Professional Documents
Culture Documents
ARDS Management Protocol: February 2018
Uploaded by
soulstakersOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ARDS Management Protocol: February 2018
Uploaded by
soulstakersCopyright:
Available Formats
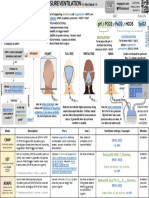
ARDS Management Protocol
February 2018
ARDS Criteria
Onset Within 1 week of a known clinical insult or new or worsening respiratory symptoms
Bilateral opacities—not fully explained by effusions, lobar/lung collapse, or nodules
Respiratory failure not fully explained by cardiac failure or fluid overload Need objective
assessment (eg, echocardiography) to exclude hydrostatic edema if no risk factor present
PaO2/FIO2 ≤ 300 mm Hg with PEEP or CPAP ≥ 5 cm H2O
Severity of Illness
Mid: 200 mm Hg < PaO2/FIO2 ≤ 300 mm Hg with PEEP or CPAP ≥ 5 cm H2O
Moderate: 100 mm Hg < PaO2/FIO2 ≤ 200 mm Hg with PEEP ≥ 5 cm H2O
Severe: PaO2/FIO2 ≤ 100 mm Hg with PEEP ≥ 5 cm H2O
Calculations
Calculate Ideal Body Weight (IBW):
Men = 50 + [(height (cm) -154) x 0.9]
Women = 45.5 + [(height (cm) -154) x 0.9]
Desired minute ventilation (MV)= IBW * 125
A Set Targets
Tidal volume 4-6 ml/kg of IBW
Plateau pressure: <30 cm H2O (preferably <28 cm H2O), may accept higher plateau If patient
has stiff chest wall or abdominal limitation (e.g., with massive ascites, large pleural effusion or
obese patients)
Driving pressure < 15 cm H2O
pH: 7.25-7.45
PaO2 55-80 mmHg or SpO2 88-95% and FiO2 ≤ 60%
1 Volume Control Mode
Pressure Regulation Mode (PRVC, CMV with autoflow, AC+, or APVcmv)
Set volume at 6 mL/kg of IBW
Decrease volume at 1 mL/kg to achieve the set plateau pressure goal
Set pressure alarm limit 37-50 cm H2O (dependent on the type of ventilator)
Set rate at desired minute ventilation/VT: The respiratory rate will be set to avoid air trapping
whenever possible as determined by the inspection of the flow tracing and/or measurements
of intrinsic PEEP.
Adjust rate for the pH goal
1 Pressure Control Mode
Set pressure control less than 30
Adjust pressure to maintain VT 4-6 mL/kg of IBW
Set rate at desired minute ventilation/VT: The respiratory rate will be set to avoid air trapping
whenever possible as determined by the inspection of the flow tracing and/or measurements
of intrinsic PEEP.
1 PEEP Titration: Low PEEP/FiO2 Table
FiO2% 30 40 40 50 50 60 70 70 70 80 90 90 90 100
PEEP (cm H2O) 5 5 8 8 10 10 10 12 14 14 14 16 18 18-24
2 PEEP Titration: High PEEP/FiO2 Table
50- 100
FiO2% 30 30 30 30 30 30 40 40 50 50 80 90 100
80
PEEP (cm 5 8 10 12 14 14 16 16 18 20 14 22 22 22 24
H2O)
3 Paralysis
Use within the first 48 hours
Severe ARDS with PEEP/FiO2 <150
Intravenous injection of 20 mg of cisatracurium (may repeat if a decrease of the end-
inspiratory plateau pressure by less than 2 cm of water was noticed)
May use continuous infusion for paralysis
Ensure adequate sedation with RASS -4 to -5
3 Recruitment Maneuver
Moderate or severe ARDS
Continuous positive airway pressure (CPAP) mode and increase the pressure to 30–40 cmH2O
for 30–40 s
Monitor hemodynamics and possibility of pneumothorax
Caution in patients with preexisting hypovolemia or shock
4 Esophageal Pressure Monitoring
Moderate to severe ARDS or conditions with increase thoracic or intraabdominal pressures,
(i.e obesity)
B Transpulmonary Pressure Targets
Transpulmonary pressure in inspiration (Insp PL) <30
Transpulmonary pressure in expiration (Exp PL): 0-10
Transpulmonary driving pressure (True Driving Pressure: DPtp) <15
C Contraindication to prone position
Increased ICP
Massive hemoptysis
Tracheal surgery or sternotomy <2 weeks
Facial trauma or surgery < 2 weeks including neck trauma or spinal instability
Pregnancy
DVT treated < 2days
large ventral surface burn
Cardiac pacemaker inserted < 2days
Unstable spine, pelvic, or femur fracture
Morbid obesity
Patients at high risk of requiring CPR or defibrillation
Staff judgement
5 Trial of prone position
Who to place in prone position?
• Patients with severe ARDS (PaO2/FiO2 < 150 mm Hg)
• Early in the course (ideally within 48 h)
• Best outcomes reported when prone positioning is used in combination with both
low tidal volume ventilation (6 cc/kg) and neuromuscular blockade
How to place patient in prone position?
• Requires 3-5 people, close attention to endotracheal tube (ETT) and central lines
• Preparation: preoxygenation, empty stomach, suction ETT/oral cavity, remove ECG
leads and reattach to back, repeated zeroing of hemodynamic transducers
• Support and frequently reposition pressure points: face, shoulder, anterior pelvis
How long to have patient in prone position each day?
• Successful trials use at least 16 hours of daily proning
• Long prone positioning sessions likely avoid derecruitment
When to stop?
• In PROSEVA, prone positioning was stopped when PaO2/FiO2 remained > 150 mm Hg
4 h after supinating (with PEEP < 10 cm H2O and FiO2 < 0.6)
• Optimal strategy is unclear: consider continuing prone positioning until clear
improvement in gas exchange, mechanics, and overall clinical course.
Potential complications
• Temporary increase in oral and tracheal secretions occluding airway
• ETT migration or kinking
• Vascular catheter kinking
• Elevated intraabdominal pressure
• Increased gastric residuals
• Facial pressure ulcers, facial edema, lip trauma from ETT, brachial plexus injury (arm
extension)
D ECMO Eligibility
Severe hypoxemia (PaO2/FiO2 ratio <80 mmHg) despite conventional and appropriate
therapies for at least 6 hours in acute reversible lung disease
Uncompensated hypercapnia with acedemia (pH <7.15) despite best accepted standard of
ventilatory care.
Presence of excessively high end-inspiratory plateau pressures (>35 cm H2O) despite best
accepted standard of ventilatory care.
No terminal disease (expected survival >6 months)
Intact neurological status
No limited vascular access
Respiratory support < 7 days (relative)
6 ECMO
http://www.nejm.org/doi/full/10.1056/NEJMct1103720
8 APRV
High airway pressure (Phigh) at the Pplat measured at the previous VCV settings +5 (not to
exceed 30 cmH2O)
Low airway pressure (Plow) at 5 cmH2O (minimal pressure level was used to prevent
atelectasis per standard practice)
Duration of release phase (Tlow) at one- to 1.5-fold the expiratory time constant, and then
adjust to achieve a termination of peak expiratory flow rate (PEFR) of ≥50% of PEFR
Release frequency at 10–14 frequency/min
Duration of Phigh (Thigh) is indirectly calculated based on the Tlow and release frequency
Spontaneous respiratory level targeted as spontaneous minute ventilation (MVspont),
approximately 30% total minute ventilation (MVtotal)
8 HFV
Bias flow 40 L/min
Inspiratory time 33%
mPaw 30 cm H2O
FIO2 1.0
Amplitude (delta P) 90 cm H2O.
Initial frequency based on most recent arterial blood gas:
• pH <7.10 = 4 Hz
• pH 7.10–7.19 = 5 Hz
• pH 7.20–7.35 = 6 Hz
• pH >7.35 = 7 Hz
8 Vasodilators: epoprostenol (aEPO)
Initiate aEPO at 50 ng/kg/min (based on ideal body weight – IBW, rounded to nearest 10kg)
via continuous nebulization with nebulizer connected to the ventilator
aEPO should be titrated downward every 30 minutes as tolerated to 10 ng/kg/min based on
PaO2 improvement.
Do NOT decrease aEPO by more than 10 ng/kg/min every 30 minutes
https://www.universityhealthsystem.com/~/media/files/clinical-pathways/inhaled-
epoprostenol-guideline-1114.pdf?la=en
8 Tracheal Gas Insufflation (TGI)
https://www.atsjournals.org/doi/pdf/10.1164/ajrccm.162.2.9910111
ARDS Criteria
Met
VT 4-6 mL/kg
PPL <30 Mode: PRVC or PC
A 1
Driving Pressure <15 PEEP: Low PEEP/FiO2 Table
SPO2 >88% on FiO2
<60% Maintain
√A
Yes
No
PEEP Titration
2
High PEEP/FiO2 Table
APRV Maintain
HFV √A
Bilevels Yes
8
Nitric Oxide No
TGI Alprostadil
Paralysis
3
Recruitment maneuver
Maintain
√A
6 ECMO Yes
No
Yes
No Transesophageal Pressure
4
Monitoring
ECMO Insp PL <30
D Exp PL 0-10
Eligible B √A
Yes DPtp <15
No No
No
Trial of Prone Yes Prone
Maintain 5 C
Yes Ventilation Eligible
√A
You might also like
- Respiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsFrom EverandRespiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsJian-Xin ZhouNo ratings yet
- ArdsDocument2 pagesArdsKakaa KakaNo ratings yet
- Mechanical VentilationDocument52 pagesMechanical VentilationShaliniNo ratings yet
- Ventilator For DummiesDocument19 pagesVentilator For DummiesGeorge MaspiNo ratings yet
- Formula For Calculation of Hemodynamics in Cardiac Catheterization-Ver.1.1Document3 pagesFormula For Calculation of Hemodynamics in Cardiac Catheterization-Ver.1.1Sam YenNo ratings yet
- Troubleshooting Problem SolvingDocument22 pagesTroubleshooting Problem Solvingnaravichandran3662No ratings yet
- Point of View Heparin ResistanceDocument20 pagesPoint of View Heparin ResistanceSameer Goyal100% (1)
- 12 LeadDocument7 pages12 Leadjerry3gowenNo ratings yet
- Agustus Monitoring HemodinamikDocument61 pagesAgustus Monitoring HemodinamikFikriYTNo ratings yet
- Pulse Contour Cardiac Output Learning Package PDFDocument17 pagesPulse Contour Cardiac Output Learning Package PDFNurse PractitionerNo ratings yet
- Fluids and Electrolyte PediatricsDocument41 pagesFluids and Electrolyte PediatricsYusron BishryNo ratings yet
- 406 - Respiratory Therapy Consult Service HandbookDocument28 pages406 - Respiratory Therapy Consult Service HandbookIkhsan JohnsonNo ratings yet
- Respiratory Care Standard Abbreviations and SymbolsDocument6 pagesRespiratory Care Standard Abbreviations and SymbolsHussein FatalNo ratings yet
- Optiflow Presentation-Carly TorgersenDocument12 pagesOptiflow Presentation-Carly Torgersenapi-252628311100% (1)
- AA GradientDocument2 pagesAA GradientzaminazzNo ratings yet
- Best Practice in ShockDocument30 pagesBest Practice in ShockFoungZanz D. LuffyzNo ratings yet
- Non-Invasive Ventilation NIV: Yazeed Abed El Khaleq Respiratory St4 BNHHDocument24 pagesNon-Invasive Ventilation NIV: Yazeed Abed El Khaleq Respiratory St4 BNHHYazeedNo ratings yet
- Normal Pediatric RR and HRDocument1 pageNormal Pediatric RR and HRRick FreaNo ratings yet
- Advanced Airway Management 4th YearsDocument39 pagesAdvanced Airway Management 4th YearsAmmaarah Isaacs100% (1)
- ABG Flow ChartDocument1 pageABG Flow ChartcpradheepNo ratings yet
- Role of New 3rd Generation of Beta-Blocker in The ... Dr. Elfiani, SPPD., FINASIMDocument55 pagesRole of New 3rd Generation of Beta-Blocker in The ... Dr. Elfiani, SPPD., FINASIMZikri HakimNo ratings yet
- ICU One Pager NIPPVDocument1 pageICU One Pager NIPPVNicholas HelmstetterNo ratings yet
- HFOV High-Frequency-Oscillatory-VentilationDocument22 pagesHFOV High-Frequency-Oscillatory-VentilationJZNo ratings yet
- COVERAM BP Decrease, Central Aortic and SynergyDocument34 pagesCOVERAM BP Decrease, Central Aortic and Synergyputridewi22100% (1)
- Regional AnesthesiaDocument54 pagesRegional AnesthesiaIdza Fariha AfriNo ratings yet
- Flight For Life 81M.01 Mechanical Ventilation 2022-07-01Document4 pagesFlight For Life 81M.01 Mechanical Ventilation 2022-07-01Bryan WinchellNo ratings yet
- Nippv Revisi Final Picu Nicu MaretDocument51 pagesNippv Revisi Final Picu Nicu MaretJulian Ammar Zaidan GunawanNo ratings yet
- ABG Interpretation ActivityDocument16 pagesABG Interpretation ActivityArlly Faena AbadNo ratings yet
- HW InotropesDocument3 pagesHW InotropesNatalie YeohNo ratings yet
- Acid Base Disorders - Lecture 45Document14 pagesAcid Base Disorders - Lecture 45yassin mostafaNo ratings yet
- Pediatric Anesthesia For StudentsDocument4 pagesPediatric Anesthesia For StudentsMarco TolentinoNo ratings yet
- Yale IIP MICU120-160 2011Document2 pagesYale IIP MICU120-160 2011afm26No ratings yet
- Dosage CardDocument2 pagesDosage CardKleibert Maciel100% (1)
- A Powerful Tool To Objectively Monitor Your Patients Ventilatory StatusDocument36 pagesA Powerful Tool To Objectively Monitor Your Patients Ventilatory StatusBeth Strom-Sturm100% (1)
- AclsDocument21 pagesAclsMelvin Sierra TejedaNo ratings yet
- 3 Step ABG Interpretation - 2Document1 page3 Step ABG Interpretation - 2Sibel ErtuğrulNo ratings yet
- ACLS Algorithms Adult 2010 Revised May 31 2011Document12 pagesACLS Algorithms Adult 2010 Revised May 31 2011arturschander3614No ratings yet
- Noninvasive Ventilation in Acute Respiratory Failure in AdultsDocument12 pagesNoninvasive Ventilation in Acute Respiratory Failure in AdultsferrevNo ratings yet
- Review of HD Monitoring: DR Ghaleb Almekhlafi MD, SFCCM, EdicDocument105 pagesReview of HD Monitoring: DR Ghaleb Almekhlafi MD, SFCCM, EdicGHALEB A. Almekhlafi100% (1)
- Arrhythmia 2Document31 pagesArrhythmia 2rittvedNo ratings yet
- Coveram Symcard DR Yerizal PDFDocument47 pagesCoveram Symcard DR Yerizal PDFRahmat MuliaNo ratings yet
- Sodium Bicarbonate - I2 V1Document1 pageSodium Bicarbonate - I2 V1Hazel CustodioNo ratings yet
- 04.06.2018 - 6 - V. Kushakovsky - Pediatric AnaesthesiaDocument46 pages04.06.2018 - 6 - V. Kushakovsky - Pediatric AnaesthesiaPhilippe KinnaerNo ratings yet
- Weaning Failure in Critical IllnessDocument8 pagesWeaning Failure in Critical IllnessNadia Setianingsih100% (1)
- King Airway: Norcal Ems Training ModuleDocument13 pagesKing Airway: Norcal Ems Training Moduleandrew22No ratings yet
- Prehospital MedicationsDocument123 pagesPrehospital Medicationshilwaalfi100% (1)
- Heparin: AnticoagulantsDocument8 pagesHeparin: AnticoagulantsThierd Cañete III100% (1)
- TachycardiaDocument12 pagesTachycardiaPuskesmas Pinang JayaNo ratings yet
- AlbuminDocument14 pagesAlbuminMaria Chona Penillos HularNo ratings yet
- Certofix BrochureDocument20 pagesCertofix BrochureAyu Indah CarolinaNo ratings yet
- Riding The WavesDocument76 pagesRiding The WavesMedic03431No ratings yet
- Materi - STBI Cedera Kepala Di ICU-JIH 2022 DR SetyoriniDocument40 pagesMateri - STBI Cedera Kepala Di ICU-JIH 2022 DR SetyoriniDudhutt TVNo ratings yet
- Inhaled Nitric OxideDocument24 pagesInhaled Nitric OxidesajaNo ratings yet
- Perioperative Fluid Management in Pediatrics: By: Karim Kamal, MDDocument33 pagesPerioperative Fluid Management in Pediatrics: By: Karim Kamal, MDMohammed AKNo ratings yet
- Amoul nCPAP Series: Ambulanc (Shenzhen) Tech. Co., LTDDocument4 pagesAmoul nCPAP Series: Ambulanc (Shenzhen) Tech. Co., LTDGetaneh GetachewNo ratings yet
- CAB ManagementDocument21 pagesCAB ManagementTery'sNo ratings yet
- Protocolo LOVDocument6 pagesProtocolo LOVV ANo ratings yet
- Managing A Mechanically Ventilated PatientDocument51 pagesManaging A Mechanically Ventilated PatientPeony03No ratings yet
- Weaning From Mechanical VentilationDocument45 pagesWeaning From Mechanical VentilationmartinNo ratings yet
- ABG MCQsDocument6 pagesABG MCQssoulstakersNo ratings yet
- Abdominal Paracentesis PDFDocument2 pagesAbdominal Paracentesis PDFsoulstakersNo ratings yet
- ABCDEF Bundle WebcastDocument42 pagesABCDEF Bundle WebcastsoulstakersNo ratings yet
- 2nd Annual Critical Care Review Course 2018 PDFDocument7 pages2nd Annual Critical Care Review Course 2018 PDFsoulstakersNo ratings yet
- Toxocology: Abdullah Alolayan, R4Document6 pagesToxocology: Abdullah Alolayan, R4soulstakersNo ratings yet
- Enteral NutritionDocument11 pagesEnteral NutritionEso Soso0% (1)
- Case Report FinalDocument21 pagesCase Report FinalAyen FornollesNo ratings yet
- IndianJPain3341-1062069 025700Document10 pagesIndianJPain3341-1062069 025700docbinNo ratings yet
- 4R's of RadiobiologyDocument32 pages4R's of Radiobiologyarif081190No ratings yet
- Bladder Calculus Resulting From The Migration of An IntrauterineDocument8 pagesBladder Calculus Resulting From The Migration of An IntrauterineFabrien Hein WillemNo ratings yet
- Topical AntifungalsDocument14 pagesTopical AntifungalsRasha Mohammad100% (1)
- Contribuciones de Shneidman Al Pensamiento SuicidaDocument21 pagesContribuciones de Shneidman Al Pensamiento SuicidaJuan Carlos Jaramillo100% (1)
- Non Surgical Therapy For Anal Fissure (Review) - Cochrane LibraryDocument118 pagesNon Surgical Therapy For Anal Fissure (Review) - Cochrane LibraryNicolás CopaniNo ratings yet
- Clinical Tools For The Assessment of Pain in Sedated Critically Ill AdultsDocument10 pagesClinical Tools For The Assessment of Pain in Sedated Critically Ill AdultsEviNo ratings yet
- Bradycardia 1Document6 pagesBradycardia 1harasthaNo ratings yet
- Oxygen Therapy: Patient EducationDocument2 pagesOxygen Therapy: Patient EducationendaNo ratings yet
- Morton's NeuromaDocument8 pagesMorton's Neuromagreencrystal81No ratings yet
- Resume MedisDocument6 pagesResume MedisRina ekaNo ratings yet
- Wart Removal and TreatmentDocument6 pagesWart Removal and TreatmentwandaNo ratings yet
- Health Benefits of HoneyDocument10 pagesHealth Benefits of HoneyMohd Idris MohiuddinNo ratings yet
- Water Quality at Residential and Industrial AreaDocument11 pagesWater Quality at Residential and Industrial AreaMohamad AizanNo ratings yet
- Santos, Ivan Jamil S. NCM 112-Or Rle Fear (Pre-Op) Assessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveDocument1 pageSantos, Ivan Jamil S. NCM 112-Or Rle Fear (Pre-Op) Assessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveIvan SantosNo ratings yet
- Tests That Will Elicit Cerebellar Signs Are inDocument4 pagesTests That Will Elicit Cerebellar Signs Are inRaina DeWyzeNo ratings yet
- Patient Blood Management Equals Patient SafetyDocument19 pagesPatient Blood Management Equals Patient SafetyMuhammadBudiman RbcNo ratings yet
- Dre & Anoscopy: A Self-Directed Learning Module Clinical Skills Program Queen's UniversityDocument10 pagesDre & Anoscopy: A Self-Directed Learning Module Clinical Skills Program Queen's UniversitymNo ratings yet
- West Bengal's Leather Industry OpportunitiesDocument5 pagesWest Bengal's Leather Industry OpportunitiesDeepak AgarwalNo ratings yet
- Ethical Issues Clinical PsychologyDocument24 pagesEthical Issues Clinical PsychologyRose annNo ratings yet
- A 3 Table of Surgical Procedures TOSP With Minor Surgical Procedures MSPs 1Document94 pagesA 3 Table of Surgical Procedures TOSP With Minor Surgical Procedures MSPs 1Chee Yung NgNo ratings yet
- DR Pugud - Correlation Between CHD and DiabetesDocument47 pagesDR Pugud - Correlation Between CHD and DiabetesKrishnaNo ratings yet
- PDF PDFDocument13 pagesPDF PDFadrianofaustinoNo ratings yet
- Sepsis Early Goal Directed Therapy (EGDT) Algorithm/Driver DiagramDocument1 pageSepsis Early Goal Directed Therapy (EGDT) Algorithm/Driver DiagramAngga AndriyantoNo ratings yet
- Art Therapy APADocument10 pagesArt Therapy APAhashmiaqeedat5No ratings yet
- PDF Fillable Medical CertDocument4 pagesPDF Fillable Medical CertCasey PetersonNo ratings yet
- Anestesi Obat ObatanDocument72 pagesAnestesi Obat ObatanfujiNo ratings yet
- Management of Failed Block - Harsh.Document48 pagesManagement of Failed Block - Harsh.Faeiz KhanNo ratings yet