guidelines For The Diagnosis and Management of Cow's Milk Protein Allergy in InfantsDocument8 pagesGuidelines For The Diagnosis and Management of Cow's Milk Protein Allergy in InfantsgladyannNo ratings yet
- Amoxicillin (Amoxycillin) : PresentationDocument4 pagesAmoxicillin (Amoxycillin) : PresentationRavikiran SuryanarayanamurthyNo ratings yet
- Rabies ImmunizationDocument40 pagesRabies Immunizationruiza corcinoNo ratings yet
- Phcist Letter Sept 2006Document52 pagesPhcist Letter Sept 2006MichelNo ratings yet
- Cephalexin dosage, mechanism of action, adverse effectsDocument1 pageCephalexin dosage, mechanism of action, adverse effectsJoover AquinoNo ratings yet
- Pprom ProtocolDocument3 pagesPprom ProtocolLana kamalNo ratings yet
- Intravenous Immunoglobulin - How To Use It: Therapeutic InterventionDocument5 pagesIntravenous Immunoglobulin - How To Use It: Therapeutic Interventionsrajan sahuNo ratings yet
- Probiotics For The Treatment or Prevention of Atopic DermatitisDocument11 pagesProbiotics For The Treatment or Prevention of Atopic DermatitistarsiahningsihNo ratings yet
- Las 7 PcolDocument47 pagesLas 7 Pcoljenet soleilNo ratings yet
- Cephalexin Nursing GuideDocument2 pagesCephalexin Nursing GuideKatyana Cesar100% (1)
- Drug StudyDocument4 pagesDrug Studymyka.legaspi21No ratings yet
- Cefuroxime 1Document3 pagesCefuroxime 1Gwyn RosalesNo ratings yet
- Gastro PDFDocument6 pagesGastro PDFAvrianne NicoleNo ratings yet
- ACOG Fetal Maturity Guidelines PDFDocument8 pagesACOG Fetal Maturity Guidelines PDFinayahsyNo ratings yet
- College of Nursing: Cebu Normal UniversityDocument7 pagesCollege of Nursing: Cebu Normal UniversityGwyn RosalesNo ratings yet
- Probiotics For The Management of Pediatric.22Document16 pagesProbiotics For The Management of Pediatric.22Diana MartinezNo ratings yet
- Immunisation and Under 5 CardDocument31 pagesImmunisation and Under 5 CardStephen AngelNo ratings yet
- Misoprostol: (Mye Soe Prost' Ole) Diarrhea, Abdominal Pain, Flatulence, VomitingDocument4 pagesMisoprostol: (Mye Soe Prost' Ole) Diarrhea, Abdominal Pain, Flatulence, VomitingThrecia RotaNo ratings yet
- Management Infant SepsisDocument10 pagesManagement Infant SepsisPutri HolmesNo ratings yet
- 11092022119226070042Document9 pages11092022119226070042Alya BarrotNo ratings yet
- Measles PHIDSPILDocument5 pagesMeasles PHIDSPILriczen mae vilaNo ratings yet
- ETS TX OMSDocument24 pagesETS TX OMSAline MirandaNo ratings yet
- Generic Name: BeforeDocument2 pagesGeneric Name: BeforeFranz Earl Niño AlbesaNo ratings yet
- Guidelines For The Diagnosis and Management of Cow's Milk Protein Allergy in InfantsDocument9 pagesGuidelines For The Diagnosis and Management of Cow's Milk Protein Allergy in InfantsBayu DestiawanNo ratings yet
- Nelson Antibioticos NEO 2023Document32 pagesNelson Antibioticos NEO 2023Lina Mariset Delgado GarzonNo ratings yet
- Pelvic Pain, Food Allergies, Thyroid Disease, Mpox, Chronic Fatigue Syndrome, Alloimmunization (AAFP 2023)Document1 pagePelvic Pain, Food Allergies, Thyroid Disease, Mpox, Chronic Fatigue Syndrome, Alloimmunization (AAFP 2023)Breno Resende Rodrigues CunhaNo ratings yet
- Atopic Dermatitis: Role of Food House Dust Mite Allergens: MethodsDocument7 pagesAtopic Dermatitis: Role of Food House Dust Mite Allergens: MethodsLediraNo ratings yet
- Bacterial VaccineDocument44 pagesBacterial VaccineShrenik LuniyaNo ratings yet
- Tatalaksana Alergi Susu SapiDocument7 pagesTatalaksana Alergi Susu SapiAyatullah MuhammadNo ratings yet
- Day 2 BSV MDR infections_HensonDocument37 pagesDay 2 BSV MDR infections_HensonRye CalderonNo ratings yet
- Drug StudyDocument5 pagesDrug StudyinjilbalazoNo ratings yet
- Medical Treatment For Pyometra in DogsDocument5 pagesMedical Treatment For Pyometra in DogsNatasha ImanuelleNo ratings yet
- Jurnal 882Document1 pageJurnal 882saddamNo ratings yet
- Group B StreptococcusDocument8 pagesGroup B StreptococcusMary QuinnNo ratings yet
- Ncbi NLM Nih Gov@pmc2760892Document2 pagesNcbi NLM Nih Gov@pmc2760892aisyahNo ratings yet
- Efficacy+of+IgM+Rich+Immunoglobin+for+Bacterial+Sepsis (Case Control)Document6 pagesEfficacy+of+IgM+Rich+Immunoglobin+for+Bacterial+Sepsis (Case Control)Tristiani UtariNo ratings yet
- Vigabatrin For IsDocument12 pagesVigabatrin For IsAndrew SantosoNo ratings yet
- Early Onset Neonatal Sepsis. Diagnostic Dilemmas and Practical ManagementDocument6 pagesEarly Onset Neonatal Sepsis. Diagnostic Dilemmas and Practical Managementlink0105No ratings yet
- Prescribed dosage and administration of Suprax antibioticDocument3 pagesPrescribed dosage and administration of Suprax antibioticHavier EsparagueraNo ratings yet
- Chapter 2 - Antimicrobial Therapy For Head and Neck InfectionDocument13 pagesChapter 2 - Antimicrobial Therapy For Head and Neck InfectionMario CastanedaNo ratings yet
- Orthopaedic Infection in Adults UHL GuidelineDocument10 pagesOrthopaedic Infection in Adults UHL GuidelineFadlu ManafNo ratings yet
- Drug Study: Adult: ChildDocument4 pagesDrug Study: Adult: ChildKristian Karl Bautista Kiw-isNo ratings yet
- Antimicrobial Therapy in Veterinary MedicineFrom EverandAntimicrobial Therapy in Veterinary MedicineSteeve GiguèreRating: 4 out of 5 stars4/5 (1)
- Trasplante Renal y Gestacion PDFDocument7 pagesTrasplante Renal y Gestacion PDFRenato SánchezNo ratings yet
- STD SurvRpt 2018 All Slides - FDocument96 pagesSTD SurvRpt 2018 All Slides - FRenato SánchezNo ratings yet
- Partograma para PrincipiantesDocument59 pagesPartograma para PrincipiantesRenato SánchezNo ratings yet
- Trasplante Renal y GestacionDocument7 pagesTrasplante Renal y GestacionRenato SánchezNo ratings yet
- Dengue Fever and PregnancyDocument6 pagesDengue Fever and PregnancyImanuel Far-FarNo ratings yet
- Pci 5s PCM 5s Data Sheet (Gps g5 Ps5 07002)Document14 pagesPci 5s PCM 5s Data Sheet (Gps g5 Ps5 07002)Renato SánchezNo ratings yet
- 2010ACOG CompendiumDocument1,629 pages2010ACOG CompendiumRenato SánchezNo ratings yet
- ALBUTEROLDocument1 pageALBUTEROLAnna LaritaNo ratings yet
- Unicom Product and Price ListDocument6 pagesUnicom Product and Price ListImanoelClousAndohNo ratings yet
- Stok BHP Ruang Icu RSPHDocument2 pagesStok BHP Ruang Icu RSPHAbdul LatiifNo ratings yet
- PMSMA Excel FORMATSDocument10 pagesPMSMA Excel FORMATSsri sri100% (1)
- Pengantar Interaksi Obat: Drug InteractionDocument21 pagesPengantar Interaksi Obat: Drug InteractionFaykar RezaNo ratings yet
- Fetal DistressDocument33 pagesFetal DistressYara H QaisiNo ratings yet
- Tabel Harga ObatDocument12 pagesTabel Harga ObatChristiana TamatompoNo ratings yet
- Sample Concept MapDocument1 pageSample Concept MapAndrea SolumNo ratings yet
- 7 - Painful JointsDocument12 pages7 - Painful JointsRawabi rawabi1997No ratings yet
- RSUD Cileungsi Laporan Penerimaan Obat Generik Januari 2018Document98 pagesRSUD Cileungsi Laporan Penerimaan Obat Generik Januari 2018dianNo ratings yet
- DRUg StudyDocument9 pagesDRUg Studyluwiee100% (1)
- Divine Interventions - Military Podcast 231Document1 pageDivine Interventions - Military Podcast 231María Camila Pareja ZabalaNo ratings yet
- Delayed walking in young children matching questionsDocument8 pagesDelayed walking in young children matching questionsfasdNo ratings yet
- DOMINGO - OB RequirmentsDocument10 pagesDOMINGO - OB RequirmentsJick Esteva de VicenteNo ratings yet
- 100MCQsinTropicalMedicine (PDF Library)Document76 pages100MCQsinTropicalMedicine (PDF Library)Abdalla ShibailiNo ratings yet
- Daftar Pustaka: Foster, S., 2017, Stevens - Johnson Syndrome, American Association of ImmunologistsDocument2 pagesDaftar Pustaka: Foster, S., 2017, Stevens - Johnson Syndrome, American Association of ImmunologistsSuci RachmawatiNo ratings yet
- Pediatric Pharyngotonsillitis Sore ThroatDocument5 pagesPediatric Pharyngotonsillitis Sore Throatdef_10No ratings yet
- IMCI Post TESTDocument7 pagesIMCI Post TESTeric100% (1)
- Harga ObatDocument21 pagesHarga ObatRizamdhani AptNo ratings yet
- Fluoroquinolones Mechanism Action Uses Side EffectsDocument2 pagesFluoroquinolones Mechanism Action Uses Side EffectsHlaSoe WinNo ratings yet
- Drug MacrobidDocument1 pageDrug MacrobidSrkocherNo ratings yet
- Laporan Bulanan Rekapitulasi Surveilans Terpadu Penyakit (STP) Baru Di Puskesmas Dan Jejaringnya Puskesmas SoliuDocument37 pagesLaporan Bulanan Rekapitulasi Surveilans Terpadu Penyakit (STP) Baru Di Puskesmas Dan Jejaringnya Puskesmas SoliuVictoria YanersNo ratings yet
- Hormonal Contraception PDFDocument28 pagesHormonal Contraception PDFSini AbrahamNo ratings yet
- Glomox PilDocument1 pageGlomox Pilpharmacia1.comNo ratings yet
- Preterm Labor. SummaryDocument3 pagesPreterm Labor. SummaryLanaNo ratings yet
- Rwanda Medicaments EssentielsDocument85 pagesRwanda Medicaments EssentielsportosinNo ratings yet
- Mapping Cempaka Ii Obstetri Selasa, 7 Juli 2020: HYS 207.2 SNR 207.3 DST 209.1 MGP 211.4 BYM 209.3Document4 pagesMapping Cempaka Ii Obstetri Selasa, 7 Juli 2020: HYS 207.2 SNR 207.3 DST 209.1 MGP 211.4 BYM 209.3Ayu Putri HitasariNo ratings yet
- ImpetigoDocument1 pageImpetigoshailesh284No ratings yet