Professional Documents
Culture Documents
The Nephritic Syndrome.3
Uploaded by
emi_bgt0 ratings0% found this document useful (0 votes)
72 views19 pagesA 21 year-old woman presents with tea-colored urine three weeks after a sore throat. Urine dipstick demonstrates 2+ protein, large heme and large leukocyte esterase. A reading of 4+ protein by dipstick does not guarantee the presence of nephrotic-range proteinuria.
Original Description:
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentA 21 year-old woman presents with tea-colored urine three weeks after a sore throat. Urine dipstick demonstrates 2+ protein, large heme and large leukocyte esterase. A reading of 4+ protein by dipstick does not guarantee the presence of nephrotic-range proteinuria.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
72 views19 pagesThe Nephritic Syndrome.3
Uploaded by
emi_bgtA 21 year-old woman presents with tea-colored urine three weeks after a sore throat. Urine dipstick demonstrates 2+ protein, large heme and large leukocyte esterase. A reading of 4+ protein by dipstick does not guarantee the presence of nephrotic-range proteinuria.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 19
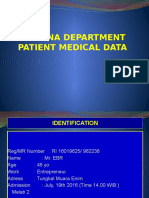
THE NEPHRITIC SYNDROME
by Geoffrey K. Dube and Robert S. Brown
A 21 year-old woman presents with tea-colored urine
three weeks after being evaluated for a sore throat.
Physical examination is notable for a blood pressure
of 170/100 and 3+ pitting edema. Serum creatinine
is 2.1 mg/dl. Urine dipstick demonstrates 2+ protein,
large heme and large leukocyte esterase.
© 2004, Beth Israel Deaconess Medical Center, Inc.
A 21 year-old woman presents with tea-colored urine three weeks after
being evaluated for a sore throat. Physical examination is notable for a
blood pressure of 170/100 and 3+ pitting edema. Serum creatinine is 2.1
mg/dl. Urine dipstick demonstrates 2+ protein, large heme and large
leukocyte esterase.
Based on the results of the urine dipstick, which of
the following diagnoses is most unlikely?
a. The nephrotic syndrome.
b. The nephritic syndrome.
c. A combined nephrotic and nephritic syndrome.
d. Acute tubular necrosis.
In this case, the urine dipstick suggests the presence
of erythrocytes and leukocytes in the urine, as well as
proteinuria that probably does not reach the nephrotic
range. The urine dipstick measures mainly the
concentration of albumin in the urine, and thus, is
dependent on the total amount of protein in the urine
and the total urine volume. Thus, a reading of 4+
protein by dipstick does not guarantee the presence
of nephrotic-range proteinuria (if oliguria is present)
and a reading of 2+ does not rule out nephrotic-range
proteinuria (if urine volume is large). The findings in
this case are most consistent with a nephritic urine,
although they may also be seen in other conditions
such as acute pyelonephritis or acute tubular
necrosis.
The nephritic syndrome is characterized by the
appearance, at times sudden, of hematuria associated
with proteinuria. The nephritic syndrome may also be
associated with an elevated serum creatinine, oliguria
and hypertension. In the nephritic syndrome, breaks in
the glomerular basement membrane, mainly due to
immunologic phenomena, allow erythrocytes and
leukocytes to enter the urine. Damage to the glomerular
basement membrane also accounts for the presence of
abnormal amounts of protein in the urine.
In contrast to nephritic urine, nephrotic urine
typically contains at most a few erythrocytes
and leukocytes. The dipstick will often be
negative or show only trace amounts of heme
pigment and leukocyte esterase. The dipstick
will usually read 4+ protein, although a large
urine volume may cause the dipstick to be
less strongly positive.
Occasionally, the nephrotic syndrome and the
nephritic syndrome can coexist in a patient.
Examples include lupus nephritis, Henoch-
Shonlein purpura, membranoproliferative
glomerulonephritis and acute renal failure due
to non-steroidal anti-inflammatory drugs. In
these cases, the dipstick usually will be
strongly positive for heme pigment, leukocyte
esterase, and protein.
In acute tubular necrosis, large amounts of
hematuria, pyuria and proteinuria are typically
absent unless there is concurrent damage to
the glomeruli or interstitium. However, in
patients with preexisting intrinsic renal
disease, the dipstick may be positive for
heme, leukocyte esterase and/or protein even
in the absence of acute glomerular or
interstitial disease.
The urine sediment from the patient in the case is
shown above. What is demonstrated?
a. Acanthocytes and dysmorphic erythrocytes
b. Lipid droplets
c. Leukocytes
d. Renal tubular epithelial cells
In hematuria of glomerular origin, most erythrocytes have a
distorted appearance and many are smaller than usually. They
are referred to as dysmorphic erythrocytes. A subtype of
dysmorphic erythrocytes is referred to as acanthocytes.
Acanthocytes (arrow) are ring-shaped erythrocytes with one or
more vesicle-like protrusions. The etiology of dysmorphic
erythrocytes and acanthocytes is thought to be related to
membrane damage that occurs as the erythrocyte passes
through breaks in the glomerular basement membrane.
Acanthocytes (above, left) should be distinguished from
crenated red cells (above, right). Crenated erythrocytes form in
highly concentrated urine. In urine with a high osmolality, water
will pass out of the erythrocyte by osmosis, resulting in a
reduced cell diameter. Crenated erythrocytes have
characteristic spicules, as shown in the slide on the right. In
urine with a low osmolality, water will pass into the erythrocyte
by osmosis, resulting in an increased cell diameter. If enough
water enters the erythrocyte, the cell can lyse.
Lipid droplets (above) can be distinguished from
erythrocytes by their variable size and their color. Lipid
droplets are not found in nephritic urine unless there is a
concurrent nephrotic process, as can occur in
membranoproliferative glomerulonephritis and in some
types of lupus nephritis.
Leukocytes can be present in variable amounts in
nephritic sediment. Leukocytes are granular cells which
are larger than erythrocytes and contain a nucleus that
may be difficult to define. The slide on the right shows
both leukocytes (yellow arrows) and normal erythrocytes.
The slide on the left shows dysmorphic erythrocytes and
acanthocytes for comparison.
Renal tubular epithelial cells (above right, contained within a
cast) are typically seen in conditions which primarily involve
the tubules, such as ATN, interstitial nephritis and acute
allograft rejection. If the inflammation from acute
glomerulonephritis extends to the tubules, renal tubule
epithelial (RTE) cells can occasionally be seen in a nephritic
sediment. In some nephrotic sediments, RTE cells can be
seen due to tubular cell sloughing associated with damage
caused by heavy proteinuria and/or lipid droplet reabsorption.
Examination of our patient’s sediment also showed the two
formed elements shown above. What do they represent?
a. Erythrocyte casts
b. Leukocyte casts
c. Hemoglobin casts
d. Granular casts
Erythrocyte casts are formed in the tubule lumen as
erythrocytes complex with Tamm-Horsfall mucoprotein.
Erythrocyte casts are a marker of bleeding within the nephrons
of the kidney. They are most often seen in glomerulonephritis,
although they can also be seen in acute interstitial nephritis and
renal vasculitis. Although erythrocyte casts are an important
sign of acute glomerulonephritis, they are only variably present
in the nephritic sediment.
Leukocyte casts, as seen in the slide on the left, are seen in
upper urinary tract bacterial infection, although they can also
be seen with non-bacterial renal inflammation due to acute
interstitial nephritis and some forms of acute
glomerulonephritis. The slide on the right shows an
erythrocyte cast. Erythrocytes are smaller than leukocytes,
have a non-granular cytoplasm, and have no nucleus. In
contrast, leukocytes have a granular cytoplasm and have a
nucleus, although the nucleus may sometimes be difficult to
appreciate in an unstained sediment.
Hemoglobin casts are pigmented cellular casts that develop in
the presence of degenerated erythrocytes within the cast
matrix. They are typically brown in color and have a granular
appearance. Focusing up and down on the microscope may
reveal the presence of degenerated erythrocytes within the
hemoglobin cast. Rarely, hemoglobin casts develop in cases of
intravascular hemolysis. In these cases, the dipstick will be
positive for heme but there will be no evidence of microscopic
hematuria, and degenerated erythrocytes will not be present
within the hemoglobin cast.
Another example of a pigmented cast is a bilirubin
cast. Bilirubin in the urine can stain any type of cast,
causing the cast to take on the typical yellow
appearance of bilirubin.
Granular casts, like the one shown above, are a non-specific
finding which can be seen in numerous kidney disorders,
including ones which present with the nephritic syndrome. It is
thought that the granules are composed of degenerating cells
and filtered proteins that have subsequently aggregated within
the renal tubules. Although granular casts are a non-specific
finding, their presence in the sediment suggests the presence
of intrinsic renal disease.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- BAB 3 Daftar PustakaDocument2 pagesBAB 3 Daftar Pustakaemi_bgtNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Daftar Pustaka BaruDocument4 pagesDaftar Pustaka Baruemi_bgtNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Daftar PustakaDocument1 pageDaftar Pustakaemi_bgtNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Yamada Et Al-2015-Journal of Diabetes InvestigationDocument8 pagesYamada Et Al-2015-Journal of Diabetes Investigationemi_bgtNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Daftar Pustak1Document4 pagesDaftar Pustak1emi_bgtNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Pediatricreferencecard 04Document2 pagesPediatricreferencecard 04yesumovsNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Daftar Pustaka....................Document2 pagesDaftar Pustaka....................emi_bgtNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Daftar Pustaka Baru Edit Pas 2 Ke 3Document2 pagesDaftar Pustaka Baru Edit Pas 2 Ke 3emi_bgtNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Daftar Pustaka BaruDocument2 pagesDaftar Pustaka Baruemi_bgtNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Daftar Pustak1Document4 pagesDaftar Pustak1emi_bgtNo ratings yet
- Edwar CBD StoneDocument25 pagesEdwar CBD Stoneemi_bgtNo ratings yet
- Abstract and IntrcoductionDocument16 pagesAbstract and Intrcoductionemi_bgtNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Masked Hypertension and Elevated Nighttime Blood Pressure N CKD: Prevalence and Association With Target Organ DamageDocument2 pagesMasked Hypertension and Elevated Nighttime Blood Pressure N CKD: Prevalence and Association With Target Organ Damageemi_bgtNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Croup Clincal Care Guidelines PDFDocument12 pagesCroup Clincal Care Guidelines PDFe_limantaraNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Therapeutic Potential of AkntiDocument2 pagesTherapeutic Potential of Akntiemi_bgtNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Masked Hypertension and Elevated Nighttime Blood Pressure N CKD: Prevalence and Association With Target Organ DamageDocument2 pagesMasked Hypertension and Elevated Nighttime Blood Pressure N CKD: Prevalence and Association With Target Organ Damageemi_bgtNo ratings yet
- 1234Document2 pages1234emi_bgtNo ratings yet
- Type Equation HereDocument1 pageType Equation Hereemi_bgtNo ratings yet
- Inflammatory Myofibroblastic Tumor of The Liver In.5Document4 pagesInflammatory Myofibroblastic Tumor of The Liver In.5emi_bgtNo ratings yet
- Autoimmune Hepatitis in A Child With Chronic.17Document3 pagesAutoimmune Hepatitis in A Child With Chronic.17emi_bgtNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pi Is 0022347613001194Document3 pagesPi Is 0022347613001194emi_bgtNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Evaluation of The Child With Suspected.4Document8 pagesEvaluation of The Child With Suspected.4emi_bgtNo ratings yet
- 1234Document2 pages1234emi_bgtNo ratings yet
- Liver, Hormones, and Bones.2Document2 pagesLiver, Hormones, and Bones.2emi_bgtNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- 1234Document2 pages1234emi_bgtNo ratings yet
- Renal 2Document7 pagesRenal 2emi_bgtNo ratings yet
- PPOKDocument15 pagesPPOKemi_bgtNo ratings yet
- 1234Document2 pages1234emi_bgtNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- You Did It AgainDocument18 pagesYou Did It AgainIpie BsaNo ratings yet
- Red MeatDocument2 pagesRed Meatemi_bgtNo ratings yet
- Hipocrates - VOLUME 6Document400 pagesHipocrates - VOLUME 6Heitor Murillo CarnioNo ratings yet
- Sermon On Spirituality & Mental Illness by Rev Laura MancusoDocument12 pagesSermon On Spirituality & Mental Illness by Rev Laura MancusoRev. Laura L. MancusoNo ratings yet
- First International congress on clinical Hypnosis & Related Sciences programDocument91 pagesFirst International congress on clinical Hypnosis & Related Sciences programGolnaz BaghdadiNo ratings yet
- GRANDE ICU CASE SUMMARYDocument3 pagesGRANDE ICU CASE SUMMARYanuzNo ratings yet
- MeningitisDocument21 pagesMeningitisSonya GodwinNo ratings yet
- Angina Pectoris: Dr. Naitik D Trivedi & Dr. Upama N. TrivediDocument15 pagesAngina Pectoris: Dr. Naitik D Trivedi & Dr. Upama N. TrivediNaveen KumarNo ratings yet
- Aapi Ebook June 19 2017Document621 pagesAapi Ebook June 19 2017AAPIUSANo ratings yet
- 03 Biosecurity Jit PPT FinalDocument20 pages03 Biosecurity Jit PPT FinalReza WratsongkoNo ratings yet
- MalariaDocument4 pagesMalarianafrabNo ratings yet
- Scientific Breakthroughs in Autophagy MechanismsDocument7 pagesScientific Breakthroughs in Autophagy MechanismshananNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Gastrointestinal Tract Infections: General ConsiderationsDocument17 pagesGastrointestinal Tract Infections: General ConsiderationsDarpan GelalNo ratings yet
- Dementia Presentation Feb 19Document28 pagesDementia Presentation Feb 19Rhu Pugo, La UnionNo ratings yet
- Lesson 1: Health and Skill Related FitnessDocument2 pagesLesson 1: Health and Skill Related FitnessCrhystal Joy ReginioNo ratings yet
- MidtermDocument22 pagesMidtermEmvie Loyd Pagunsan-ItableNo ratings yet
- The Politics of The Asia-Pacific Triumphs, Challenges, and Threats (Mark S. Williams (Editor)Document381 pagesThe Politics of The Asia-Pacific Triumphs, Challenges, and Threats (Mark S. Williams (Editor)lelenaNo ratings yet
- Kim (2015) - Lemon Detox Diet Reduced Body FatDocument12 pagesKim (2015) - Lemon Detox Diet Reduced Body FatRodrigo MelloNo ratings yet
- Colposcopic Findings Prepubertal Assessed For Sexual Abuse: Genital GirlsDocument5 pagesColposcopic Findings Prepubertal Assessed For Sexual Abuse: Genital GirlsSusi PuspitaNo ratings yet
- Severe Acute Respiratory Syndrome Coronavirus 2Document31 pagesSevere Acute Respiratory Syndrome Coronavirus 2Ian VillacrusisNo ratings yet
- Elective Caesarean Section on a GoatDocument17 pagesElective Caesarean Section on a GoatAbdirazak AlkhaalidNo ratings yet
- Chapter 2 Herbs That Clear HeatDocument159 pagesChapter 2 Herbs That Clear HeatCarleta Stan100% (1)
- Cystic HygromaDocument12 pagesCystic Hygromaraymond onyekaNo ratings yet
- Pug BookDocument152 pagesPug BookArtemio SotomayorNo ratings yet
- Genetics of Mitochondrial Disease: Russell P. SanetoDocument54 pagesGenetics of Mitochondrial Disease: Russell P. SanetoGréta BotyánszkiNo ratings yet
- Emergency Ultrasound教學 (8) 急診超音波在深部靜脈栓塞之應用Document40 pagesEmergency Ultrasound教學 (8) 急診超音波在深部靜脈栓塞之應用juice119No ratings yet
- Production and Evaluation of Smoothies Made From Various Fruits Sold in Lagos MarketDocument5 pagesProduction and Evaluation of Smoothies Made From Various Fruits Sold in Lagos MarketInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Foodborne IllnessDocument2 pagesFoodborne IllnessBjorni VaniNo ratings yet
- Medical TerminologyDocument10 pagesMedical Terminologyfreedomx0a100% (2)
- Transfusion-Related Acute Lung Injury: HistoryDocument20 pagesTransfusion-Related Acute Lung Injury: HistoryBladimir CentenoNo ratings yet
- CHAPTER II Open BurningDocument6 pagesCHAPTER II Open Burningjedric_14100% (1)
- Border Terrier Ukc StandardDocument2 pagesBorder Terrier Ukc Standardapi-342444556No ratings yet