Professional Documents
Culture Documents
Ischiococcygeus Muscle
Uploaded by
mcwnotesOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ischiococcygeus Muscle
Uploaded by
mcwnotesCopyright:
Available Formats
Clinical Human Anatomy
Class of 2009 Coop
November 14, 2005
Lecturer: Dr. Kuhlmann
Pelvis and Perineum 1
Dr. Kuhlmann began by asking us to use the notes as an outline and listen to the lecture.
His lecture contained slides that were either from old Netter editions or other textbooks.
He said that he would start each class with a review of the previous lecture then end with
a clinical correlation. Also, he said that he would be in the inner lab to discuss the
prosections of the pelvis. This Coop contains portions of the 2007 Coop with additions.
Bony Pelvis [Netter 240,468,340]
The bony pelvis is made up of 4 bones: the sacrum (S1-S5), coccyx, and (2) innominate
(ox coxal or hip bone). The hip bone is made up of the ilium, ischium, and pubic bone.
Spaces and planes [Netter 340]
1) true pelvis - below the iliopectineal line which contains and protects the lower portion
of the GI, GU(genitourinary), and internal reproductive organs.
2) false pelvis - above the iliopectineal line. little clinical importance.
Look down into the pelvis: the portion of the pelvis below the "ring" is the true pelvis,
that portion on top is the false pelvis.
Ligaments [Netter 340]
The sacrospinous ligament and sacrotuberous ligament form the greater sciatic
foramen and lesser sciatic foramen. The sacrospinous sacrospinous ligament and
sacrotuberous ligament and sacrotuberous ligament also prevent rotation of the
sacrum as this supports the weight of the vertebral column. The obturator canal or space
is formed by the obturator membrane in the obturator foramen. The obturator nerve,
artery, and vein pass through the obturator canal.
Pelvic planes [Netter 342]
The plane of the pelvic inlet is a plane drawn from the tip of the sacral promontory to
the superior edge of the pubic symphysis. The plane of the pelvic outlet is a plane drawn
from the end of S5 to the inferior edge of the pubic symphysis. These two planes are
measured (obstetrical conjugate) to determine the type of pelvis a woman has and to see
if it is adequate for delivering a child.
Sex differences [Netter 342]
The male pubic arch is less than 90 degrees, while the female pubic arch is greater
than 90 degrees. Dr. Kuhlmann also said if you were to pour cement into the pelvis, you
would see the male pelvis cause the flows to converge, while in the female pelvis flows
would diverge.
Muscular Pelvis [Netter 343-346]
1) The pelvic diaphragm creates two spaces: the intra-pelvic (visceral) and the
ischiorectal space.
A. The intra-pelvic (visceral) space is superior to the pelvic diaphragm. The
ischiorectal space (fossa) is inferior to the pelvic diaphragm and posterior to the
urogenital diaphragm. The ischiorectal fossa is filled with fat and covered by the
gluteus maximus muscles.
B. Muscles of the pelvic diaphragm are the levator ani muscles and
ischiococcygeus (coccygeus) muscle.
1. Levator ani muscles are the main part of the pelvic diaphragm.
a. Puborectalis m.: forms a sling, important for maintaining rectal
continence
b. Pubococcygeus m.: main part of levator ani
c. Iliococcygeus m.
(Innervation to the levator ani is from the perineal branches of the third and
fourth sacral nerves.)
2. Ischiococcygeus muscle (Innervation from S4,5)
Note: The pelvic diaphragm constitutes the main support for the pelvic
viscera.
2) Piriformis muscle – this muscle is adjacent to the ischiococcygeus muscle, but is
NOT part of the pelvic diaphragm
3) The Urogenital Diaphragm (UG diaphragm, aka deep pouch or deep space)
The UG diaphragm fills a defect in the pelvic diaphragm.
Fascia of the UG diaphragm is composed of two layers
a. the superior fascia
b. the inferior fascia, also know as the perineal membrane
Note: Anything inferior to the inferior fascia is in the Superficial Pouch.
Muscles of the UG Diaphragm are between these two fascial layers
a. the sphincter urethra muscle
b. the deep transverse perineal muscle
Note: The urethra and vagina (in females) pass through the UG
diaphragm. The rectum does NOT pierce the UG diaphragm.
4) The Superficial Space (Pouch) is composed of:
a. Ischiocavernosus muscles (two)
b. Bulbocavernosus muscles (or bulbospongiosus) (two)
c. Superficial transverse perineal muscles (two)
d. Branches of the pudendal nerve and vessels
And in females only:
e. Vestibular bulb- highly vascularized and extremely vulnerable to traumatic injury
(straddle injury, for example)
f. Bartholin gland a.k.a. Greater Vestibular Gland (two).
Note: The superficial space is continuous with the anterior abdominal wall because
the inferior fascia is continuous with Scarpa’s fascia.
Practice Exam Question:
A four-year old girl fell on a fence, sustaining a “straddle” injury. A large hematoma is noted involving
her perineum; within 12 hrs. her lower abdominal wall becomes “bluish” to the level of her umbilicus.
Which of the following is true concerning the “superficial pouch”?
1. it contains the external iliac artery
2. it is continuous with Scarpa’s fascia of the anterior abdominal wall
3. it contains the sphincter urethrae muscle
4. it contains the femoral nerve
(answer at end of COOP)
5) The deep pouch is enclosed by the superior and inferior fascias of the UG
diaphragm.
In males, the deep pouch contains:
a) membranous urethra
b) sphincter urethra
c) bulbourethral gland’s (Cowper’s)
d) deep transverse perineal muscle
In females, the deep pouch contains:
a) urethra
b) sphincter urethral muscle
c) inferior vagina
d) deep transverse perineal muscle
The Neural Pelvis [Netter 389-391 male, 393 female]
1) Obturator nerve (know the course of the nerve)
* This nerve originates from L2-L4 and accompanies the obturator artery and
vein. It runs along the superior pelvic aperture, crosses the sacroiliac joint and
passes through the obturator canal, sending branches to the Obturator internus
muscle and the Adductor muscles of the thigh.
2) Lumbosacral trunk
* L4-L5, joins up with S1-S3.
3) Sacral Plexus
* Consists of: The lumbosacral trunk (L4-L5) and S1-S4.
Includes the Pudendal n., Sciatic n., Superior Gluteal n., among others.
4) Sciatic nerve
* L4-S3
* Will be discussed in greater detail in gluteal region.
* Passes through the Greater Sciatic foramen.
5) Pudendal nerve (Know the course) [Netter 391, 393]
* S2, 3, 4
* Exits at greater sacrosciatic foramen, re-enters the pelvis through the lesser
sacrosciatic foramen, and travels through the pudendal canal. Visualized best in
the gluteal region.
* Branches include:
1. Inferior rectal n.—to the anal region
2. Deep perineal n.
3. Deep Branches to the urogenital diaphragm, which terminates as the
Dorsal nerve of the penis/clitoris.
4. Posterior femoral cutaneous n. of the thigh and ilioinguinal region.
Vast majority of innervation of perineum is from Pudendal Nerve.
Vasculature of the Pelvis [Netter 378-385]
The common iliac artery branches into Internal and External Iliac arteries.
Branches of Internal Iliac artery [Netter 382-383]:
1. Anterior Division
a) Umbilical artery
* Gives rise to superior vesicular branches which supply the bladder; later
obliterates and runs along the anterior abdominal wall as the umbilical ligament.
b) Obturator A.
* can come off the umbilical artery or directly off of the internal iliac artery.
c) Internal Pudendal A.
d) Inferior Gluteal A.
e) Middle Rectal A.
f) Uterine and vaginal artery
2. Posterior Division (just remember these 3, any others are part of the anterior division)
a) Iliolumbar A.
b) Lateral sacral A.
c) Superior gluteal A.
Know the relationship between the ureter and the uterine artery. The ureter passes
under the artery, as emphasized many times: “Water (ureter) runs under the bridge
(uterine artery).”
Blood supply of the ureter:
abdominal—medial to lateral supply—renal branches
pelvis – lateral to medial supply – internal iliac artery, then vesicular, uterine,
vaginal branches.
Dr. Bolender concluded the lecture with tips for the pelvis dissection. He said to follow
c.12 in the dissection guide.
1. remove the skin to reveal the gluteus maximus
2. cut the gluteus maximus away from the sacrotuberous ligament, but don't cut the
ligament.
3. the ischiorectal fossae is between the ischial tuberosity and the coccyx
4. the pudendal n.,a.,v. run together leaving the greater sacrosciatic foramen and entering
the lesser sacrosciatic foramen..
5. insert a tampon into the anus to give support during the dissection.
Answer to practice question: (2)
You might also like
- Practices of Anorectal SurgeryFrom EverandPractices of Anorectal SurgeryDong Keun LeeNo ratings yet
- PELVISDocument68 pagesPELVISDevsya DodiaNo ratings yet
- 2 B Anterior Abdominal Wall and StomachDocument29 pages2 B Anterior Abdominal Wall and StomachArif NabeelNo ratings yet
- Thoracic and Coracoid Arteries In Two Families of Birds, Columbidae and HirundinidaeFrom EverandThoracic and Coracoid Arteries In Two Families of Birds, Columbidae and HirundinidaeNo ratings yet
- Anatomy and Physiology Questions from AIIMS May 2015 ExamDocument33 pagesAnatomy and Physiology Questions from AIIMS May 2015 ExamScribbleCoolioNo ratings yet
- A Simple Guide to the Voice Box and Its Disorders, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to the Voice Box and Its Disorders, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Pelvic Cavity PDFDocument10 pagesPelvic Cavity PDFRigor MortisNo ratings yet
- Maternal Anatomy WilliamsDocument52 pagesMaternal Anatomy WilliamsMariane Tejano100% (1)
- Os Complete Final AnswerDocument198 pagesOs Complete Final AnswerDeshini Balasubramaniam100% (4)
- A New Order of Fishlike Amphibia From the Pennsylvanian of KansasFrom EverandA New Order of Fishlike Amphibia From the Pennsylvanian of KansasNo ratings yet
- 1 4899983447608524847Document113 pages1 4899983447608524847berlianroma100% (1)
- A Guide for the Dissection of the Dogfish (Squalus Acanthias)From EverandA Guide for the Dissection of the Dogfish (Squalus Acanthias)No ratings yet
- Epidural AnaesthesiaDocument99 pagesEpidural AnaesthesiaabhinavguttikondaNo ratings yet
- GRDA Intro Bony PelvisDocument5 pagesGRDA Intro Bony PelvisKingNo ratings yet
- PerineumDocument4 pagesPerineumwiwin09No ratings yet
- LG 3 (Abdominal Wall Muscles and Inguinal Canal)Document33 pagesLG 3 (Abdominal Wall Muscles and Inguinal Canal)allanNo ratings yet
- Anterior Abdominal WallDocument108 pagesAnterior Abdominal WallMunikrishna Salavakam100% (1)
- Pelvic Musculature and Perineum AnatomyDocument29 pagesPelvic Musculature and Perineum AnatomyNatyra RaniNo ratings yet
- 4 Pectoral RegionDocument62 pages4 Pectoral RegionFarrukh ShahzadNo ratings yet
- Anatomy of The Female Reproductive SystemDocument62 pagesAnatomy of The Female Reproductive SystemBibek GajmerNo ratings yet
- Pelvic and PerineumDocument20 pagesPelvic and PerineumRahaf MajadlyNo ratings yet
- Practical Class - Week 12: Abdominal Walls, GI Tract, Reproductive & Urinary SystemsDocument8 pagesPractical Class - Week 12: Abdominal Walls, GI Tract, Reproductive & Urinary SystemskevNo ratings yet
- Anat 5.2 Pelvis and Perineum - ElevazoDocument14 pagesAnat 5.2 Pelvis and Perineum - Elevazolovelots1234No ratings yet
- PELVIS, Student FileDocument52 pagesPELVIS, Student FileShawn Gaurav JhaNo ratings yet
- Pectoral Region & BreastDocument52 pagesPectoral Region & BreastemanNo ratings yet
- Material Mini NetterDocument11 pagesMaterial Mini NetterVALENTINA ALBORNOZ BASTÍASNo ratings yet
- Anatomy of the Human Reproductive SystemDocument18 pagesAnatomy of the Human Reproductive SystemNindy TjionganataNo ratings yet
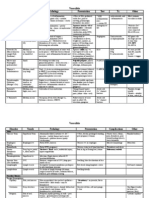
- Muscle Origin Insertion Innervation ActionDocument6 pagesMuscle Origin Insertion Innervation ActionmcwnotesNo ratings yet
- The PerineumDocument3 pagesThe PerineumSanjay KishoreNo ratings yet
- Pelvis and PerineumDocument5 pagesPelvis and PerineumK ZarabianNo ratings yet
- Anatomy & Embryology of The Female Genital SystemDocument86 pagesAnatomy & Embryology of The Female Genital SystemyazNo ratings yet
- Question No 01: PART A) Define Pelvis?Document5 pagesQuestion No 01: PART A) Define Pelvis?aminaNo ratings yet
- Ob 1 1Document73 pagesOb 1 1Kate GuzmanNo ratings yet
- Review of Anatomy and Physiology of Human ReproductiveDocument68 pagesReview of Anatomy and Physiology of Human Reproductivesavita hanamsagarNo ratings yet
- PELVIC FRACTURE: ANATOMY AND INNERVATIONDocument22 pagesPELVIC FRACTURE: ANATOMY AND INNERVATIONAgeng BudianantiNo ratings yet
- Abdominal Walls: You Must Know The Following StructuresDocument12 pagesAbdominal Walls: You Must Know The Following StructuressamNo ratings yet
- Upper Limp Questions (ANSWERED)Document57 pagesUpper Limp Questions (ANSWERED)kazelio2017No ratings yet
- Dissector Answers - Deep Back & Spinal CordDocument9 pagesDissector Answers - Deep Back & Spinal CordUloko ChristopherNo ratings yet
- 1 s2.0 S0039610905704084 MainDocument25 pages1 s2.0 S0039610905704084 Mainjuan pablo mesa mejiaNo ratings yet
- Anterior Abdominal WallDocument22 pagesAnterior Abdominal WallBhavana VallakattiNo ratings yet
- General Zoology Muscular System of The Frog - NotesDocument15 pagesGeneral Zoology Muscular System of The Frog - NotesMarian CordanoNo ratings yet
- NeckDocument215 pagesNeckpilot abdi baariNo ratings yet
- Dinding Abdomen PSIKDocument79 pagesDinding Abdomen PSIKSondang DamanikNo ratings yet
- Anatomy and Physiology of Pregnancy Part 1Document37 pagesAnatomy and Physiology of Pregnancy Part 1Umer RafiqNo ratings yet
- Inguinal Canal and ScrotumDocument55 pagesInguinal Canal and ScrotumAuza Moses IbrahimNo ratings yet
- Pelvis Slide 5-7 Complete)Document23 pagesPelvis Slide 5-7 Complete)Joseph EstradaNo ratings yet
- Hernia and HydrocoeleDocument3 pagesHernia and HydrocoeleDr.Biswajit jenaNo ratings yet
- Anatomy of Larynx Lecture 7Document21 pagesAnatomy of Larynx Lecture 7sallykamareddine100% (1)
- LAB Anterior Abdominal Wall & Inguinal RegionDocument12 pagesLAB Anterior Abdominal Wall & Inguinal RegionnanaNo ratings yet
- Abdomen 2023Document131 pagesAbdomen 2023Fenot YBNo ratings yet
- CBL 2Document20 pagesCBL 2Hammad AkramNo ratings yet
- Abdominal HerniasDocument38 pagesAbdominal HerniasHafizah HoshniNo ratings yet
- Aiims May 2009Document50 pagesAiims May 2009Gowri ShankarNo ratings yet
- Abdominal anatomy notes on inguinal herniasDocument39 pagesAbdominal anatomy notes on inguinal herniasJoseph KimNo ratings yet
- Perineal TearsDocument49 pagesPerineal TearsvisakhaNo ratings yet
- Medial Side of ThighDocument29 pagesMedial Side of ThighAnnapurna BoseNo ratings yet
- Anatomy of Female Genital OrgansDocument7 pagesAnatomy of Female Genital OrgansAyurveda PgNo ratings yet
- Humerus Arm Anatomical Neck ArmDocument41 pagesHumerus Arm Anatomical Neck ArmmcwnotesNo ratings yet
- Humerus Arm Anatomical Neck ArmDocument41 pagesHumerus Arm Anatomical Neck ArmmcwnotesNo ratings yet
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- NullDocument53 pagesNullmcwnotesNo ratings yet
- Cytokines: Cytokine Source Target/Effect OtherDocument1 pageCytokines: Cytokine Source Target/Effect OthermcwnotesNo ratings yet
- Surface Molecules: Molecule Location Ligand Action OtherDocument1 pageSurface Molecules: Molecule Location Ligand Action OthermcwnotesNo ratings yet
- Antibodies: Type Response Action Other Hypersensitivity TypeDocument2 pagesAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesNo ratings yet
- Cytokines: Cytokine Source Target/Effect OtherDocument1 pageCytokines: Cytokine Source Target/Effect OthermcwnotesNo ratings yet
- Hypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesDocument1 pageHypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesmcwnotesNo ratings yet
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- Surface Molecules: Molecule Location Ligand Action OtherDocument1 pageSurface Molecules: Molecule Location Ligand Action OthermcwnotesNo ratings yet
- Antibodies: Type Response Action Other Hypersensitivity TypeDocument2 pagesAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesNo ratings yet
- NullDocument4 pagesNullmcwnotesNo ratings yet
- Disorder Hyperprolactinema Adrenal Insufficiency 1° (Addison's) FSH, LHDocument2 pagesDisorder Hyperprolactinema Adrenal Insufficiency 1° (Addison's) FSH, LHmcwnotesNo ratings yet
- Hormone Thyroid T3, T4 Target Nuclear Receptors Of: MostDocument3 pagesHormone Thyroid T3, T4 Target Nuclear Receptors Of: MostmcwnotesNo ratings yet
- Organ Hypothalamus Anterior Pituitary Posterior Pituitary Pineal Thyroid ParathyroidDocument1 pageOrgan Hypothalamus Anterior Pituitary Posterior Pituitary Pineal Thyroid ParathyroidmcwnotesNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- NullDocument2 pagesNullmcwnotesNo ratings yet
- People That Meet Clinical Criterion Synonymous DifferencesDocument2 pagesPeople That Meet Clinical Criterion Synonymous DifferencesmcwnotesNo ratings yet
- Changes With Aging Characteristic CV TPR Blood Vessels Renin-AngiotensinDocument2 pagesChanges With Aging Characteristic CV TPR Blood Vessels Renin-AngiotensinmcwnotesNo ratings yet
- Maternal Changes During Pregnancy System Pituitary Hormone/ Parameter GHDocument1 pageMaternal Changes During Pregnancy System Pituitary Hormone/ Parameter GHmcwnotesNo ratings yet
- Adenohypophysis Cell Type Somatotrophs (GH/Prolactin Family) Product GH (Somatotrophin)Document2 pagesAdenohypophysis Cell Type Somatotrophs (GH/Prolactin Family) Product GH (Somatotrophin)mcwnotesNo ratings yet
- Prevalence The Number of Existing Cases in A PopulationDocument5 pagesPrevalence The Number of Existing Cases in A PopulationmcwnotesNo ratings yet
- Hormone Thyroid T3, T4 Target Nuclear Receptors Of: MostDocument2 pagesHormone Thyroid T3, T4 Target Nuclear Receptors Of: MostmcwnotesNo ratings yet
- People That Meet Clinical Criterion Synonymous DifferencesDocument2 pagesPeople That Meet Clinical Criterion Synonymous DifferencesmcwnotesNo ratings yet
- Adenohypophysis Cell Type Somatotrophs (GH/Prolactin Family) Product GH (Somatotrophin)Document2 pagesAdenohypophysis Cell Type Somatotrophs (GH/Prolactin Family) Product GH (Somatotrophin)mcwnotesNo ratings yet
- Male Region Testis Tunica Albuginia Tunica Vasculosa Seminiferous TubuleDocument2 pagesMale Region Testis Tunica Albuginia Tunica Vasculosa Seminiferous TubulemcwnotesNo ratings yet
- Lab 4 Assessment and Analysis of Cardiovascular Function inDocument2 pagesLab 4 Assessment and Analysis of Cardiovascular Function inmcwnotesNo ratings yet
- Lab 3: Computer Simulation of Cardiovascular Dynamics 1. CirculatoryDocument3 pagesLab 3: Computer Simulation of Cardiovascular Dynamics 1. Circulatorymcwnotes100% (1)
- Lab 4 Assessment and Analysis of Cardiovascular Function inDocument2 pagesLab 4 Assessment and Analysis of Cardiovascular Function inmcwnotesNo ratings yet
- JNTUA Mechanical Engineering (R09) Syllabus BookDocument147 pagesJNTUA Mechanical Engineering (R09) Syllabus Bookslv_prasaad0% (1)
- Rostam's Seven LaboursDocument3 pagesRostam's Seven LaboursArifin SohagNo ratings yet
- Year 2 - Push and Pull FPDDocument18 pagesYear 2 - Push and Pull FPDRebecca LNo ratings yet
- RRLDocument4 pagesRRLTiltshifter ViNo ratings yet
- Packetfence Network Devices Configuration Guide: For Version 3.5.0Document76 pagesPacketfence Network Devices Configuration Guide: For Version 3.5.0René FabricioNo ratings yet
- Flow Through Pipes: Departmentofcivilengineering Presidency University, Bangalore-64 BY Santhosh M B Asstistant ProfessorDocument15 pagesFlow Through Pipes: Departmentofcivilengineering Presidency University, Bangalore-64 BY Santhosh M B Asstistant ProfessorSanthoshMBSanthuNo ratings yet
- Manage a micro business with BSB30315Document3 pagesManage a micro business with BSB30315Theo A W JacksonNo ratings yet
- FrankensteinDocument24 pagesFrankensteinLisa WardNo ratings yet
- Upper Six 2013 STPM Physics 2 Trial ExamDocument11 pagesUpper Six 2013 STPM Physics 2 Trial ExamOw Yu Zen100% (2)
- MechanismDocument17 pagesMechanismm_er100No ratings yet
- Communication & Collaboration: Lucy Borrego Leidy Hinojosa Scarlett DragustinovisDocument44 pagesCommunication & Collaboration: Lucy Borrego Leidy Hinojosa Scarlett DragustinovisTeacherlucy BorregoNo ratings yet
- Vee 2003Document14 pagesVee 2003Syed faizan Ali zaidiNo ratings yet
- Infineum Ilsa Gf-6 API SP e JasoDocument28 pagesInfineum Ilsa Gf-6 API SP e JasoDanielNo ratings yet
- Causes of The Renaissance: Silk RoadDocument6 pagesCauses of The Renaissance: Silk RoadCyryhl GutlayNo ratings yet
- Booklet English 2016Document17 pagesBooklet English 2016Noranita ZakariaNo ratings yet
- Deconstructing Product Design Exploring The Form, Function, Usability, Sustainability, and Commercial Success of 100 Amazing Products PDFDocument100 pagesDeconstructing Product Design Exploring The Form, Function, Usability, Sustainability, and Commercial Success of 100 Amazing Products PDFMontserrat CifuentesNo ratings yet
- Percentage Practice Sheet - RBEDocument11 pagesPercentage Practice Sheet - RBEankitNo ratings yet
- 3.5 Lonaphala S A3.99 PiyaDocument9 pages3.5 Lonaphala S A3.99 PiyaPiya_TanNo ratings yet
- Volume 4-6Document757 pagesVolume 4-6AKNo ratings yet
- Health Benefits of Kidney BeansDocument17 pagesHealth Benefits of Kidney BeansShyneAneeshNo ratings yet
- ClarifierDocument2 pagesClarifierchagar_harshNo ratings yet
- Mobile-Friendly Cooperative WebDocument7 pagesMobile-Friendly Cooperative WebWahyu PNo ratings yet
- Paper23 PGDMM Public Procurement MCQ Sept2021Document25 pagesPaper23 PGDMM Public Procurement MCQ Sept2021Gagan VermaNo ratings yet
- Plano Electrico 785CDocument2 pagesPlano Electrico 785CLuis MartínezNo ratings yet
- Palo Alto Firewall VirtualizationDocument394 pagesPalo Alto Firewall VirtualizationRyanb378No ratings yet
- Avance Collection Mixer Grinder SpecsDocument3 pagesAvance Collection Mixer Grinder SpecsfaNo ratings yet
- Newly Constructed Masculinity' in Mahesh Dattani's Dance Like A ManDocument4 pagesNewly Constructed Masculinity' in Mahesh Dattani's Dance Like A ManIJELS Research JournalNo ratings yet
- Catalogue PDFDocument4 pagesCatalogue PDFShivam GuptaNo ratings yet
- Comandos HuaweiDocument3 pagesComandos Huaweicgottoli0% (1)
- Hall Design For SpeechDocument1 pageHall Design For SpeechSarovar SaroNo ratings yet
- The Yogi Code: Seven Universal Laws of Infinite SuccessFrom EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessRating: 4.5 out of 5 stars4.5/5 (104)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingFrom EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingRating: 4.5 out of 5 stars4.5/5 (66)
- Relentless: From Good to Great to UnstoppableFrom EverandRelentless: From Good to Great to UnstoppableRating: 5 out of 5 stars5/5 (779)
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindFrom EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindRating: 4.5 out of 5 stars4.5/5 (1)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerFrom EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerRating: 4 out of 5 stars4/5 (5)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (110)
- Wall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesFrom EverandWall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesNo ratings yet
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsFrom EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsRating: 5 out of 5 stars5/5 (95)
- Chakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.From EverandChakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.Rating: 4 out of 5 stars4/5 (2)
- The Strength and Conditioning Bible: How to Train Like an AthleteFrom EverandThe Strength and Conditioning Bible: How to Train Like an AthleteNo ratings yet
- Meat Is for Pussies: A How-To Guide for Dudes Who Want to Get Fit, Kick Ass, and Take NamesFrom EverandMeat Is for Pussies: A How-To Guide for Dudes Who Want to Get Fit, Kick Ass, and Take NamesRating: 3.5 out of 5 stars3.5/5 (8)
- How Bad Do You Want It?: Mastering the Pshchology of Mind over MuscleFrom EverandHow Bad Do You Want It?: Mastering the Pshchology of Mind over MuscleRating: 4.5 out of 5 stars4.5/5 (127)
- The Art of Impossible: A Peak Performance PrimerFrom EverandThe Art of Impossible: A Peak Performance PrimerRating: 5 out of 5 stars5/5 (230)
- If You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsFrom EverandIf You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsRating: 4.5 out of 5 stars4.5/5 (7)
- Calisthenics: Guide for Bodyweight Exercise, Build your Dream Body in 30 MinutesFrom EverandCalisthenics: Guide for Bodyweight Exercise, Build your Dream Body in 30 MinutesRating: 3 out of 5 stars3/5 (5)
- 5-Minute Yoga: A More Energetic, Focused, and Balanced You in Just 5 Minutes a DayFrom Everand5-Minute Yoga: A More Energetic, Focused, and Balanced You in Just 5 Minutes a DayRating: 5 out of 5 stars5/5 (1)
- Wheels of Life: A User's Guide to the Chakra SystemFrom EverandWheels of Life: A User's Guide to the Chakra SystemRating: 4.5 out of 5 stars4.5/5 (33)
- Roxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingFrom EverandRoxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingRating: 4.5 out of 5 stars4.5/5 (18)
- Roxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingFrom EverandRoxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingRating: 4.5 out of 5 stars4.5/5 (130)
- The Swing!: Lose the Fat and Get Fit with This Revolutionary Kettlebell ProgramFrom EverandThe Swing!: Lose the Fat and Get Fit with This Revolutionary Kettlebell ProgramNo ratings yet
- Light on Yoga: The Definitive Guide to Yoga PracticeFrom EverandLight on Yoga: The Definitive Guide to Yoga PracticeRating: 5 out of 5 stars5/5 (1)
- Calisthenics: 12 Effective Exercises to Build Calisthenics Body in 14 DaysFrom EverandCalisthenics: 12 Effective Exercises to Build Calisthenics Body in 14 DaysRating: 3 out of 5 stars3/5 (5)
- ROAR: How to Match Your Food and Fitness to Your Unique Female Physiology for Optimum Performance, Great Health, and a Strong, Lean Body for LifeFrom EverandROAR: How to Match Your Food and Fitness to Your Unique Female Physiology for Optimum Performance, Great Health, and a Strong, Lean Body for LifeRating: 4.5 out of 5 stars4.5/5 (44)
- Applied Polyvagal Theory in Yoga: Therapeutic Practices for Emotional HealthFrom EverandApplied Polyvagal Theory in Yoga: Therapeutic Practices for Emotional HealthNo ratings yet
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!From EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Rating: 4.5 out of 5 stars4.5/5 (22)