Professional Documents
Culture Documents
Regenerative Medicine
Uploaded by
The Royal Society of EdinburghOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Regenerative Medicine
Uploaded by
The Royal Society of EdinburghCopyright:
Available Formats
The Royal Society of Edinburgh
Supported by the Beacons of Public Engagement (Edinburgh Beltane) Discussion Forum Regenerative Medicine: How will it change my life? 24 November 2008 Report by Jennifer Trueland
Definition: Broadly, regenerative medicine is the umbrella term for innovative medical therapies which allow the body to repair or regenerate damaged or diseased cells, tissues or organs. This includes technologies which use stem cells capacity to grow into the different cells of the body. Introduction/Summary Writing in the 17th century, Joseph Glanvill, a founding member of the Royal Society, said that one day grey hairs might be restored to juvenility and that exhausted marrow might be renewed without a miracle. Almost 350 years later these lines were quoted at the RSE, this time by Dr Brendon Noble, a scientist who is helping to make them come true. He and colleagues at Edinburgh Universitys Centre for Regenerative Medicine which had been launched officially earlier that day are using stem cells to regenerate bone and cartilage, work which will potentially revolutionise treatment for people with conditions including arthritis and bone fractures. The RSE event, supported by Edinburgh Beltane, one of the UKs beacons for public engagement, asked what regenerative medicine was and what it might do. Three distinguished speakers Dr Noble, Dr Anna Krassowska and Professor Hamish Simpson gave short presentations then the bulk of the evening was made up of discussion and questions. Dr Anna Krassowska, formerly research manager with the UK Stem Cell Foundation, gave an overview of the current state of play and potential of stem cell research. Dr Noble described some of his laboratory-based research, which is working with stem cells to grow bone and cartilage and make them into therapies. Dr Simpson, an orthopaedic surgeon, spoke of how such technologies could benefit patients in practice and, importantly, said some could be available in the next few years. A number of challenges were brought out during the discussion, including the need for a strong, wellfunded research base in Scotland and the importance of a regulatory environment which is robust and safe, but does not stifle innovation. The importance of engaging the public with the issues was emphasised throughout. Dr Anna Krassowska, former Research Manager, UK Stem Cell Foundation Dr Krassowska described how regenerative medicines, including stem cell technologies, have potential in many different chronic conditions which are caused by the loss of specific cell types. These include diabetes, where there is a loss of insulin-secreting cells, and Parkinsons, where the dopamine-secreting cells are lost. Others include spinal cord injury, osteoarthritis and heart disease. The idea is that one can take damaged cells and replace them by transplantation or encourage endogenous cells to replenish, she said. There were several areas with proof of concept the first real evidence that something works including a Canadian study where insulin-secreting cells were transplanted into patients with diabetes, who then became less dependent on insulin. There were challenges, however. For example, the diabetes study required cells from 2 3 donors for just one patient, which would hinder large-scale treatment programmes. She described the different types of cells which had the ability or potential to develop into other cells in the body. In particular, she spoke about the stem cells which come from embryos, and which are
particularly flexible in terms of the type of cells they can grow into. She also spoke about adult stem cells, which are less flexible, but have potential in a number of therapeutic areas. Stem cells can be taken from a persons own body for example, from bone marrow or (with planning ahead) from umbilical cord blood which lessens the risk of the body rejecting them because of an immune response. But Dr Krassowska also described allogeneic treatments, where a bank of cells is created and stored at hospital sites to be used when needed. Again there are challenges, including making sure the stem cells grow into the right thing. You dont want bone growing in the heart, she said. Although there is promising research, for example in heart disease, it is still early days. Dr Brendon Noble, MRC Centre for Regenerative Medicine, University of Edinburgh Dr Noble began by describing the mythical Hydra the creature which grew two heads for each one that was cut off calling it an early experiment in regenerative medicine. His work in Edinburgh, however, is concerned with bone rather than monster heads. He talked about mesenchymal stem cells, which are found in bone marrow and which have the potential to grow into bone and cartilage, among other cells. Although work in the lab has been relatively promising, he said there is a need for a reality check. Persuading the cells to survive in real patients is more challenging, partly because they are going into a harsh environment the previous bone or cartilage cells didnt like it there, so why should the new ones? Rather than send in the new cells unarmed to a hostile environment, his scientists are trying to find a way of protecting them. This can involve a protective, bioactive scaffold which keeps the cells alive so that they can do their stuff. In Edinburgh, Dr Noble and his team have been testing different materials to see which ones the cells will be happy with. Early results have been promising, he said, with bone growing where it wouldnt have done and authentic-looking cartilage being produced. If successful, some of Dr Nobles work will be placed in a clinical trial in 2 years time. Professor Hamish Simpson, Scottish Centre for Regenerative Medicine and Professor of Orthopaedics and Trauma at the University of Edinburgh Following on from Dr Nobles description of the work being done in the laboratory, Professor Simpson gave an overview of what it could mean for patients. He described the great clinical need for more effective treatments for bone injury and disease, talked about conditions which might benefit from stem cell technologies then gave his assessment of how soon treatments might be available. He also emphasised the importance of translational medicine, which is taking discoveries from the lab bench to the patient bedside and back again. And he spoke about the human side of musculo-skeletal problems, including a patient who had to undergo years of treatment, losing his job and marriage in the process. Hip and knee replacements had been a great boon, he said, but did not suit everyone and were difficult to repair. Better alternatives were needed. Similarly, although 95 per cent of fractures heal well, the remainder, the non-union ones, fail to heal. He described work which has been done to regrow bone to fill gaps left where bone has died and had to be removed. He is optimistic that treatment will be available within a very few years to repair small, localised defects in cartilage, which affect some 2,000 people in the UK each year. Similarly, ways of dealing with non-union fractures should be available in the short term. Using stem cells to treat osteoarthritis and large bone defects are long-term ambitions, however.
He spoke of the challenges in clinical trials, including developing objective outcome measures and finding enough similar patients to take part. Getting cells of sufficient quality and winning ethical approval can also be difficult. Discussion The discussion session was chaired by Professor Mary Bownes, Vice-Principal for research, training and community relations with the University of Edinburgh, who also heads the Edinburgh Beltane. She opened with a short explanation of the work of that project, which includes all the higher education institutions in Edinburgh and other organisations including the RSE. One of six UK beacons of public engagement, its aim is to help scientists engage more with the public and vice versa, changing cultures, improving understanding and influencing policy. The involvement of Edinburgh Beltane proved topical, with more than one member of the audience asking for more information and engagement. The questions ranged from the personal and specific to more general points. The recently reported case of the operation performed on a woman in Spain to replace her windpipe was raised several times. Asked about its relevance to regenerative medicine, Dr Noble explained that the patient had been given a trachea which had her own cartilage-forming stem cells added. Professor Simpson added that the trachea, which had been taken from a cadaver and had had all its own cells removed, would have acted as a kind of mechanical strut to allow the stem cells to grow. One member of the audience asked if the development of regenerative medicine would put people under more pressure to have treatments or if perhaps they would choose to terminate their lives earlier. The panel responded that, in effect, it was just another medicine or therapy, which people would have the right to refuse, so it didnt change the current situation. Professor Simpson added that new therapies might be more about improving the quality of life, not extending it in all cases, and that this improved quality might change peoples minds about whether they wanted to undergo treatment or not. One questioner asked about collaborative research across universities, remarking that Scotland appeared to be leading the way with regenerative medicine. Dr Noble said that the Scottish Stem Cell Network was a fantastic way of promoting collaboration and networking and Professor Simpson said that trials involved many centres. Asked if stem cell therapy might be used in birth defects, such as those related to thalidomide, Prof Simpson said that would be a bigger challenge because it would involve growing muscle as well as bone. But Dr Noble said that treatments for even genetic conditions were not ruled out. One woman in the audience offered herself up as a guinea pig for Dr Nobles research and asked what was being done to make GPs aware of new developments. She also asked if steps forward in treatment would be patient-driven or if she had to wait for her GP. Dr Noble said it was too early to say which patients would be suitable for trials and Professor Simpson said that patients would probably be recruited from orthopaedics clinics, so it was important that colleagues knew where trials were happening. He defended GPs, saying they had a lot to keep up with so wouldnt necessarily know about possible future trials. Asked about the difference between adult and embryonic stem cells (to which some people have an ethical objection) the panel said that while they could be used for many of the same things, embryonic cells could develop more cell types. However, Dr Noble said that he was convinced that patients would be informed about the origin of the cells. Asked about the main policy issues, the panel mentioned several, including funding, the regulatory environment getting over the various hurdles to run trials and licence treatments and the importance of keeping a workforce with expertise in Scotland.
Professor Bownes asked how much regenerative medicine would cost. Dr Noble said it would be similar to other drug discovery expensive to develop and bring to market, but less expensive later. Dr Krassowska has a vision of off the shelf products, such as heart cells which have been frozen in vials and used to treat people who come into hospital needing urgent therapy. Professor Simpson pointed out that current treatment for a person with severe bone trauma can run into hundreds of thousands of pounds. Asked if it would be possible to grow large organs like hearts or lungs, Dr Noble said that while this was not possible at the moment it might be one day. Who knows? he asked. Professor Simpson said it was difficult to get the interconnectivity right the liver has to hook up to several vascular systems, for example. Talking about the regulatory environment in the UK, Dr Noble said that although it involved hurdles, he was glad it was there. Dr Krassowska said clinics in other countries are offering expensive stem cell therapies which have not been proven and could be dangerous, to vulnerable, desperate people. Theres no long term follow-up, nobody is learning anything, she added. The audience was keen for the public to learn more. One said medical meetings should be opened up. The panel said that the public could attend many medical meetings and that patient interest groups and charities were a good source of information. Dr Krassowska said that many of her scientific colleagues regularly gave talks to such groups. Professor Bownes said that this is the sort of thing that the beacons of public engagement are trying to promote. The debate wasnt closed with the end of this meeting, she said, and asked that anyone who had further points or suggestions get in touch with the Edinburgh Beltane.
Opinions expressed here do not necessarily represent the views of the RSE, nor of its Fellows The Royal Society of Edinburgh, Scotlands National Academy, is Scottish Charity No. SC000470
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Enlightening The Constitutional DebateDocument128 pagesEnlightening The Constitutional DebateThe Royal Society of EdinburghNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Economy, Energy and Tourism Committee Inquiry Into Scotland's Economic Future Post-2014Document8 pagesEconomy, Energy and Tourism Committee Inquiry Into Scotland's Economic Future Post-2014The Royal Society of EdinburghNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Currency Banking and Tax Jan 2014Document8 pagesCurrency Banking and Tax Jan 2014The Royal Society of EdinburghNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Food Scotland BillDocument2 pagesThe Food Scotland BillThe Royal Society of EdinburghNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- BBC Trust Consultation On Draft Guidelines For The Coverage of The Referendum On Independence For ScotlandDocument2 pagesBBC Trust Consultation On Draft Guidelines For The Coverage of The Referendum On Independence For ScotlandThe Royal Society of EdinburghNo ratings yet
- BBC Trust Service Review On News and Current AffairsDocument2 pagesBBC Trust Service Review On News and Current AffairsThe Royal Society of EdinburghNo ratings yet
- Enlightening The Constitutional DebateDocument128 pagesEnlightening The Constitutional DebateThe Royal Society of EdinburghNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- National Performance FrameworkDocument4 pagesNational Performance FrameworkThe Royal Society of EdinburghNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- New Waves in Marine EnergyDocument5 pagesNew Waves in Marine EnergyThe Royal Society of EdinburghNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Review of Sessions 2008-2009 and 2009-2010Document511 pagesReview of Sessions 2008-2009 and 2009-2010The Royal Society of EdinburghNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Real EconomyDocument8 pagesThe Real EconomyThe Royal Society of EdinburghNo ratings yet
- EIF 2013 Leisure RevolutionDocument4 pagesEIF 2013 Leisure RevolutionThe Royal Society of EdinburghNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Enlightening The Constitutional Debate - Defence and International RelationsDocument8 pagesEnlightening The Constitutional Debate - Defence and International RelationsThe Royal Society of EdinburghNo ratings yet
- Scotland RocksDocument4 pagesScotland RocksThe Royal Society of EdinburghNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- English and ScotsDocument4 pagesEnglish and ScotsThe Royal Society of EdinburghNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
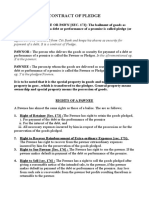
- Contract of PledgeDocument4 pagesContract of Pledgeshreya patilNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Birds (Aves) Are A Group Of: WingsDocument1 pageBirds (Aves) Are A Group Of: WingsGabriel Angelo AbrauNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Faringitis StreptococcusDocument16 pagesFaringitis StreptococcusnurNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Complete Admin Law OutlineDocument135 pagesComplete Admin Law Outlinemarlena100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Mathematics Grade 5 Quarter 2: Answer KeyDocument4 pagesMathematics Grade 5 Quarter 2: Answer KeyApril Jean Cahoy100% (2)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- ĐỀ THI DỰ ĐOÁN 9Document4 pagesĐỀ THI DỰ ĐOÁN 9tranvananh2041985No ratings yet
- Chapter 3 - the-WPS OfficeDocument15 pagesChapter 3 - the-WPS Officekyoshiro RyotaNo ratings yet
- Introduction To Public HealthDocument54 pagesIntroduction To Public HealthKristelle Marie Enanoria Bardon50% (2)
- Evaluation of The Agricultural Land Utilization Types For Mitigation of Land Degradation in Giritirta, Pejawaran, BanjarnegaraDocument15 pagesEvaluation of The Agricultural Land Utilization Types For Mitigation of Land Degradation in Giritirta, Pejawaran, BanjarnegaraTasyaNo ratings yet
- Bgs Chapter 2Document33 pagesBgs Chapter 2KiranShettyNo ratings yet
- 1 Mark QuestionsDocument8 pages1 Mark QuestionsPhani Chintu100% (2)
- Key Performance IndicatorsDocument15 pagesKey Performance IndicatorsAbdul HafeezNo ratings yet
- Reported SpeechDocument2 pagesReported SpeechmayerlyNo ratings yet
- Physics Syllabus PDFDocument17 pagesPhysics Syllabus PDFCharles Ghati100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- 67-Article Text-118-1-10-20181206Document12 pages67-Article Text-118-1-10-20181206MadelNo ratings yet
- Thermal Physics Questions IB Question BankDocument43 pagesThermal Physics Questions IB Question BankIBBhuvi Jain100% (1)
- CSEC Eng A Summary ExerciseDocument1 pageCSEC Eng A Summary ExerciseArisha NicholsNo ratings yet
- 25 ConstitutionDocument150 pages25 ConstitutionSaddy MehmoodbuttNo ratings yet
- BHP Billiton Foundations For Graduates Program Brochure 2012Document4 pagesBHP Billiton Foundations For Graduates Program Brochure 2012JulchairulNo ratings yet
- Configuration Steps - Settlement Management in S - 4 HANA - SAP BlogsDocument30 pagesConfiguration Steps - Settlement Management in S - 4 HANA - SAP Blogsenza100% (4)
- 30 Linux System Monitoring Tools Every SysAdmin Should Know - NixcraftDocument90 pages30 Linux System Monitoring Tools Every SysAdmin Should Know - Nixcraftvignesh05No ratings yet
- Esse 3600Document15 pagesEsse 3600api-324911878100% (1)
- Digital Sytems Counters and Registers: Dce DceDocument17 pagesDigital Sytems Counters and Registers: Dce DcePhan Gia AnhNo ratings yet
- Directions: Choose The Best Answer For Each Multiple Choice Question. Write The Best Answer On The BlankDocument2 pagesDirections: Choose The Best Answer For Each Multiple Choice Question. Write The Best Answer On The BlankRanulfo MayolNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Sayyid Jamal Al-Din Muhammad B. Safdar Al-Afghani (1838-1897)Document8 pagesSayyid Jamal Al-Din Muhammad B. Safdar Al-Afghani (1838-1897)Itslee NxNo ratings yet
- Rita Ora - Shine Ya LightDocument4 pagesRita Ora - Shine Ya LightkatparaNo ratings yet
- Effect of Intensive Health Education On Adherence To Treatment in Sputum Positive Pulmonary Tuberculosis PatientsDocument6 pagesEffect of Intensive Health Education On Adherence To Treatment in Sputum Positive Pulmonary Tuberculosis PatientspocutindahNo ratings yet
- Storage Emulated 0 Android Data Com - Cv.docscanner Cache How-China-Engages-South-Asia-Themes-Partners-and-ToolsDocument140 pagesStorage Emulated 0 Android Data Com - Cv.docscanner Cache How-China-Engages-South-Asia-Themes-Partners-and-Toolsrahul kumarNo ratings yet
- Genpact - Job Description - One Data and AI - B Tech Circuit and MCA (3) 2Document4 pagesGenpact - Job Description - One Data and AI - B Tech Circuit and MCA (3) 2SHIVANSH SRIVASTAVA (RA2011053010013)No ratings yet
- History of Drugs (Autosaved)Document68 pagesHistory of Drugs (Autosaved)Juan TowTowNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)