Professional Documents
Culture Documents
Diabetic Foot Care Behaviors: A Literature Review: Titis Kurniawan, Imas Rafiyah, Ardia Putra, Yanuar Primanda
Uploaded by
nadya wahyu0 ratings0% found this document useful (0 votes)
31 views7 pagesArdia
Original Title
Ardia_prosiding
Copyright
© © All Rights Reserved
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentArdia
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
31 views7 pagesDiabetic Foot Care Behaviors: A Literature Review: Titis Kurniawan, Imas Rafiyah, Ardia Putra, Yanuar Primanda
Uploaded by
nadya wahyuArdia
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 7
Diabetic Foot Care Behaviors: A Literature Review
Titis Kurniawan1,2*, Imas Rafiyah1,2, Ardia Putra1,3, Yanuar Primanda1,4
1
Master student, Master of Nursing Science (International Program), Faculty of Nursing, Prince of Songkla University,
P.O. Box 9, Khor Hong, Hatyai, Songkhla, 90112, Thailand
2
Lecturer of Faculty of Nursing, Universitas Padjadjaran, Jl. Raya Bandung-Sumedang Km 21, Jatinangor, West-Java,
45363, Indonesia
3
Lecturer of Nursing Science Program, Medical Faculty, Syiah Kuala University, Gedung Petronas, Jl. Tgk. Tanoeh
Abee, Darussalam, Banda Aceh, 23111, Indonesia
4
Lecturer of Nursing Science Program, Faculty of Medicine and Health Science, Muhammadiyah University of
Yogyakarta, Jl. Lingkar Barat, Tamantirto, Kasihan, Bantul, Yogyakarta, 55183, Indonesia
*Corresponding author, E-mail: titiz_kazep@yahoo.com
Abstract—Diabetic other hand, diabetic foot this review are to outline color, dryness, thickness,
foot care behaviors are one ulcer treatment is the diabetic foot care fissures, or cracking. To
of essential component of challenging, costly, time behaviors components, ensure all part of foot were
diabetic foot ulcer consuming [2,3,4], and contributing factors, assessed properly, the
prevention. It facilitates
early detection of foot
often requires foot assessment, and diabetic diabetic patients suggested
abnormalities and allows amputation [5]. It was foot care behaviors using mirror.
early treatment that reported that almost 32% improvement program. 2). Peripheral
produce bigger opportunity of diabetic patient with neuropathy assessment.
for better outcomes. foot ulcer ended up with II. METHOD This assessment is
However, many of diabetic such types of foot The including thermal
patients were not perform amputation [6]. http://lib.med.psu.ac.th/lib sensation, pain sensation,
this practice properly. The Depressingly, evidences medeng/ was used as the numbness, or autonomic
aims of this review are to
showed that diabetes main channel to search damage.
describe the diabetic foot
care behaviors components, related foot amputation is related journals, articles,
3). Vascular
contributing factors, closely related to physical and other comprehensive
impairment assessment.
assessment, and diabetic disability, depression, reports from the classic
This assessment including
foot care behaviors financial burdens, poor nursing and health-related
assessing warm skin,
improvement program. A quality of life, and high databases such as
relevant literature searched distended vein and foot
mortality [4,7,8]. Thus, PubMed, Cumulative
from databases: PubMed, pulses.
DFU prevention is very Index to Nursing and
CINAHL, the Cochrane important. Allied Health (CINAHL), 4). Foot posture and
and ProQuest Medical
Library, and Science Direct the Cochrane Library, and shape assessment.
Additionally,
were conducted. It was Science Direct. The Activities including
once diabetes peripheral
found that diabetic foot numbers of keywords investigating of claw toes,
neuropathy (DPN) is
care behaviors basically were used to obtain those metatarsal heads, or
developed, diabetes
consist of simple activities articles including diabetic Charcot joint.
that predict had significant patients’ feet are easily
foot care, foot ulcer, foot
benefits in preventing developing foot ulceration. 5). Callus and
care practice, and foot
diabetic foot ulceration. Some of the patients’ daily blister assessment. This
ulcer prevention.
Foot care behaviors activities, such as walking assessment focused on the
influenced by several bare foot, footwear, and III. DIABETIC FOOT CARE plantar pressured point
factors including patients’ trimming toenails are BEHAVIORS COMPONENTS including the site, size,
age, gender, knowledge, foot impending causes of foot and the appearance of
care education experiences, Diabetic foot care
ulcer. However, since the callus or blister.
foot care education and foot behaviors simply defined
patients unable to sense
examination that conducted as the daily activities to 6). Infection or
by healthcare providers, the pain caused by
assess or examine foot inflammation assessment.
and resources availability. injuries, foot ulcer become
conditions and apply some It especially aimed to
With regard to the insensible injury and most
recommended actions to identify the between toes
important of foot care of patients just know the
maintain and improve foot area and the moist part of
behaviors in preventing ulcer after it developed
diabetic foot ulceration, it conditions or minimize the each foot.
such degree of infection
was recommended for risk based on the
[9]. These situations 7). Assessment of
healthcare providers to assessment findings [15].
emphasize that daily foot ulceration. This
regularly assess patients’ Generally, it consists of
foot care knowledge and
inspection is very assessment includes
foot assessment and foot
behaviors and apply the important. Daily foot assessment of the foot
care.
certain strategies to inspection allows patient ulcer site, appearance,
improve patients’ foot care early detect any foot A. Foot Assessment size, infection signs, and
knowledge and behaviors abnormalities that This activity is exudation.
properly. eventually provides large purposed to identify the B. Foot Care
Keywords-component; opportunity to prevent foot major causes of foot
diabetic foot care, foot ulcer, ulceration. It was noted This activity
ulceration including foot
foot ulcer prevention. that patients who consists of any
peripheral neuropathy,
performed proper foot care recommended actions to
vascular problem, and foot
I. INTRODUCTION had significantly lower maintain foot conditions
pressure. There were some
risk of foot ulceration than and/or minimize foot ulcer
Diabetic foot recommended points in
those who did not [10,11]. risk factors. Those
ulcer (DFU) is the the foot assessment as
Unfortunately, previous recommended foot care
commonest diabetic followed [15, 16]:
studies showed that many activities were include as
complications. It affects 1). Foot skin follows [17,18,19]:
diabetic patients did not
almost 15% to 25% of assessment. These
perform it properly [11,
diabetic patients [1]. In the activities include skin
12, 13]. The objectives of
1). Foot hygiene. not able to be safely
patients’ characteristics
accommodated in
The foot should be kept in that significantly
shoes. Continue
clean, dry, and soft. 4). Avoiding extreme patientassociated
education. with greater
Patients are suggested to temperatures. Check the basic foot care were
2 PAD + Consider prescriptive
wash the foot daily by temperature of LOPS younger age, African-
or accommodative
using mild soap and pour water/shower before used. American
footwear. background,
(warm not hot) water and However, because patients higher
Consider vasculareducation, more
soft washcloth. Avoid mostly experience loss- consultation
severefor foot neuropathy,
combined follow-up.
soaking feet more than 4 sensation because of and having experience of
minutes and drying all neuropathy, they may be 3 History of Same foot
as category
ulcer1. [13]. Another
ulcer or Consider vascular
parts the foot including unaware of thermal injury. study noted that there were
amputation consultation for
between toes area gently If possible, put water combined follow-updifferent
significant if of foot
by using soft and clean thermometer in the care
PAD present. behaviors and
towel, especially between bathroom to ensure that Abbreviations: PAD = peripheral
understanding between
areas. To keep skin foot the water is in the artery diseases and LOPS = loss American Indian/Pacific
moist, apply a proper/tolerable of protective sensation. Source: Islanders, Asians, and
moisturizing lotion after temperature. Boulton et al. (2008). African Americans [21].
washing.
5). Attending on the IV. DIABETIC FOOT CARE C. Complication of
2). Selecting and regular health BEHAVIORS Diabetes Mellitus
wearing fitted footwear. It professional foot CONTRIBUTING FACTORS Complication of
was suggested to use examination. During the diabetes mellitus influence
proper cushion footwear, regular check up, patient is A. Patients’ Knowledge
patients’ foot care
athletic shoes, footwear suggested to promptly and Foot Care Education.
behaviors in negative and
with laces, velcro, or report foot problems to the In one study positive direction.
buckles, and avoiding healthcare professional stated that one of the Negatively, DM
pointed-toe, open-toe such as infection, ulcer, barriers of performing foot complication may develop
shoes, high heels, sandals, cuts that do not heal, and care properly is patients’ any physical disabilities
and un-breathable and other abnormal findings lack of knowledge [20,21]. that reduce patients’
inelastic materials. that they find during daily Inherent, the evidences capacity to perform foot
assessment (redness, mostly suggested that care practice properly. In
3). Toenails
drainage, swelling, pain or educational program one study identified that
trimming and care. This
dark discoloration). Also improve patients’ some barriers of
foot care action only
suggested for patients to knowledge and foot performing foot care
suggested for the patients
ask any advises from behaviors [22, 23]. In practice were included
who able to reach and cut
nurses or primary care addition, it was noted that vision problem, joint
the toe nails properly.
providers when superficial repeated exposure to the problem, and excess
Cutting the toenails
cuts, scratches, and educational program weight [21]. In contrast,
carefully using proper nail
blisters that do not heal in improved patients’ complication also may
cutter/nail clipper,
three days. The attending adherence to perform improve patient awareness
following to the shape of
comprehensive foot proper foot care. Diabetic to perform foot care more
the toes, avoid cut the
examination frequencies patients who participated properly in order to
nails too close to the skin
will different for each in more than three minimize the
of toenails bed, and avoid
patient depends on their education programs complications that already
cutting down the corners
risk factors severity. practiced had significantly developed [24].
or skin at the end of
Patients’ risk factors better self foot care than
toenails (see Figure 1). In D. Foot Care Education
classification and scoring patients who had no or
addition, it is suggested to and Foot
is as followed [16]: only one training program
perform nail cutting after Examination from
[13, 24]
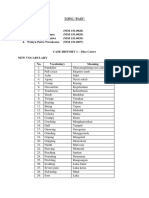
soaking feet (after a bath TABLE I. RISK CLASSIFICATION Healthcare Providers
or shower). When find BASED ON THE COMPREHENSIVE B. Patients’
FOOT EXAMINATION In the study
toenails are ingrown, Characteristic
Risk Definition Recommended identified that patients
thickened, or infected, it One study
Category who received foot care
should be treated and showed that man was
0 No LOPS, Patient education education and their feet
trimmed by a healthcare no PAD, no includingmore
advice confident
on in their had been examined by
professional. deformity appropriate footwear
ability to manage their healthcare providers were
diabetes, reported fewer more likely to check their
1 LOPS+ Consider prescriptive
lapse in foot care, reported
deformity or accommodative
feet regularly [26].
higher quality of life, and
footwear E. Resources
overall better treatment
Consider prophylactic
surgerysatisfaction [25]. The other
if deformity is Availability
It was identified 51-item [28]. It was behaviors. Foot care Regarding the
that lack of foot care implemented with 100 practice section comprised components measured,
equipments such as mirror, diabetic patients and 61 foot self-examination (4 NAFF and DisFoKaPS-32
foot-stool, and nail cutter healthy volunteers in out- questions), foot wear (3 seem more comprehensive
would inhibit patients to patients department. The questions), toenails care (2 than SDSCA. In addition,
perform self-foot care internal consistency was questions), and foot NAFF and DisFoKaPS-32
properly [13]. Without 0.46 and 0.39 in people hygiene (7 questions). The have some similarities
those equipments may with diabetes and in content validity was including used foot
hinder them to perform healthy volunteers, approved by five inspection, foot hygiene,
some foot care techniques respectively. From this, physicians and one nurse footwear, preventing foot
properly. 28 items were found and tried-out with diabetic injuries,
significant differences patients. However, there toenails/callus/corn care
Based on all of between each group. The was no report regarding and moisturizing foot skin
those findings, it can be instrument was then reliability test of this to measure foot care
generalized that patients’ revised into 29 items and questionnaire. behaviors. However, since
foot care behaviors are consists of foot assessment the NAFF developed in
C. Summary of Diabetes
influenced by three major (2 questions), foot wear European country, the
Self-Care Activities
factors, namely: patients’ (13 questions), foot measurement items may
(SDSCA)
related factors, health care hygiene (3 questions), not fit to measure foot care
Questionnaire
providers’ related factors, prevent foot injury (7 behaviors in non-European
and resources availability questions), toenails, The SDSCA is a countries.
related factors. callus/corn care (2 brief self-report
questions), and questionnaire to assess VI. DIABETIC FOOT
V. DIABETIC FOOT CARE wound/ulcer care (2 diabetes self-management CARE BEHAVIORS
BEHAVIORS ASSESSMENT questions). The internal including: general diet, IMPROVEMENT PROGRAM
Patients’ self- consistency was 0.53 and specific diet, exercise,
According to the
report (questionnaire) on there was a significant blood-glucose testing, foot
evidences from the
perceived foot care correlation (γ = 0.83; p < care, and smoking [30]. In
previous studies, there
behaviors were generally 0.001) and no significant addition, Toobert and
were 10 studies (5 RCTs, 2
used in the previous difference (p = 0.85) colleagues reported the
quasi experiments studies,
studies to measure the between scores in the test- high internal consistency-
and 3 systematic reviews)
outcome of patients’ foot retest study. However, reliability of the 5
evaluated the effectiveness
care behaviors. since this instrument categories of this tool (γ =
of diabetic foot care
Observational method was developed and utilized in 0.47) with an exceptional
program in improving foot
also used in combination European countries, of the specific diet test-
care behaviors and
with patients’ self-report in utilization in other regions retest correlations were at
preventing foot ulcer.
evaluating foot care is therefore needed to be moderate level (γ = 0.40).
Even though there were
behaviors [27], modified to fit with Furthermore, SDSCA
some limitations regarding
unfortunately there was no context and culture. questionnaire was a brief,
the methodological issues,
clearly explanation reliable, and valid self-
B. DisFoKaPS-32 all evidences suggested
regarding this technique. report measure of diabetes
Questionnaire that educational program
The published self-management
that combined with follow
questionnaires had been This (included foot care
up, consultation, and
developed to evaluate foot questionnaire was practice) and suggested to
providing printed material
care behaviors were developed by Khamseh use both for research and
were effectively improved
including Nottingham and colleagues in 2007 clinical practice. The
patients’ foot care
Assessment of Functional based on foot care limitation of this
knowledge and behaviors.
Foot-care Questionnaire principle, their instrument might be
Accordingly, the
(NAFF), DisFoKa-32, and experiences as healthcare detected at the few items
systematic reviews
summery of diabetes self- providers, and the of foot care behaviors
reported that trials in this
care activity (SDSCA). recommendations from the questions that consisted of
arena considerably
American College of Foot two questions regarding
A. Nottingham Assessment improved patients’ foot
and Ankle Surgeons and patient’s practice in
of Functional Foot- care knowledge and
the British Diabetes checking their foot and
care Questionnaire behaviors however most
Association [29]. It was inspecting inside part of
(NAFF) of those studies had lower
originally developed in footwear. So, it might be
internal validity and high
This instrument Persian Language version not represent the whole
risk of bias [23, 31,32].
was developed by Lincoln and consisted of 16 picture of diabetic foot
and colleagues in 2007 questions on knowledge care behaviors Regarding the
and primarily consisted of and 16 items of foot care components. follow up strategies used,
most of those studies efficacy [38], improved almost of those studies [3] W. J. Jeffcoate, and
utilized telephone call, patients’ perceptions of were conducted in the K. G. Harding,
card reminder, home visit, barrier, benefit, severity, western countries. “Diabetic foot ulcer,”
and face-to-face followed threat, and susceptibility Therefore, the program Lancet, vol. 361, pp.
up as schedule at clinic/ of foot care [27], and and measurement used 1545–1551, 2003.
outpatient department improved patients’ self- may not produce similar [4] G. Ragnarson-
during regular check up. management behaviors effect when it was applied Tennvall and J.
Regarding the phone call [36,40]. However, effect in the countries with Apelqvist, “Health-
follow up, some other of diabetic foot care different characteristic/ economic
studies reported that phone programs on patients’ cultural background. consequences of
call intervention for giving mood and quality of life diabetic foot
health education and/or were not found [27]. Also, VIII. RECOMMENDATION lesions,” Clinical
follow-up effectively did not reach statistical Based on Infectious Diseases.
improved patients’ significant in term of evidences outlined, it is Vol. 39 pp. S132–
behaviors [33, 34, 35]. diabetic foot care program suggested for every S139, 2004.
on reducing foot ulcer or healthcare provider who [5] Canadian Diabetes
In the educational
incidences, particularly in treats diabetic patients to Association [CDA],
strategies, most of the
high risk patients [27, 39]. regularly assess patients’ “Approached
previous studies provided
current foot care treatment of a patient
diabetic foot care VII. CONCLUSION knowledge and behaviors with diabetic ulcer,”
programs as an individual
Overall, foot care and apply certain Available at
(face-to-face) or a group
behaviors are one of the improvement program/ http://www.diabetes.
that combined with
important components of strategy to enhance patient ca/, 2005.
demonstration, discussion,
foot ulcer prevention. foot care knowledge and [6] N. Tantisiriwat and
providing leaflet/booklet,
Unfortunately, the behaviors in order to S. Janchai,
providing other
evidences suggested that prevent diabetic foot “Common problems
motivational sessions, or
many diabetic patients did ulceration. in diabetic foot
providing consultation or
not perform foot care clinic,” Journal of
couching. The efficacy of ACKNOWLEDGMENT
practice properly. It was Medical Association
using individual and group
also identified that Thailand, vol. 7, pp.
diabetic foot care program I would like to
diabetic foot care 1097-1101, 2008.
showed that group thank to the Directorate of
behaviors were influenced Higher Education, [7] M. Abdelgadir, W.
approach was more
by many factors, such as Ministry of National Shebeika, M. Eltom,
effective than individual
patients’ knowledge, foot Education of Republic of C. Berne, and K.
approach [36]. In other
care education experience, Indonesia for giving me Wikblad, “Health
study noted that
DM complications, foot scholarship to continue my related Quality of
effectiveness of group
care education and study in Faculty of life and sense of
approach (4-8
examination from Nursing, Prince of Songkla coherence in
patient/group) was equally
healthcare providers, and University, Thailand. Sudanese diabetic
effective in improving the
resources availability. subjects with lower
outcomes and may allow REFERENCES
Fortunately, most of those limb amputation,”
other benefits regarding
factors were modifiable Tohoku Journal of
time and cost [38]. [1] N., Singh, D. G.,
and several foot care Experimental
Armstrong, and B. Medicine, vol. 217,
There were improvement programs
A. Lipsky, pp. 45-50, 2008
several measured showed effectively
“Preventing foot [8] K. Stockl, A.
outcomes evaluated in the improved patients foot
ulcers in patients Vanderplas, E.
previous studies. Those care knowledge and
with diabetes,” The Tafesse, and
outcomes were ulcer/ behaviors. Generally, the
Journal of the E.Chang, “Costs of
diabetic foot program provided was
American Medical lower-extremity
problem/amputation, combination of interactive
Association, Vol. ulcers among
patients’ foot care educational session with
293, pp. 217-228, patients with
knowledge, and patients’ others strategies including
2005. diabetes,” Diabetes
foot care behaviors. Those follow-up phone call,
[2] M. Edmonds, Care, vol. 27, pp.
studies revealed that all of booklet, motivation and
“Diabetic foot 2129–2134, 2004.
the diabetic foot care counseling strategies.
ulcers: practical [9] J. H. Calhoun, K. A.
programs improved Even though the previous
treatment Overgaard, C. M.
patients’ foot care evidences showed
recommendations,” Stevens, J. P .F.
knowledge and behaviors effectively improved
Drugs, vol. 66, pp. Dowling, and J. T.
[27, 22, 36, 38-41], patients’ foot care
913-929, 2006. Mader, “Diabetic
enhanced patients’ self knowledge and behaviors,
Foot Ulcers and Unit Rawat Jalan 26, pp. 250-263, Nursing, vol. 17, pp.
Infections: Current Rumah Sakit Umum 2010. 2920–2926, 2008.
Concepts,” Advances Daerah Sumedang [20] H. B. Chandalia, [25] R. Rubin, and M.
in Skin & Wound (Primary prevention D.Singh, V. Kapoor, Peyrot, “Men and
Care, vol. 15, pp. 31- of diabetic foot S. H. Chandalia, and diabetes-
45, 2002. ulceration among P. S. Lamba, psychological and
[10] A. L. Calle-Pascual, diabetic patients in “Footwear and foot behavioural issues,”
A. Duran, A. Outpatient Unit of care knowledge as Diabetes Spectrum,
Beneda, M. I. Calvo, Sumedang District risk factors for foot vol. 11, pp. 81-87,
A. Charro, J. A. General Hospital),” problems in Indian 1998.
Diaz, et al., Unpublished diabetics,” [26] G. De Berardis, F.
“Reduction in Foot research. Universitas International Journal Pellegrini, M.
Ulcer Incidence,” Padjadjaran, of Diabetes in Franciosi, M.
Diabetes Care, vol. Indonesia, 2010. Developing Belfiglio, B.
24, pp. 405-407. [15] American Diabetes Countries, vol. 28, DiNardo, S.
2001. Association [ADA], pp. 109 – 113, 2008. Greenfield et al.,
[11] P. Jayaprakash, S. “Preventive foot care [21] J. M. Olson, M. T. “Physician attitudes
Bhansali, A. in people with Hogan, L. M. toward foot care
Bhansali, P. Dutta, diabetes,” Diabetes Pogach, M. Rajan, education and foot
and R. Care, vol. 25 (suppl G. J. Raugi, and G. examination and
Anantharaman, 1), pp. 69–70, 2003. E. Reiber, “Foot care their correlation with
“Magnitude of foot [16] A. J. M. Boulton, D. education and self patient practice,”
problems in diabetes G. Armstrong, S. F. management Diabetes Care, vol.
in the developing Albert, R. G. behaviors in diverse 27, pp. 286-287,
world: a study of Frykberg, R. veterans with 2004.
1044 patients. Hellman, M. S. diabetes,” Patient [27] S. M. M. Hazavehei,
Diabetic Medicine, Kirkman et al., Prefer Adherence, G. Sharifirad, and S.
vol. 26, pp. 939-942, “Comprehensive foot vol. 3, pp. 45-50, Mohabi, “The effect
2009. examination and risk 2009. of educational
[12] R. A. Bell, T. A. assessment,” [22] N. B. Lincoln, K. A. program based on
Arcury, B. M. Diabetes Care, vol. Radford, F. L. Game, health belief model
Snively, R. Dohanis, 31, pp. 1679-1685, and W. J. Jeffcoate, on diabetic foot
and S. A. Quandt, 2008. “Education for care,” International
“Diabetes foot self- [17] Indian Health secondary prevention Journal of Diabetes
care practice in a Service Division of of foot ulcers in in Developing
rural, Triethnic Diabetes Treatment people with diabetes: Countries, vol. 27,
population,” and Prevention, A randomised pp. 18-23, 2007.
Diabetes Educator, “Indian health controlled trial,” [28] N. B. Lincoln, W. J.
vol. 31, pp. 75–83, diabetes best practice Diabetologia, vol. Jeffcoate, P Ince, M.
2005. foot care. Available 51, pp. 1954-1961, Smith, and K. A.
[13] M. V. Johnston, L. at 2008. Radford, “Validation
Pogach Rajan, M., A. http://www.ihs.gov/ [23] G. D. Valk, D. M. W. of a new measure of
Mitchinson, S. L. MedicalPrograms/Di Kriegsman, and W. J. protective footcare
Krein, K. Bonackeret abetes/HomeDocs/T J. Assendelft, behaviour: the
al., “Personal and ools/BestPractices/2 “Patient education Nottingham
treatment factors 009_BP_Foot_Care. for preventing Assessment of
associated with foot pdf., 2009. diabetic foot Functional Footcare
self-care among [18] National Diabetes ulceration,” (NAFF),” Practical
veterans with Education Program Cochrane Database Diabetes
diabetes,” Journal of (NDEP), “Feet can of Systematic International, vol. 4,
Rehabilitation last a lifetime” Reviews, vol. 1, pp. pp. 207-211, 2007.
Research and available at 1–43, 2005. [29] M. E. Khamseh, N.
Development, vol. http://www.ndep.nih. [24] S. Schmidt, H. Vatankhah, and H. R.
43, pp. 227-238, gov/media/Feet_HC Mayer, and E. M. Baradaran,
2006. Guide.pdf, 1998. Panfil, “Diabetes “Knowledge and
[14] L. Makmurini, C. E. [19] J. Heitzman, “Foot foot self-care practice of foot care
Kosasih, and U. care for patients with practices in the in Iranian people
Rahayu, “Upaya diabetes,” Topics in German population,” with type 2
pencegahan primer Geriatric Journal of Clinical diabetes,”
kaki diabetikum di Rehabilitation,” Vol. International Wound
Journal, vol. 4, pp. Diabetes Self- Group Versus
298-302. 2007. Management with Individual Diabetes
[30] D. J. Toobert, S. E. and without Education: A
Hampson, and R. E. automated telephone randomized study,”
Glasgow, “The reinforcement,” Diabetes Care, vol.
summary of diabetes Diabetes Care, vol. 25, pp. 269-274,
self-care activities 31, pp. 408-414, 2002.
measure: Results 2008. [38] C. F. Corbett, “A
from 7 studies and a [36] B. Kulzer, N. randomized pilot
revised scale,” Hermanns, H. study of improving
Diabetes Care, vol. Reinecker, and T. foot care in home
23, pp. 943-950, Haak, “Effects of health patients with
2000. self-management diabetes.” The
[31] Bazian, ltd., training in Type 2 Diabetes Educator,
“Education to diabetes: A vol. 29, pp. 273-282,
prevent foot ulcers in randomized, 2003.
diabetes,” Evidence- prospective trial. [39] D. K. Litzelman, C.
Based Healthcare Diabetic Medicine: A W. Slemenda, C. D.
and Public Health, Journal of the British Langefeld, L. M.
vol. 9, pp. 351-358, Diabetic Association, Hays, M. A. Welch,
2005. vol.24, pp. 415-423, D. E. Bild et al.,
[32] J. A. N. Dorresteijn, 2007. “Reduction of Lower
D. M. W. Kriegsman, Extremity Clinical
and G. D. Valk, Abnormalities in
“Complex Patients with Non-
interventions for Insulin-Dependent
preventing diabetic Diabetes Mellitus.
foot ulceration,” Annals of Internal
Cochran Database of Medicine, vol. 119,
Systematic Reviews, pp. 36-41, 1993.
vol. 1, pp.1-37, [40] S. D. McMurray, G.
2010. Johnson, S. Davis,
[33] D.DeWalt, T. C. and K. McDougall,
Davis, A. S. Wallace, “Diabetes education
H. K. Seligman, B. and care
Bryant-Shilliday, C. management
L. Arnold, et al., significantly improve
“Goal setting in patient outcomes in
diabetes self- the dialysis unit.
management: Taking American Journal of
the baby steps to Kidney Diseases,
success,” Patient vol. 40, pp. 566-575,
Education and 2002.
Counseling, vol. 77, [41] N. Vatankhah, M. E.
pp. 218-223, 2009. Khamseh, Y.
[34] E. G. Eakin, S. P. Noudeh, R. Aghili,
Lawler, C. H. R. Baradaran, and
Vandelanotte and N. S. N. Haeri, “The
Owen, “Telephone effectiveness of foot
Interventions for care education on
Physical Activity and people with type 2
Dietary Behavior diabetes in Tehran,
Change A Systematic Iran. Primary Care
Review, American Diabetes, vol. 3, pp.
Journal of Preventive 73-77, 2009.
Medicine, vol. 32,
pp. 419–434, 2007. [37] P. L. Rickheim, T. W.
[35] K. R. Lorig, P. L. Weaver, J. L. Flader,
Ritter, F. Villa, and J. and D. M. Kendall,
D. Piette, “Spanish “Assessment of
You might also like
- Diabetic Foot Care Behaviors: A Literature Review: Titis Kurniawan, Imas Rafiyah, Ardia Putra, Yanuar PrimandaDocument7 pagesDiabetic Foot Care Behaviors: A Literature Review: Titis Kurniawan, Imas Rafiyah, Ardia Putra, Yanuar PrimandaKKN TEMATIK XI UNISSULANo ratings yet
- Jurnal Diabetic FootDocument7 pagesJurnal Diabetic FootAyu KartikaNo ratings yet
- Diabetic Foot BMJ 2007Document7 pagesDiabetic Foot BMJ 2007edwinnjotoNo ratings yet
- Nurses as educators of diabetic foot patients: Αccepted ArticleDocument4 pagesNurses as educators of diabetic foot patients: Αccepted ArticleKlinik KitamuraNo ratings yet
- International Journal of Nursing StudiesDocument7 pagesInternational Journal of Nursing StudiesAnnisa NoviliaNo ratings yet
- Effectiveness of A Self-Foot-Care Educational Program For Prevention of Diabetic Foot DiseaseDocument11 pagesEffectiveness of A Self-Foot-Care Educational Program For Prevention of Diabetic Foot DiseaseFarhan EmirNo ratings yet
- Diabetic FoodDocument7 pagesDiabetic FoodAstariniHidayahNo ratings yet
- Foot Ankle Spec 2008 Zgonis 46 53Document8 pagesFoot Ankle Spec 2008 Zgonis 46 53pjanu86No ratings yet
- Metode Kualitatif DiabeticDocument8 pagesMetode Kualitatif DiabeticIyanNo ratings yet
- Consensus Development Conference On Diabetic Foot Wound CareDocument7 pagesConsensus Development Conference On Diabetic Foot Wound CarerheyzthNo ratings yet
- Evaluation of Nurses Knowledge Levels of DiabeticDocument13 pagesEvaluation of Nurses Knowledge Levels of DiabeticKlinik KitamuraNo ratings yet
- Jurnal InternationalDocument12 pagesJurnal InternationalJoni RifaniNo ratings yet
- Evidence-based interventions improve diabetic foot careDocument33 pagesEvidence-based interventions improve diabetic foot carerahminurNo ratings yet
- Nursing Vol3 Issue1 Article 4Document9 pagesNursing Vol3 Issue1 Article 4Mark Angelo Picar AbelleraNo ratings yet
- Prevention and Management of Foot Problems in Diabetes: A Summary Guidance For Daily Practice 2015, Based On The IWGDF Guidance DocumentsDocument9 pagesPrevention and Management of Foot Problems in Diabetes: A Summary Guidance For Daily Practice 2015, Based On The IWGDF Guidance DocumentsMatthew PhillipsNo ratings yet
- Diabetic Foot Ulcer Prevention: An Evidence Based PracticeDocument6 pagesDiabetic Foot Ulcer Prevention: An Evidence Based PracticeHarismaPratamaNo ratings yet
- Case Study: Evidence-Based Interventions Enhancing Diabetic Foot Care Behaviors Among Hospitalized DM PatientsDocument17 pagesCase Study: Evidence-Based Interventions Enhancing Diabetic Foot Care Behaviors Among Hospitalized DM PatientsNajib RosyadNo ratings yet
- Foot Self-Care Pada Penyandang Diabetes Mellitus DDocument7 pagesFoot Self-Care Pada Penyandang Diabetes Mellitus DstevanusferdinNo ratings yet
- Practical Guidelines On The Prevention and Management of Diabetic Foot IWGDF 2019Document10 pagesPractical Guidelines On The Prevention and Management of Diabetic Foot IWGDF 2019Maya SariNo ratings yet
- LRDocument22 pagesLRمالك مناصرةNo ratings yet
- Footwear and Foot Care Knowledge As Risk Factors For Foot Problems in Indian DiabeticsDocument5 pagesFootwear and Foot Care Knowledge As Risk Factors For Foot Problems in Indian DiabeticsIqbal TawakalNo ratings yet
- Jurnal BedahDocument17 pagesJurnal Bedahkamah oktaviaNo ratings yet
- Prevention of Foot Ulcer 2020Document22 pagesPrevention of Foot Ulcer 2020Devi SiswaniNo ratings yet
- Journal of Health Science and PreventionDocument5 pagesJournal of Health Science and PreventionKlinik KitamuraNo ratings yet
- Johnson 2006Document6 pagesJohnson 2006GuedesNo ratings yet
- Saurabh 2014Document6 pagesSaurabh 2014Muhammad SawalNo ratings yet
- Cronfa - Swansea University Open Access Repository: Diabetes Research and Clinical PracticeDocument7 pagesCronfa - Swansea University Open Access Repository: Diabetes Research and Clinical PracticeDimasjamalia SafiqriNo ratings yet
- Foot Care For The DiabeticDocument10 pagesFoot Care For The DiabeticlovelyryNo ratings yet
- Diabetic Foot Assessment PDFDocument7 pagesDiabetic Foot Assessment PDFIrma KurniawatiNo ratings yet
- 1 s2.0 S1413355523000217 MainDocument16 pages1 s2.0 S1413355523000217 MainSalvia Elvaretta HarefaNo ratings yet
- Osteomielitis 2020 ArtDocument10 pagesOsteomielitis 2020 ArtAlex Gino Quispe Enriquez100% (1)
- The Effect of Foot Exercise On Diabetic Patients With Foot Ulcer An Evidence Based Case ReportDocument5 pagesThe Effect of Foot Exercise On Diabetic Patients With Foot Ulcer An Evidence Based Case ReportHerald Scholarly Open AccessNo ratings yet
- Effectiveness Combination of Foot Care With Active Range of Motion (ROM) and Plantar Exercise For Reducing Diabetic Foot Ulcer Risk in Diabetes Mellitus Type IIDocument4 pagesEffectiveness Combination of Foot Care With Active Range of Motion (ROM) and Plantar Exercise For Reducing Diabetic Foot Ulcer Risk in Diabetes Mellitus Type IIImron BuhoriNo ratings yet
- Consensus Statements On Osteoporosis Diagnosis, Prevention, and Management in The PhilippinesDocument16 pagesConsensus Statements On Osteoporosis Diagnosis, Prevention, and Management in The PhilippinesMia DangaNo ratings yet
- Joint DO, FX, Safety (Student)Document11 pagesJoint DO, FX, Safety (Student)Lola LeNo ratings yet
- Diabetes and Clinical ResearchDocument7 pagesDiabetes and Clinical ResearchAde PahrunNo ratings yet
- Williams2014Document10 pagesWilliams2014Eugeni Llorca BordesNo ratings yet
- Effect of Foot Exercise and Care On Peripheral Vascular Status in Patients With Diabetes MellitusDocument8 pagesEffect of Foot Exercise and Care On Peripheral Vascular Status in Patients With Diabetes MellitusannyNo ratings yet
- Diabeticfootclassifications ReviewofliteratureDocument8 pagesDiabeticfootclassifications ReviewofliteratureAlma Abigail PamartaNo ratings yet
- Cis 460Document6 pagesCis 460restiNo ratings yet
- Haghverdian Et Al 2023 Clinical Pathway For The Management of Diabetic Foot Infections in The Emergency DepartmentDocument5 pagesHaghverdian Et Al 2023 Clinical Pathway For The Management of Diabetic Foot Infections in The Emergency DepartmentINICUOMNo ratings yet
- --Low-Level Laser Therapy at 635 nm for Treatment of Chronic Plantar Fasciitis. A Placebo-Controlled, Randomized StudyDocument5 pages--Low-Level Laser Therapy at 635 nm for Treatment of Chronic Plantar Fasciitis. A Placebo-Controlled, Randomized StudymarioNo ratings yet
- A Study To Assess The Effectiveness of Planned Teaching Programme On Knowledge of Foot Care Among Diabetic Patients at Selected Community Health Center in Bhopal M.P.Document7 pagesA Study To Assess The Effectiveness of Planned Teaching Programme On Knowledge of Foot Care Among Diabetic Patients at Selected Community Health Center in Bhopal M.P.Editor IJTSRDNo ratings yet
- Lifengetal FeasibilityAcceptabilityandEffectsofaFootSelf-CareEducationalIntervention2013Document9 pagesLifengetal FeasibilityAcceptabilityandEffectsofaFootSelf-CareEducationalIntervention2013Marcela RodriguezNo ratings yet
- Diabetic Neuropathy Doc 2Document5 pagesDiabetic Neuropathy Doc 2ikhlaslivingNo ratings yet
- Activity Modification and Knee Strengthening For Osgood-Schlatter DiseaseDocument9 pagesActivity Modification and Knee Strengthening For Osgood-Schlatter DiseaseSebastian FandiñoNo ratings yet
- Knee PTDocument12 pagesKnee PTMahtab AhmadiNo ratings yet
- 1 s2.0 S0976566220305774 MainDocument14 pages1 s2.0 S0976566220305774 Mainblok etikakedokteranNo ratings yet
- Prevention of Diabetic Foot Ulcers The Bottlenecks in The PathwayDocument3 pagesPrevention of Diabetic Foot Ulcers The Bottlenecks in The PathwayreuniNo ratings yet
- 044 - 3619 - I Wayan Subawa - GalleyDocument7 pages044 - 3619 - I Wayan Subawa - GalleyrashbahatNo ratings yet
- Internasional 1Document5 pagesInternasional 1Lili ApriliaNo ratings yet
- Identifikasi Risiko Diabetic Foot Ulcer (Dfu) Pada Pasien Dengan Diabetes MellitusDocument6 pagesIdentifikasi Risiko Diabetic Foot Ulcer (Dfu) Pada Pasien Dengan Diabetes Mellituselsa aureliaNo ratings yet
- Diabetes Metabolism Res - 2023 - Lepesis - Systematic Review and Meta Analysis of The Effects of Foot and Ankle PhysicalDocument14 pagesDiabetes Metabolism Res - 2023 - Lepesis - Systematic Review and Meta Analysis of The Effects of Foot and Ankle Physicalnindi jemmyNo ratings yet
- 28 1561634191Document5 pages28 1561634191Trần Duy TânNo ratings yet
- IWGDF Guidelines 2019 PDFDocument194 pagesIWGDF Guidelines 2019 PDFMara100% (2)
- Literature Review: Foot Exercise Prevents The Risk of Neuropathy On Diabetes Mellitus PatientDocument8 pagesLiterature Review: Foot Exercise Prevents The Risk of Neuropathy On Diabetes Mellitus PatientEva Cica SusantiNo ratings yet
- Management of Diabetes FootDocument41 pagesManagement of Diabetes FootsangheetaNo ratings yet
- Prevention and Treatment of Diabetic Foot Ulcers. Journal of The Royal Society of Medicine. 2017. Vol 110Document6 pagesPrevention and Treatment of Diabetic Foot Ulcers. Journal of The Royal Society of Medicine. 2017. Vol 110Jose Fernando DiezNo ratings yet
- 239 1078 4 PBDocument5 pages239 1078 4 PBEmiel AwadNo ratings yet
- Efn GroupDocument1 pageEfn Groupnadya wahyuNo ratings yet
- The Digestive System Part 1Document9 pagesThe Digestive System Part 1nadya wahyu100% (1)
- Breathing Problems (Difficult Words)Document2 pagesBreathing Problems (Difficult Words)nadya wahyuNo ratings yet
- A TranslateDocument1 pageA Translatenadya wahyuNo ratings yet
- Nursing CommunicationDocument5 pagesNursing Communicationnadya wahyuNo ratings yet
- Topic PainDocument3 pagesTopic Painnadya wahyuNo ratings yet
- Mrs Bell's Sleep DifficultiesDocument4 pagesMrs Bell's Sleep Difficultiesnadya wahyuNo ratings yet
- Digestive SystemDocument17 pagesDigestive Systemnadya wahyuNo ratings yet
- Group 5 Elimination ProblemsDocument3 pagesGroup 5 Elimination Problemsnadya wahyuNo ratings yet
- Safety and Preventing Accident: Providing General Giving Information Offering Self Giving InformationDocument3 pagesSafety and Preventing Accident: Providing General Giving Information Offering Self Giving Informationnadya wahyuNo ratings yet
- Wheel Chair Makes People Lazy and Not Trying Can Not Be Independent The Price of Cane Is Also Relatively Cheaper Than The Wheel ChairDocument1 pageWheel Chair Makes People Lazy and Not Trying Can Not Be Independent The Price of Cane Is Also Relatively Cheaper Than The Wheel Chairnadya wahyuNo ratings yet
- Link ScribdDocument1 pageLink Scribdnadya wahyuNo ratings yet
- Group 1 Group 2 Group 3Document2 pagesGroup 1 Group 2 Group 3nadya wahyuNo ratings yet
- Wheel Chair Makes People Lazy and Not Trying Can Not Be Independent The Price of Cane Is Also Relatively Cheaper Than The Wheel ChairDocument1 pageWheel Chair Makes People Lazy and Not Trying Can Not Be Independent The Price of Cane Is Also Relatively Cheaper Than The Wheel Chairnadya wahyuNo ratings yet
- Contra Fast FoodDocument1 pageContra Fast Foodnadya wahyuNo ratings yet
- A TranslateDocument1 pageA Translatenadya wahyuNo ratings yet
- A TranslateDocument1 pageA Translatenadya wahyuNo ratings yet
- Vocabulary UasDocument6 pagesVocabulary Uasnadya wahyuNo ratings yet
- Wheel Chair Makes People Lazy and Not Trying Can Not Be Independent The Price of Cane Is Also Relatively Cheaper Than The Wheel ChairDocument1 pageWheel Chair Makes People Lazy and Not Trying Can Not Be Independent The Price of Cane Is Also Relatively Cheaper Than The Wheel Chairnadya wahyuNo ratings yet
- Contra Fast FoodDocument1 pageContra Fast Foodnadya wahyuNo ratings yet
- Mencari "VOCABULARY" Yang Sulit Dan Di "TERJEMAHKAN" 2. Menentukan Kalimat "THERAPEUTIC COMMUNICATION TECHNIQUES"Document1 pageMencari "VOCABULARY" Yang Sulit Dan Di "TERJEMAHKAN" 2. Menentukan Kalimat "THERAPEUTIC COMMUNICATION TECHNIQUES"nadya wahyuNo ratings yet
- Mencari "VOCABULARY" Yang Sulit Dan Di "TERJEMAHKAN" 2. Menentukan Kalimat "THERAPEUTIC COMMUNICATION TECHNIQUES"Document1 pageMencari "VOCABULARY" Yang Sulit Dan Di "TERJEMAHKAN" 2. Menentukan Kalimat "THERAPEUTIC COMMUNICATION TECHNIQUES"nadya wahyuNo ratings yet
- Group 5 - Taking Patient Identity, Background, and Health HistoryDocument2 pagesGroup 5 - Taking Patient Identity, Background, and Health Historynadya wahyuNo ratings yet
- Mencari "VOCABULARY" Yang Sulit Dan Di "TERJEMAHKAN" 2. Menentukan Kalimat "THERAPEUTIC COMMUNICATION TECHNIQUES"Document1 pageMencari "VOCABULARY" Yang Sulit Dan Di "TERJEMAHKAN" 2. Menentukan Kalimat "THERAPEUTIC COMMUNICATION TECHNIQUES"nadya wahyuNo ratings yet
- Group 4 - Taking Patient Identity, Background, and Health HistoryDocument2 pagesGroup 4 - Taking Patient Identity, Background, and Health Historynadya wahyuNo ratings yet
- Group 5 - Taking Patient Identity, Background, and Health HistoryDocument2 pagesGroup 5 - Taking Patient Identity, Background, and Health Historynadya wahyuNo ratings yet
- Link ScribdDocument1 pageLink Scribdnadya wahyuNo ratings yet
- Group 5 - Taking Patient Identity, Background, and Health HistoryDocument2 pagesGroup 5 - Taking Patient Identity, Background, and Health Historynadya wahyuNo ratings yet
- Group 4 - Taking Patient Identity, Background, and Health HistoryDocument2 pagesGroup 4 - Taking Patient Identity, Background, and Health Historynadya wahyuNo ratings yet
- Skin Infection Lab ReportDocument6 pagesSkin Infection Lab Reportthe someone100% (2)
- Psik Soal UtsDocument1 pagePsik Soal UtsNaurahSalsabil / 20No ratings yet
- NCM 103 Aliasas AtelectasisDocument3 pagesNCM 103 Aliasas AtelectasisDARREN EDMARKNo ratings yet
- PESCI Recalls PDFDocument9 pagesPESCI Recalls PDFDanishNo ratings yet
- Challenges Providing Palliative Care Cancer Patients PalestineDocument35 pagesChallenges Providing Palliative Care Cancer Patients PalestineHammoda Abu-odah100% (1)
- Business Plan Analysis - 08 1: SFHN/SJ&G Oxalepsy (Oxcarbazipine300 & 600 MG)Document63 pagesBusiness Plan Analysis - 08 1: SFHN/SJ&G Oxalepsy (Oxcarbazipine300 & 600 MG)Muhammad SalmanNo ratings yet
- Playing With PerformanceDocument10 pagesPlaying With PerformancemarisaNo ratings yet
- Prescribing Information: 1. Name of The Medicinal ProductDocument5 pagesPrescribing Information: 1. Name of The Medicinal Productddandan_20% (1)
- Atrial Fibrillation - Diagnosis and Treatment - AAFP PDFDocument8 pagesAtrial Fibrillation - Diagnosis and Treatment - AAFP PDFNaufal AmanullahNo ratings yet
- Immediate Dental Implant Placement Into Infected vs. Non-Infected Sockets: A Meta-AnalysisDocument7 pagesImmediate Dental Implant Placement Into Infected vs. Non-Infected Sockets: A Meta-Analysismarlene tamayoNo ratings yet
- Nursing Documentation for Wina Purnamasari's Immunization and Vital Signs CheckDocument6 pagesNursing Documentation for Wina Purnamasari's Immunization and Vital Signs Checkilah keciNo ratings yet
- Green White Minimalist Modern Real Estate PresentationDocument8 pagesGreen White Minimalist Modern Real Estate Presentationapi-639518867No ratings yet
- Research EssayDocument12 pagesResearch Essayapi-608972617No ratings yet
- Surgical Site InfectionDocument7 pagesSurgical Site InfectionCaxton ThumbiNo ratings yet
- Organization of NICU ServicesDocument45 pagesOrganization of NICU ServicesMonika Bagchi84% (64)
- Rheumatological History Taking OSCE GuideDocument11 pagesRheumatological History Taking OSCE GuideChen BrionesNo ratings yet
- Manage Ophthalmia NeonatorumDocument2 pagesManage Ophthalmia NeonatorumEjay BautistaNo ratings yet
- NEET UG Biology Human Health and DiseasesDocument18 pagesNEET UG Biology Human Health and DiseasesMansoor MalikNo ratings yet
- Miliaria Pustulosa (Infetrop)Document11 pagesMiliaria Pustulosa (Infetrop)Muhammad mukramNo ratings yet
- Qip ProjectDocument13 pagesQip Projectapi-534216481No ratings yet
- Repositioning an Inverted UterusDocument5 pagesRepositioning an Inverted Uterusshraddha vermaNo ratings yet
- Comparative Efficacy of Non-Sedating Antihistamine Updosing in Patients With Chronic UrticariaDocument6 pagesComparative Efficacy of Non-Sedating Antihistamine Updosing in Patients With Chronic UrticariadregleavNo ratings yet
- Endocrine System: Capillary Glucose MonitoringDocument34 pagesEndocrine System: Capillary Glucose Monitoringjoel david knda mj100% (1)
- The Truth About The Flu ShotDocument5 pagesThe Truth About The Flu ShotPoorMexicanNo ratings yet
- Aesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Document60 pagesAesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Drhisham AttiaNo ratings yet
- 2018 Conference AbstractsDocument155 pages2018 Conference AbstractsBanin AbadiNo ratings yet
- Medical Design BriefsDocument62 pagesMedical Design Briefsneto512No ratings yet
- Sample Birthing PlanDocument2 pagesSample Birthing PlanChuohNo ratings yet
- Gender-Dysphoric-Incongruene Persons, Guidelines JCEM 2017Document35 pagesGender-Dysphoric-Incongruene Persons, Guidelines JCEM 2017Manel EMNo ratings yet
- The Medical Power of LightDocument2 pagesThe Medical Power of LightMichele CarvalhoNo ratings yet