Professional Documents
Culture Documents
Does Chocolate Reduce Blood Pressure
Uploaded by
akaduthilaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Does Chocolate Reduce Blood Pressure
Uploaded by
akaduthilaCopyright:
Available Formats
Dark Chocolate May Help Control Elevated Blood Pressure CME
News Author: Laurie Barclay, MD CME Author: Laurie Barclay, MD July 1, 2010 Dark chocolate may help control elevated blood pressure (BP), according to the results of a meta-analysis reported in the June 28 issue of BMC Medicine. "Flavanols have been shown to increase the formation of endothelial nitric oxide, which promotes vasodilation and consequently may lower blood pressure," said lead author Karin Ried, from the University of Adelaide, Adelaide, Australia, in a news release. "There have, however, been conflicting results as to the real-life effects of eating chocolate. We've found that consumption can significantly, albeit modestly, reduce blood pressure for people with high blood pressure but not for people with normal blood pressure." The goal of this meta-analysis was to review recent evidence on the effect of flavanol-rich cocoa products on BP in individuals with hypertension and in those with BP within the normotensive range. To identify randomized controlled trials of the effect of cocoa vs placebo on systolic and diastolic BP (SBP/DBP), the investigators searched MEDLINE, Cochrane, and international trial registries from 1955 to 2009. Minimal duration of included trials was 2 weeks. For all studies meeting the inclusion criteria, the investigators performed random-effects metaanalysis. In addition, they performed subgroup analysis according to baseline BP being in the hypertensive or normotensive range. The relationship between type of treatment, dosage, duration, or baseline BP and BP outcome was examined with meta-regression analysis. Selection criteria were met by 15 trial groups of 13 evaluated studies. Compared with placebo, cocoa-chocolate significantly lowered BP, according to a pooled meta-analysis of all trials, which showed a mean change in SBP of 3.2 1.9 mm Hg (P = .001) and DBP of 2.0 1.3 mm Hg (P = .003). On the basis of subgroup meta-analysis, however, cocoa-chocolate had a significant effect vs placebo only in the hypertensive or prehypertensive subgroups (SBP: 5.0 3.0 mm Hg; P = .0009; DBP: 2.7 2.2 mm Hg; P = .01). In the normotensive subgroups, BP was not significantly decreased for cocoa-chocolate vs placebo (SBP: 1.6 2.3 mm Hg; P = .17; DBP: 1.3 1.6 mm Hg; P = .12). "The practicability of chocolate or cocoa drinks as long-term treatment is questionable," Dr. Ried said. Study design and type of control used were borderline significant, but possibly indirect, predictors for BP outcome, according to results of meta-regression analysis. Limitations of this meta-analysis include high heterogeneity in the hypertensive subgroups. Effect sizes and levels of significance of the subgroup meta-analyses of trials with subjects with (pre-)hypertension at baseline should therefore be interpreted more cautiously. "Our meta-analysis suggests that dark chocolate is superior to placebo in reducing systolic hypertension or diastolic prehypertension," the study authors write. "Flavanol-rich chocolate did not significantly reduce mean blood pressure below 140 mmHg systolic or 80 mmHg diastolic." This study was supported by the Royal Australian College of General Practitioners (RACGP) 2006 Cardiovascular Health Research Grant, and the Australian Government Primary Health Care Research Evaluation Development (PHCRED) Program. The study authors have disclosed no
relevant financial relationships. BMC Medicine. Published online June 28, 2010. Abstract
Clinical Context
Hypertension is a well-known and significant risk factor for cardiovascular disease. Flavanols in dark chocolate increase endothelial nitric oxide formation, which promotes vasodilation and lowers BP. As an alternative treatment of hypertension, dark chocolate and flavanol-rich cocoa products have been studied in several controlled trials. Although previous meta-analyses suggested that cocoa-rich foods may lower BP, several recent trials have shown conflicting findings.
Study Highlights
This meta-analysis aimed to summarize recent findings on the effect of flavanol-rich cocoa products on BP in subjects with hypertension and those with BP within the normal range. The investigators searched MEDLINE, Cochrane, and international trial registries from 1955 to 2009. Selection criteria were randomized controlled trials of cocoa vs placebo on SBP and DBP, with duration of at least 2 weeks. The researchers performed random-effects meta-analysis for all randomized controlled trials meeting selection criteria. Subgroups based on hypertensive or normotensive BP at baseline were also analyzed. Meta-regression analysis evaluated the association between treatment type, dosage, duration, or baseline BP with BP outcome. 15 trial groups of 13 evaluated studies met selection criteria. Of the 15 trial groups, 9 compared chocolate containing 50% to 70% cocoa vs white chocolate or other cocoa-free controls, and 6 trial groups compared high-flavanol vs lowflavanol cocoa products. In the active treatment groups, daily flavanol dosages ranged from 30 to 1000 mg. Duration of the interventions was 2 to 18 weeks. In a pooled meta-analysis of all included randomized controlled trials, cocoa-chocolate vs placebo significantly lowered BP. In the meta-analysis of all included randomized controlled trials, mean change in SBP was 3.2 1.9 mm Hg (P = .001), and mean change in DBP was 2.0 1.3 mm Hg (P = .003). In subgroup meta-analysis, cocoa-chocolate vs placebo had a significant effect only in the hypertensive or prehypertensive subgroups (SBP: 5.0 3.0 mm Hg; P = .0009; DBP: 2.7 2.2 mm Hg; P = .01). For individuals with hypertension, the 5-mm Hg reduction in SBP may be clinically meaningful and is comparable to the effects of 30 daily minutes of physical activity (4 - 9 mm Hg). Theoretic risk reduction of a cardiovascular event for the 5-mm Hg decrease in SBP for individuals with hypertension could be approximately 20% during 5 years. However, the investigators note that long-term treatment with chocolate or cocoa drinks is of questionable practicability. For cocoa-chocolate vs placebo, BP was not significantly decreased in the normotensive subgroups (SBP: 1.6 2.3 mm Hg; P =.17; DBP: 1.3 1.6 mm Hg; P = .12). In meta-regression analysis, study design (parallel vs crossover) and type of control (flavanol-free vs low-flavanol) were borderline significant, but possibly indirect, predictors
for BP outcome. Dosage, duration, quality of trials, age, and body mass index were not associated with BP outcome, based on meta-regression analysis. On the basis of these findings, the investigators concluded that dark chocolate is superior to placebo in reducing systolic hypertension or diastolic prehypertension. However, they noted that flavanol-rich chocolate did not significantly lower mean BP lower than 140 mm Hg systolic or 80 mm Hg diastolic. Limitations of meta-analysis included high heterogeneity in the hypertensive subgroups. Effect sizes and significance of the subgroup meta-analyses of trials in the (pre-)hypertensive groups should therefore be interpreted with caution.
Clinical Implications
In a pooled meta-analysis of all included randomized controlled trials, cocoa-chocolate vs placebo significantly lowered BP. However, the investigators note that long-term treatment with chocolate or cocoa drinks is of questionable practicability. In subgroup meta-analysis, cocoa-chocolate vs placebo had a significant effect only in the hypertensive or prehypertensive subgroups. For individuals with hypertension, the 5-mm Hg reduction in SBP may be clinically meaningful and is comparable to the effects of 30 minutes daily of physical activity.
You might also like
- Does Chocolate Reduce Blood PressureDocument3 pagesDoes Chocolate Reduce Blood PressureakaduthilaNo ratings yet
- AndhrapradeshDocument22 pagesAndhrapradeshakaduthilaNo ratings yet
- 27 TreesDocument2 pages27 TreesakaduthilaNo ratings yet
- Significance of Echinocytosis in Blood SmearsDocument4 pagesSignificance of Echinocytosis in Blood SmearsakaduthilaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Survival of The Sickest PresentationDocument24 pagesSurvival of The Sickest Presentationapi-255985788No ratings yet
- Oet Reading Part A Additional - GlucomaDocument8 pagesOet Reading Part A Additional - Glucomaafacean25% (8)
- Transport Technology Center (T.T.C)Document19 pagesTransport Technology Center (T.T.C)Abubakar Lawan GogoriNo ratings yet
- 10 Doh Approved Herbal MedicineDocument32 pages10 Doh Approved Herbal MedicineIsmael JaaniNo ratings yet
- 2020 DWTC Event Calendar EnglishDocument4 pages2020 DWTC Event Calendar EnglishMustazhar0% (1)
- عقد خدمDocument2 pagesعقد خدمtasheelonlineNo ratings yet
- K55 MSDSDocument7 pagesK55 MSDSalocNo ratings yet
- Lesson 1 Local Government's Historical BackgroundDocument16 pagesLesson 1 Local Government's Historical BackgroundLorienelNo ratings yet
- 1866 PSC Iasc Ref Guidance t2 DigitalDocument11 pages1866 PSC Iasc Ref Guidance t2 DigitalDama BothNo ratings yet
- Prepared By: Ulfat Amin MSC Pediatric NursingDocument25 pagesPrepared By: Ulfat Amin MSC Pediatric NursingAngelic khanNo ratings yet
- Reviews of Two Works by Dr. Amy Baker.Document9 pagesReviews of Two Works by Dr. Amy Baker.Talia SchwartzNo ratings yet
- Q1. Read The Passage Given Below and Answer The Questions That FollowDocument2 pagesQ1. Read The Passage Given Below and Answer The Questions That FollowUdikshaNo ratings yet
- Kidde Fire Systems Nitrogen Engineered Systems: Design, Installation, Operation and Maintenance ManualDocument110 pagesKidde Fire Systems Nitrogen Engineered Systems: Design, Installation, Operation and Maintenance ManualYoyon HaryonoNo ratings yet
- Assessed Conference Presentations ScheduleDocument2 pagesAssessed Conference Presentations ScheduleAna Maria Uribe AguirreNo ratings yet
- Brett Stolberg 100112479 - ResumeDocument1 pageBrett Stolberg 100112479 - Resumeapi-193834982No ratings yet
- The NBCP Referral Code SubDocument4 pagesThe NBCP Referral Code SubArcon Solite BarbanidaNo ratings yet
- HSE List of PublicationsDocument12 pagesHSE List of PublicationsDanijel PindrićNo ratings yet
- Case Study - Genetic DisordersDocument3 pagesCase Study - Genetic Disordersapi-340003532100% (1)
- الورقة الثالثة- القبالة-2Document4 pagesالورقة الثالثة- القبالة-2Habebt MusabNo ratings yet
- AgraLi The Low Chloride Liquid Fertilizer For Sensitive Crops enDocument2 pagesAgraLi The Low Chloride Liquid Fertilizer For Sensitive Crops enASHNo ratings yet
- Nres1dm-Chapter I and IIDocument35 pagesNres1dm-Chapter I and IImlmmandapNo ratings yet
- Family Nursing Care PlanDocument1 pageFamily Nursing Care PlanDersly LaneNo ratings yet
- (SEIU) Out Loud Sodexo Workers From Seven Countries Speak Out On Human RightsDocument30 pages(SEIU) Out Loud Sodexo Workers From Seven Countries Speak Out On Human RightsNewThorHinoNo ratings yet
- Undulating Periodization For BodybuildingDocument24 pagesUndulating Periodization For BodybuildingPete Puza89% (9)
- 380 Final PaperDocument46 pages380 Final Paperapi-538048965No ratings yet
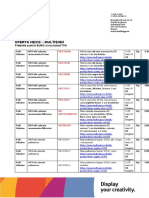
- Oferta Hexis - Multisign: Preturile Sunt in EURO Si Nu Includ TVADocument9 pagesOferta Hexis - Multisign: Preturile Sunt in EURO Si Nu Includ TVAPoschina CiprianNo ratings yet
- Anatomy of Writing For Publication For Nurses PDFDocument369 pagesAnatomy of Writing For Publication For Nurses PDFfernlover3901100% (1)
- GastroparesisDocument10 pagesGastroparesisapi-437831510No ratings yet
- Factors Affecting Social Science Teachers' Burnout in Selected State Universities in The PhilippinesDocument41 pagesFactors Affecting Social Science Teachers' Burnout in Selected State Universities in The PhilippinesAmadeus Fernando M. Pagente100% (1)
- Human Sexual Response Physiology PhasesDocument2 pagesHuman Sexual Response Physiology PhasesLovely HerreraNo ratings yet