Professional Documents
Culture Documents
Anti Tussive Tranx
Uploaded by
Aaron Christian Earl VillosoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anti Tussive Tranx
Uploaded by
Aaron Christian Earl VillosoCopyright:
Available Formats
Subject: Pharmacology Topic: Antitussives Lecturer: Dra.
Aguinaldo Date of Lecture: October 2, 2011 Transcriptionist: The Soloist Pages: 8
COUGH Cough is a powerful physiological mechanism that causes the central It is characterized by a violent expiration, which provides the high flow rates that are required to shear away mucus and remove foreign particles from the larynx, trachea, and large bronchi. Most sensory stimuli that cause coughing also increase airway secretion, which is beneficial as this provides a vehicle for expulsion of particulate matter. Cough Receptors Cough usually results from the stimulation of sensory nerves in the airways. The nerves that initiate cough are predominantly in the upper airway, for it is here that the greatest protection against the ingress of foreign material is required. The sensor and central components of the reflex arc are targets for drugs that suppress cough: Through reducing receptor activation or activity in the afferent nerves Reducing sensitivity of the cough center The afferent limb includes receptors within the sensory distribution of the trigeminal, glossopharyngeal, superior laryngeal, and vagus nerves As a reflex mechanism, the cough involves an arc with central, sensory and efferent components. The exact nature of the sensory receptors of cough are unknown. Anatomically, cough sensitive nerves extend from the larynx to the division of the segmental bronchi. The exact pathway of the afferent pathways involved in cough and the exact location of the CNS relay (cough center) are also unknown. The efferent pathway for cough involves the intercostal and phrenic nerves. Abrupt contraction of the respiratory muscles leads to an explosive rise in intrathoracic pressure, which airways to be cleared of foreign material and excess secretion
SY 2011-2012
forces air out of the alveoli and through the airways.
The vagus nerves are known to carry the sensory information from the lung which initiates the cough reflex, as cough from stimulation of one side of the bronchial tree is abolished by ipsilateral vagotomy. The lung has three types of sensory nerves: slowly adapting stretch receptors, rapidly adapting stretch receptors (or "irritant receptors"), and C fibre endings. The latter are subdivided into pulmonary C fibre endings and bronchial C fibre endings, depending on the source of their blood supply. Cough caused by mechanical irritation results from stimulation of myelinated or non myelinated sensory nerves in the larynx or the rapidly adapting stretch receptors in the lung, or both. Cough caused by direct chemical stimulation results from activation of receptors in the larynx (myelinated or non-myelinated) or activation of C fibre endings in the lung, or both. The prevalence of cough in the population depends on the prevalence of smoking and other environmental factors and in different populations has varied from 5% to 40%. One indication of the size of the problem is the self prescription of over the counter antitussives, which has been estimated at 75 million doses per annum in the United Kingdom. *TYPES OF COUGH 1. ACUTE COUGH: lasts less than 3 weeks CAUSES: Upper respiratory infections i.e. common cold, acute bacterial sinusitis, pertussis, exacerbations of COPD, allergic rhinitis and rhinitis due to environmental irritants NOTE: Estimating the duration of cough is the first step in narrowing the list of possible diagnoses. The four phases of cough
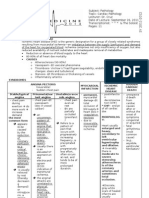
Treatment for Acute Cough Cause Common cold Therapeutic option Dexbromphenirami ne 6mg, plus pseudoephedrine, 120 mg daily for 1 week or naproxen 500mg LD then 500mg TID x 5 days, or ipratropium nasal spray 2 sprays per nostril 3-4x/d as needed for 4 days Avoidance of allergens; Loratidine 10mg OD Dextropheniramine + pseudoephedrine BID x 1 week; Oxymetazoline 2 sprays daily OD x 5 days; Treat for H. influenzae and S.pneumoniae Antibiotic vs. H. influenzae and S. pneumoniae; Systemic corticosteroids tapered over 2 weeks; continous oxygen as needed; Ipratropium + albuterol, cessation of smoking Erythromycin 500mg QID x 14 days or if allergic, Co-tri 160-800mg BID x 14 days
CAUSES: post infectious cough, subacute bacterial sinusitis, bordetella pertussis, asthma Treatment for Subacute Cough
Allergic rhinitis Acute bacterial sinusitis
Causes Postnasal drip syndromes: Nonallergic rhinitis Allergic rhinitis
Exacerbation of COPD
Vasomotor rhinitis Chronic bacterial sinusitis
Bordetella pertussis infection
Asthma
GERD
Chronic Bronchitis 2. SUBACUTE COUGH: lasts from 3-8 weeks ACE inhibitors Eosinophilic bronchitis
Therapeutic options Dexbromphenira mine + pseudoephedrine x 3 weeks or ipratropium nasal spray for 3 weeks Avoidance of offending allergens; Loratidine 10 mg BID Ipratopium nasal spray x 3 weeks then as needed Dexbrophenirami ne+ pseudoephedrine for 3 weeks; oxymetazoline for 5 days;specific antibiotic therapy ( H. influenzae, Strep and anaerobes) Beclomethasone and albuterol as metered dose inhaler Modifications of diet and lifestyle Acid suppression Prokinetic therapy Elimination of irritant; Ipratropium by metered dose inhaler Discontinuance of the drug Inhaled budesonide 7 400g BID x 14 days
Treatment for Chronic Cough Cause Postinfection Therapeutic option Dexbromphenira mine + pseudoephedrine x 1 week or ipratropium nasal spray x 1-3 weeks; systemic corticostreroids tapered over 2-3 weeks; central antitussives Erythromycin x 14 days or Cotrimoxazole Dexbromphenira mine + pseudoephedrine x 3 weeks; Oxymetazoline x 5 days; antibiotics Beclomethasone, albuterol - Drugs that bind to specific pharmacologic receptors affecting on well-defined areas of the CNS and peripheral NS. - Intended to reduce coughing regardless of etiology - Used when the excitability &/or intensity of the cough is elevated over what is required to defend the airways
B. Pertussis infection Subacute bacterial sinusitis
Asthma
3. CHRONIC COUGH : lasting more than 8 weeks CAUSES: post-nasal drip syndromes (most common), chronic bacterial sinusitis, asthma, gastroesophageal reflux disease (GERD), chronic bronchitis, angiotensin-converting enzyme (ACE) inhibitors, eosinophilic bronchitis.
CLASSIFICATION: A.Peripherally Acting COUGH MEDICATIONS Non-specific or Suppressant Therapy: Refer to drugs that modify the excitability of the cough receptors. Usually non-sedating. Involves the suppression of pulmonary afferent activity.
1. Antihistamines Examples: Diphenhydramine HCl, Fenspiride Proposed MOA: - may have an indirect effect on the cough mechanism, it may reduce postnasal drip which can precipitate cough - H1 antagonists - inhibit mast cell release of Histamine and other inflammatory mediators First generation: More sedating, more anticholinergic activity
Examples: Potassium Cl, Ammonium Cl, Syrup of Ipecac, Glyceryl guaiacolate Proposed MOA: - may lead to more coughing - may alter the physicochemical properties of mucus or its secretion rate. - may also have an effect on the chemotactic trigger zone in the midbrain 3. Mucolytics Examples: Acetylcysteine,Carboxymethylc ysteine, Bromhexine, Ambroxol HCl, Erdosteine MOA: breaks disulfide bonds that hold mucus together thus facilitating easier expulsion. Precautions: in treating bronchospasms, in patients with other underlying problems i.e. peptic ulcers and esophagel varices 4. Bronchodilators Examples: Ephedrine, Theophylline, Terbutaline Role in cough suppression in the absence of asthma conflicting results in studies done. The use of anti asthmatic drugs to treat cough in the absence of asthma is not recommended
Second generation: Less sedating owing in part to lesser distribution in the CNS and little or no anticholinergic activity
Possible MOA : ? Reduce input from stretch receptors and cause bronchodilation even in normal airways ? May alter mucociliary clearance 2. Expectorants 5. Demulcents
Examples: Syrup of Acacia, Glycerin, Licorice (glycyrrhizin), Honey, Olive Oil Proposed MOA: -the sugar in the cough mixture encourages saliva production swallowing may interfere with the cough reflex - the sugar solution may coat the sensory nerve endings in the epipharynx which may result in cough suppression - the sugar coating may act as a protective barrier to the sensory receptors that produce cough. 6. Local Anesthetics Examples: Benzocaine, Benzonatate Proposed MOA: - has an effect on unmyelinated and myelinated nerve endings - may remove all protective reflexes and cause bronchoconstriction - may act on the C fibers B.Centrally Acting cough medications Refer to drugs that act on the sensory afferents that control the excitability of the neural elements in the brainstem that produce cough. May be sedating.
they act within the CNS either a direct action on the cough center in the medulla or in the brainstem respiratory center - receptor stimulation may lead to increase mucociliary clearance or decrease mucus production, hence reduce the need for cough 1. Non-narcotic Dextromethorphan Hbr Butamirate citrate Dimethoxanate Pipazethate
DRUG PROTOTYPES GLYCERYL GUAIACOLATE/ GUAIFENESIN: Classification: Expectorant Dose:Adult: 200-400 mg every 4 hr. Max: 2.4 g/day. Child: 6-12 yr: 100-200 mg; 2-6 yr: 50-100 mg; 6 mth-2 yr: 25-50 mg. To be given every 4 hr. Max: 6-12 yr: 1.2 g/day; 2-5 yr: 600 mg/day. MOA: Guaifenesin increases the volume and reduce the viscosity of tenacious sputum and is used as an expectorant for productive cough. PK: Absorption: Well absorbed in the GI tract. Excretion: Urine. Adverse effects: GI discomfort, nausea and vomiting; dizziness, drowsiness, headache; rash; decreased uric acid levels; urinary calculi (large doses).
CLASSIFICATION: 1. Narcotic
Codeine
Acts on sensory nerve endings that produce cough; receptors in the lung, exact location ?
BROMHEXINE Classification: Mucolytic Dose: PO 8-16 mg 3 times/day. Should be taken with food MOA: secretolytic, causes increase in the production of serous mucus in the respiratory tract and makes the phlegm thinner and less sticky. This contributes to a secretomotoric effect: it helps the cilia to transport the phlegm out of the lungs. Adverse effects: GI side effects; headache, dizziness, sweating, skin rashes. Inhalation: Cough or bronchospasm; transient rise in aminotransferase values AMBROXOL HCL Classification: Mucolytic Dose:Adult: 60-120 mg daily, in 2-3 divided doses. Child: <2 yr: 7.5 mg bid; 2-5 yr: 7.5 mg bid/tid; 6-12 yr: 15 mg bid/tid. Taken with food. MOA: a metabolite of bromhexine hence same action Adverse effects: Mild GI effects and allergic reactions. CODEINE Classification: Narcotic, centrally acting Dose: (cough suppression) Adult: 15-30 mg 3-4 times daily. Max: 240 mg/day. Child: 1-5 yr: 3 mg; 5-12 yr: 7.5-15 mg. Doses to be taken 3-4 times daily. Renal impairment: Dose adjustment may be needed. Hepatic impairment: Dose adjustment may be needed. MOA:Codeine provides relief by blocking the ascending pain
pathways by binding to opiate receptors found in the CNS. It also helps suppress cough by direct action in the medulla. Onset: Oral: 0.5-1 hr. IM: 10-30 min. Duration: 4-6 hr. PK: DRUG PROTOTYPES Absorption: Oral and rectal: Adequate. Distribution: Crosses placenta and enters breast milk. Metabolism: Hepatic by O- and Ndemethylation to morphine (active), norcodeine and other metabolites including normorphine and hydrocodone. Excretion: In the urine, mainly as conjugates with glucuronic acid. Plasma half-life: about 3-4 hr. Adverse effects: CNS and respiratory depression, seizures in infants, bradycardia,hypotension, potential for abuse and dependence DEXTROMETORPHAN HYDROBROMIDE Classification & MOA: NonNarcotic, centrally acting Dose: Children 26 yr: 2.57.5 mg q 48 hr or extendedrelease, 15 mg q 12 hr (max: 30 mg/24 hr). 612 yr: 1015 mg q 48 hr, or extended-release, 30 mg bid (max: 60 mg/24 hr). >12 yr and adults: 1030 mg q 48 hr, or extended release, 60 mg bid (max: 120 mg/24 hr).
Adverse effects in OD: N/V, drowsiness, unsteadiness, visual disturbances, difficulty breathing, tachycardia, hallucinations, seizures, coma Indication: Symptomatic relief of cough, best when cough is nonproductive (depresses medullary cough center).
POTENTIAL FUTURE ANTITUSSIVE THERAPIES 1. VR1- Vanilloid Receptor Antagonists Used capsaicin to identify these receptors 2. Selective Opioid Receptor Agonists 3. Opioid like Receptor Agonists Agonists of the -opioid receptor (such as codeine) suppress cough at the expense of adverse effects that may include sedation, respiratory depression, nausea, constipation, and potential for abuse. A more specifically acting agent that could inhibit cough without such undesirable side effects would offer significant benefit over the currently available narcotic antitussive agents
5-Hydroxytryptamine (5-HT) has been demonstrated to suppress experimentally induced cough in healthy volunteers CalciumChannel
6. Large-Conductance Activated Potassium Openers
Animal studies have demonstrated that the modulation of potassium channels can inhibit experimentally induced cough Further elucidation of the role of potassium channels in pathologic cough may yield effective therapeutic agents in the future.
4. Tachynin Receptor Antagonists In human airways, inflammatory cells appear to be the major source of tachykinins, which include various neuropeptide transmitters such as substance P, neurokinin (NK) A, NKB, and calcitonin gene-related peptide. Animal studies have suggested that tachykinins, through stimulation of three receptor subtypes (ie, NK1, NK2, and NK3), induce neurogenic inflammation, bronchial hyperresponsiveness,and cough.
NOTE: Multiple studies have shown that antitussive therapy is highly successful if aimed at specific etiologies of cough. In cases wherein there is a need for non-specific therapy, such as in chronic unexplained cough, current antitussive therapy may be inadequate or have unacceptable side effects.
Antagonists of the three NK receptor subtypes have been isolated and have demonstrated antitussive activity in animal studies. 5. 5-Hydroxytryptamine Receptor Agonist
___________end of transcription____________ The only way of finding the limits of the possible is by going beyond them into the impossible.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- DR - Cantor's Longevity DietDocument248 pagesDR - Cantor's Longevity DietKenyaReyes67% (3)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Test Bank For Therapeutic Exercise Foundations and Techniques 6th Edition by KisnerDocument6 pagesTest Bank For Therapeutic Exercise Foundations and Techniques 6th Edition by Kisnera33085258962% (13)
- Internet Book of Critical Care (IBCC) : Rapid ReferenceDocument1 pageInternet Book of Critical Care (IBCC) : Rapid Referenceian porterNo ratings yet
- Dermatologic and Cosmetic SurgeryDocument77 pagesDermatologic and Cosmetic SurgeryDr.Tawheed100% (3)
- Infectious DermatologyDocument206 pagesInfectious DermatologyAaron Christian Earl VillosoNo ratings yet
- HANDOUT 3Y Inflammatory Dermatoses 5-28-2012Document23 pagesHANDOUT 3Y Inflammatory Dermatoses 5-28-2012Monica ArmonioNo ratings yet
- Anatomy, Urticaria and Angioedema Reactions To Drugs, SJS-TEN HandoutDocument12 pagesAnatomy, Urticaria and Angioedema Reactions To Drugs, SJS-TEN HandoutAaron Christian Earl VillosoNo ratings yet
- SURGERY Tranx InjuryDocument17 pagesSURGERY Tranx InjuryAaron Christian Earl VillosoNo ratings yet
- Cutaneous Manifestations in Systemic DiseasesDocument10 pagesCutaneous Manifestations in Systemic DiseasesAaron Christian Earl VillosoNo ratings yet
- Patho Respi - 1 TranxDocument15 pagesPatho Respi - 1 TranxAaron Christian Earl VillosoNo ratings yet
- Amebicidal DrugsDocument8 pagesAmebicidal DrugsAaron Christian Earl VillosoNo ratings yet
- Cardiac PathologyDocument15 pagesCardiac PathologyAaron Christian Earl Villoso100% (1)
- Healing and Wound Care Surgery 2Document12 pagesHealing and Wound Care Surgery 2Aaron Christian Earl VillosoNo ratings yet
- Screening of C-Dna Library Using Colony PCRDocument7 pagesScreening of C-Dna Library Using Colony PCRIJAR JOURNALNo ratings yet
- Prevent HIV TransmissionDocument6 pagesPrevent HIV TransmissionHazel EstayanNo ratings yet
- The Promise of Energy Medicine (1984)Document2 pagesThe Promise of Energy Medicine (1984)Regular BookshelfNo ratings yet
- Pulp CappingDocument3 pagesPulp CappingMeta Anjany FirmansyahNo ratings yet
- IBD MedicationDocument19 pagesIBD MedicationTheghanNo ratings yet
- 10 DOH Approved Herbal Medicine: Prepared By: Washington, Luis D. Student Nurse BSN 2H-DDocument11 pages10 DOH Approved Herbal Medicine: Prepared By: Washington, Luis D. Student Nurse BSN 2H-DLuis WashingtonNo ratings yet
- Influenza: CausesDocument2 pagesInfluenza: CausesMaui ShihtzuNo ratings yet
- Types of Feeding TubesDocument8 pagesTypes of Feeding TubesElda KuizonNo ratings yet
- Hipospadia, PPT Blok 3.1 (English)Document11 pagesHipospadia, PPT Blok 3.1 (English)weniNo ratings yet
- Dasar Dasar VirologiDocument28 pagesDasar Dasar Virologiiif adwiyatu iffaNo ratings yet
- A Concise Review On Nerium Oleander L.Document5 pagesA Concise Review On Nerium Oleander L.tatralor100% (1)
- Nursing Care of Clients Undergoing Eye SurgeryDocument1 pageNursing Care of Clients Undergoing Eye SurgerySewyel GarburiNo ratings yet
- Coronavirus British English Intermediate b1 b2 GroupDocument4 pagesCoronavirus British English Intermediate b1 b2 GroupAngel AnitaNo ratings yet
- Health and Social Care Inequalities: The Impact of COVID-19 On People Experiencing Homelessness in BrazilDocument13 pagesHealth and Social Care Inequalities: The Impact of COVID-19 On People Experiencing Homelessness in BrazilcinacchiNo ratings yet
- U BDocument7 pagesU Bapi-3809387No ratings yet
- Nina Rajan Pillai & Ors. Vs Union of India and Ors. On 13 May, 2011Document33 pagesNina Rajan Pillai & Ors. Vs Union of India and Ors. On 13 May, 2011Sanjayan KizhakkedathuNo ratings yet
- Allele-specific expression of variant-specific surface proteins in Giardia lambliaDocument7 pagesAllele-specific expression of variant-specific surface proteins in Giardia lambliawiwienNo ratings yet
- Biology 10Th Edition Raven Test Bank Full Chapter PDFDocument36 pagesBiology 10Th Edition Raven Test Bank Full Chapter PDFlewis.barnes1000100% (12)
- Organ Transplantatio1Document26 pagesOrgan Transplantatio1Bindashboy0No ratings yet
- ShaylaDocument3 pagesShaylaapi-530728661No ratings yet
- Physiology TestDocument10 pagesPhysiology TestGanta ChaitanyaNo ratings yet
- TRIUMPHANT COLLEGE COVID-19 TRAINING NewDocument26 pagesTRIUMPHANT COLLEGE COVID-19 TRAINING NewDaniellaNo ratings yet
- Dengue AccomplishmentDocument4 pagesDengue AccomplishmentKylie GolindangNo ratings yet
- Basic Haematology Exercise 1 (MKEB2403)Document10 pagesBasic Haematology Exercise 1 (MKEB2403)kiedd_04100% (8)
- Target Client List For NCD Prevention and Control SERVICES (Part 1)Document9 pagesTarget Client List For NCD Prevention and Control SERVICES (Part 1)Lchg KrvyNo ratings yet
- Heart Disease Diagnosis System Based On Multi-Layer Perceptron Neural Network and Support Vector MachineDocument13 pagesHeart Disease Diagnosis System Based On Multi-Layer Perceptron Neural Network and Support Vector MachineshahadNo ratings yet