Professional Documents
Culture Documents
Practical 1a
Uploaded by
Maisarah Ab SamadOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Practical 1a
Uploaded by
Maisarah Ab SamadCopyright:
Available Formats
SCHOOL OF HEALTH SCIENCES 2011/2012
GTU 310 CLINICAL BIOCHEMISTRY PRACTICAL 1 6 MARCH 2012
Estimation of Albumin by Bromocresol green (BCG) Dye Method Estimation of Total Protein by Biuret Method Separation of Serum Proteins by Electrophoresis NAME: MAISARAH AB SAMAD MATRIC NUMBER: 105105 GROUP: 6 PROGRAM: BIOMEDICINE 3 LECTURERS NAME: DR YUSMAZURA BT ZAKARIA
PRACTICAL 1A: ESTIMATION OF ALBUMIN BY BROMOCRESOL GREEN (BCG) DYE METHOD OBJECTIVE 1. To estimate the albumin in serum by BCG Dye method 2. To record the optical density (absorbance) using the calorimeter and calculate the concentration of the test sample from the formula. INTRODUCTION Serum proteins are proteins found in blood plasma. Albumin consists of approximately 60% of the total proteins in the body while the other major part consists of globulin. Albumin is synthesized in the liver and it is made up only of amino acids, without prosthetic groups or other additives. Albumin is essential for maintaining the osmotic pressure by regulating the blood oncotic pressure. A balance osmotic pressure is needed for proper distribution of body fluids between intravascular compartments and body tissues. Besides that, it also acts as a plasma carrier by non-specifically binding
several hydrophobic steroid hormones and as a transport protein for hemin and fatty acids. It acts as carrier for many cations and water insoluble substances, like calcium and bilirubin. Hypoalbuminemia is often associated with liver diseases, malnutrition or malabsorption, burns or dermatitis, kidney and intestinal diseases. Hyperalbuminemia is rarely seen and is usually associated with dehydration. Bromocresol green (BCG) dye method is a method to determine albumin in serum or plasma. Albumin will bind with the dye Bromocresol Green in buffered medium at pH 4.2 to form a green coloured complex. The intensity of the colour of the resulting albumin-BCG complex is directly proportional to the amount of albumin present in the sample.
PROTOCOL Reagents and Apparatus: 1. Standard (Human serum albumin); Concentration: 46.75 g/L 2. BCG reagent; contain bromocresol green dye, succinate buffer pH 4.2, Brij-35 3. Pipettes 4. Spectrophotometer 5. Cuvetts 6. Vortex
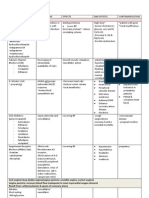
Procedure: The protocol of the procedure is described below. 1. The test tubes were labeled as B for Blank, S1 for standard and T1, T2 and QC for Test samples. 2. 3.0 ml of BCG reagent was added into each tube. 3. A micropipette was used to add 10l of standard and test sample to the corresponding test tubes. 10l of distilled water was added in Blank. 4. The tubes were mixed gently using a vortex and the tubes incubated at room temperature for 5 minutes. 5. The samples were read at 630nm against the blanks using a spectrophotometer. 6. The concentration of the albumin present in the given test sample was calculated using the formula Concentration of Albumin in sample = Atest/QC Astandard RESULT Blank Standard Test (T1) Test (T2) Q.C X Concstd
1 Optical density
0.520
0.487
0.422
0.501
0.519
0.484
0.423
0.503
Average Concentration of albumin (g/L)
0.5195
0.486
0.4225
0.502
46.75
43.69
37.98
45.18
Concentration range of QC: 38.7 61.9 g/L
DISCUSSION The normal range of serum albumin is 35g/L to 50g/L. Based on the result above, the concentration of the standard is 46.75 g/L, for T1 and T2; the concentrations are 43.69 g/L and 37.98 g/L respectively. The concentration of QC is 45.18 g/L. Internal QC acts as quality control in determining whether the method is acceptable. The range of concentration of QC is 38.7 to 61.9 g/L. In this practical, the concentration of QC is within the range, thus the concentration of T1 and T2 are acceptable. The concentration of serum albumin in both T1 and T2 are normal. Bromocresol green (BCG) dye-binding method for the quantitative determination of serum-albumin was introduced in 1964 by DELANEY (Proc. Australian Assoc. Clin. Biochem 64 (1964),1). Serum is diluted with buffered BCG at pH 7.0 and the decrease in absorbance at 615 nm is measured. This change in absorbance is linear with albumin concentration up to 50 mg/ml and other electrophoretically separated proteins like hemoglobin and bilirubin do not interfere. This method is quicker compared to Biuret method in analysing the serum protein. However, the measurement if albumin can be limited as it can be interfered by haemolysed and lipaemic sera. Thus, in collecting the specimen, it is important to avoid excessive haemolysis since every 100mg/dl of haemoglobin corresponds to about 100mg/dl of albumin. Abnormality in serum albumin concentration is often associated with clinical significances that lead to hypoalbuminemia and hyperalbuminemia. Hypoalbuminemia or decrease in serum albumin may due to reduced synthesis that caused by malnutriniton, intestinal malabsorption, liver disease, wasting diseases, nephritic syndrome and haemodilution. Hypoalbuminemia is also occurred due to excessive loss caused by nephritic syndrome, massive burns, and protein-losing enteropathy. Severe burns that damage capillaries and blood vessels cause a huge loss of serum proteins. The increased capillary permeability caused by the burn damage allows a continual leakage of serum proteins out of the vascular system. Analbuminaemia is a genetic disease with autosomal recessive inheritence that can lead to near to or absence of albumin. Besides that, serum globulin may decrease due to haemodilution in shock, burns, haemorrhage. Serum globulin increases in multiple myeloma, macroglobulinaemia, chronic liver disease, chronic infections and autoimmune diseases. Increased albumin levels or hyperalbuminemia are generally not observed. A rise in serum albumin may occur in dehydration due to haemoconcentration.
CONCLUSION The intensity of the colour of albumin-BCG complex (green) is directly proportional to the concentration of albumin present in the sample. The concentrations of albumin in both Test samples are within the normal range and there might be no clinical significances associated with the normal concentration.
PRACTICAL 1B: ESTIMATION OF TOTAL PROTEIN BY BIURET METHOD\ OBJECTIVE 1. To estimate the amount of protein present in the Test samples by biuret method. 2. To record the optical density (absorbance) using the calorimeter and calculate the concentration of the test sample from the formula. INTRODUCTION Serum contains a large variety of proteins. Proteins are constituents of muscles, enzymes, hormones and several other key functional and structural entities in the body. The total proteins consist mainly of albumin and the various globulins. Proteins are essential in the maintenance of the normal distribution of water between blood and the tissues.
Biuret method is use to estimate the total protein in serum. Cupric ions form chelates with the peptide bonds of proteins in alkaline medium. A purple complex is formed as the result of coordination of peptide nitrogen atoms with Cu
2+
. The intensity of the violet colour
that is formed is proportional to number of peptide bonds which, in turn, depends on the concentration of protein. The intensity of the colour can be measured by using a calorimeter at 540nm.
PROTOCOL Reagents and Apparatus: 1. Standard solution, S1; Concentration: 46.75 g/L 2. Test (Serum) sample solution (T1 and QC) containing unknown concentration of protein 3. Biuret reagent (contains sodium potassium tartrate, cupric sulfate, sodium hydroxide, potassium iodide)
4. Micropipettes 20l 5. Cuvetts 6. Spectrophotometer 7. Vortex
Procedure: 1. The test tubes were labeled as B for Blank, S1 for standard and T1, T2 and QC for Test samples. 2. 1.0 ml of Biuret reagent was added into each tube. 3. A micropipette was used to add 20l of standard and test sample to the corresponding test tubes. 4. The tubes were mixed well by vortexing and were leaved at room temperature for 30 minutes at 25oC at room temperature. 5. The calorimeter was zeroed with the blank solution and the optical density (OD) or absorbance was read at 540nm. 6. The results were tabulated and formula was used to calculate the concentration of total protein.
Concentration of total protein = ODtest ODstd
X ConcStd
RESULT Blank Standard Test (T1) Test (T2) Q.C
1 Optical density
0.312
0.386
0.427
0.370
0.318
0.392
0.432
0.376
Average Concentration of albumin (g/L)
0.315
0.389
0.4295
0.373
59.8
73.85
81.57
70.81
Concentration range of QC: 59.8 74.6 g/L
Normal Range Total Protein : 64g/L 83g/L Albumin Globulins A/G ratio : 35g/L 50g/L : 29g/L 33g/L : 1.2 to 1.5
DISCUSSION The normal range of total protein is 64g/L to 83g/L. Based on the result above, the concentration of the standard is 59.8 g/L, for T1 and T2; the concentrations are 73.85 g/L and 70.81 g/L respectively. The concentration of QC is 70.81 g/L. Internal QC acts as quality control in determining whether the method is acceptable. The range of concentration of QC is 59.8 to 74.6 g/L. In this practical, the concentration of QC is within the range, thus the concentration of T1 and T2 are acceptable. The concentration of total protein in both T1 and T2 are normal. Biuret method is one of protein quantification method in handling protein samples for isolation and characterization and is a prerequisite step before submitting proteins for chromatographic, electrophoretic or immunochemical analysis and separation. The name of Biuret method is derived from the reaction between biuret and cupric ions in an
alkaline medium. A protein assay method should be chosen based on the sensitivity and
accuracy of method as well as the condition of the sample to be analyzed. Biuret total protein reagent is the best choice if the total protein concentration in the samples is high (5 to 160 mg/ml). It is the most widely used calorimetric method; however it is not specific to the components of the serum protein. It is the earliest colorimetric protein assay methods developed for the determination of protein (Gornall, Bardawill, & David, 1949). Compounds containing two or more peptide bonds react with the biuret reagent forming a purple colored complex (Boyer, 2000). The colored product is the result of the coordination complex of copper atom and two nitrogen atoms from each peptide chain (Switzer & Garrity, 1999). 30 minutes are required for the colour to reach the maxiumem intensity, thus the method is a bit time consuming. This method is also limited in which haemolysed and lipaemic sera will interfere strongly with the measurement of proteins. There are certain factors that cause physiologic changes of total prorein. Haemoconcentration causes an increase in serum total proteins occurs in dehydration. An increase may also occure in multiple myeloma, macroglobulinaemia, chronic infections,
chronic liver disease and auto-immune diseases. A decrease in serum total proteins may results from heavy losses of proteins in urine as in nephritic syndrome. Protein undernutrition, intestinal malabsorption and protein losing enteropathy may also lower the serum total proteins. A decrease may also occur in shock, burns, crush injuries, and hemorrhage. Increased levels of total protein is associated with cholelithiases, multiple myeloma and liver cirrhosis.Breakdown of proteins, as in hyperthyroidism, un-treated diabetes mellitus, wasting diseases may also lower the level of proteins in serum. The concentration of globulins can also be calculated by subtracting the concentration of total protein with concentration of albumin. The calculated ratio of albumin to globulins, termed the A/G ratio. Normally, there is a little more albumin than globulins, giving a normal A/G ratio is between 1.2 and 1.5. For Standard, the ratio is 3.58, for test 1 and test 2, the ratio are 1.45 and 0.87 respectively. For QC, the ratio is 1.76. A low A/G ratio may reflect overproduction of globulins, such as seen in multiple myeloma or autoimmune diseases, or low albumin synthesis due to cirrhosis, or selective loss of albumin from the circulation, as occurs with kidney disease. A high A/G ratio suggests underproduction of immunoglobulin as may be seen in some genetic deficiencies and in some leukemias. More specific tests, such as albumin, liver enzyme tests, and serum protein electrophoresis must be performed to make an accurate diagnosis. Low A/G ratio for test 2 and high A/G ratio for standard and QC require further diagnosis. For test 1, the ratio is within the normal range.
CONCLUSION The intensity of the colour of protein + Cu2+ complex (blue-violet) is directly proportional to the concentration of protein present in the sample. The concentrations of total protein in both Test samples are within the normal range and there might be no clinical significances associated with the normal concentration. However, the A/G ratio is abnormal for the standard, test 2 and QC which requires further diagnosis as the condition might be associated with clinical significances due to abnormal concentration of globulin.
QUESTIONS 1. Name the other methods by which total protein can be measured. a. Z-scan technique (Dhinaa, A. and Palanisamy, P., 2010) b. Bradford Protein assays (Bradford, M.M., 1976) 2. What is the importance of Reagent blank in a calorimetric assay? Reagent blank is important in calibration of calorimeter. This solution contains only the diluent used for making the standard solution. Reagent blank is important in spectroscopy to negate the effects of Background. This is to assure that the readings are exclusively due to the components that been measured, not due to extraneous chemical in solution.
3. From the albumin and total protein value for each sample, calculated the a. Serum globulins: Total proteins Albumin Standard: Serum globulins: 59.8 - 46.75 = 13.05 g/L Test 1: Serum globulins: 73.85 - 43.69 = 30.16 g/L Test 2: Serum globulins: 81.57 37.98 = 43.59 g/L QC: Serum globulins: 70.81 - 45.18 = 25.63 g/L b. A/G Ratio: Albumin/Globulin Standard: A/G Ratio: 46.75/13.05 = 3.58 Test 1: A/G Ratio: 43.69/30.16 = 1.45 Test 2: A/G Ratio: 37.98/43.59 = 0.87 QC: A/G Ratio: 45.18/25.63 = 1.76
PRACTICAL 1C: SEPARATION OF SERUM PROTEINS BY ELECTROPHORESIS INTRODUCTION Protein molecules in solution will possess a combination of negative and ositive charges. The net charge on a molecule being dependent upon the balance of the types of amino acids in the protein and the pH of the solution. In electrophoresis, the pH of the solution is controlled by adjusting it with buffers. At the pH used in most methods, most serum protein possess a net negative charge (anions), some more negative than others. When an electrical current is conducted through the protein solution, the protein move toward anode. Because the protein differ in the magnitude of their negative charge, and to same extent because of their size differences, they move toward the anode at different rates. The more bulky the protein, the less negatively charged molecules and move more slowly than albumins, which are relatively small and more negative. The relative influence of size vs charge depends upon the medium used for the electrophoresis: cellulose acetate is primarily charge; with agarose gel, size assumes a greater role; with polyacrylamide gel size is most important reseparating the fractions. Regardless of medium, the net result of these charge and size differences in molecules is the ability to separate the mixture of proteins into its fractions and also to identify the components based upon the distances that they have moved during the time of the test. Further, the various protein fractions can also be quantified by staining them and measuring the intensity of the colour. The principle behind the electrophoresis is the protein in solution at a specified pH will separate from each other when exposed to an electrical current for a period of time. PROTOCOL Components of Electrophoresis System 1. Support media which is 0.5% agarose gel 2. Buffer system Barbital buffer pH 8.3 3. Power pack, Electrophoresis apparatus 4. Serum protein fixative solution (Methanol), staining solution (AmidoBlack) and destaining solution (10% acetic acid)
5. Other accessories requied are Sample Gel holder, Template (to load sample), filter paper wicks, drying oven and incubator, pipettes, tips and Detection system (densitometer) for quotation of protein fractions. Procedure Electrophoresis was run in batches on Deluxe electrophoresis chamber. Sera were applied with the help of wire loop applicator. Agarose gel was used as a support medium. Barbital buffer was set at pH 8.3. Buffer pH was checked with the help of a pH meter before use in electrophoresis. Line of application was directed towards cathode, and current was applied at 100 Volts for 45 minutes. Different protein fractions moved depending upon charge, molecular weight and size. Fixation was performed by methyl alcohol 85% and glacial acetic acid 10% for 5 min. Staining was done with the help of AmidoBlack in 3% acetic acid for10 min, whereas clearing was done with 10% acetic acid for 20 min. Strips were dried in hot air oven and densitometric scanning was done for quantification of different protein fractions. The procedure is modified based on paper by Waqar Azim, Saad Azim, Khalid Ahmed et al. (2004).
RESULT
Albumin 1-globulin 2-globulin -globulin -globulin
Figure 1: Electrophoresis pattern
DISCUSSION Serum protein electrophoresis is a simple, reliable and specific method of separating different protein fractions. Based on the result, the lane 1 shows the electrophoresis pattern of normal serum while both lane 3 and lane 4 shows the electrophoresis pattern of abnormal serum. There are five classes of plasma proteins which are albumin, 1-globulin, 2-globulin, -globulin and -globulin. Albumin moves fastest due its low molecular weight, followed by 1-globulin, 2-globulin, -globulin and -globulin. -globulin is the slowest due to its high molecular weight. By comparing the intensity of the each types of serum protein, albumin has the highest intensity which indicates high concentration in serum, followed by -globulin. The normal range for total serum protein is 6-8 g/dl. More than half of total serum protein (3.5-5 g/dl) is accounted for by albumin synthesized in liver. The remaining total serum globulin fraction (2-3.5 g/dl) is comprised mainly by alpha and beta globulins synthesized by the liver, and by immunoglobulins in the gamma band synthesized by plasma cells.
Figure 2: Normal serum protein electrophoresis (home.comcast.net) In lane 3, the abnormal pattern shows low intensity of -globulin which can be assumed to low concentration of -globulin than normal. Lane 3 pattern can be associated with clinical conditions such as hypercholesterolemia, iron deficiency anemia and multiple myeloma. For lane 4 pattern, the -globulin has high intensity showing high concentration of -globulin than normal. Lane 4 pattern can be associated with clinical conditions such as
rheumatoid arthrisis, systemic lupus erythomatosus, cirrhosis, chronic liver disease and multiple myeloma. Electrophoresis has proved to be very useful in subfractioning or separating different types of proteins. it has turned out to be a very useful diagnostic tool. Electrophoresis proved very useful when routine investigations were hard to determined. Correct monitoring of buffer pH, voltage, equal quantity of test and control applied and skill of technologist is the prime importance in improving the quality of strips and proper interpretation of results.
Figure 3: Electrophoretic pattern of different diseases (Waqar Azim, Saad Azim, Khalid Ahmed et al., 2004) CONCLUSION Albumin is the plasma protein that moves fastest due to low molecular weight and has high intensity due to high concentration of albumin in the blood serum. The abnormal electrophoretic pattern is associated with different diseases based on physiologic or pathologic changes of serum protein. Electrophrosis has become the main tool in separating the components of protein serum.
QUESTIONS 1. Name the 5 classes of plasma proteins and write which one moves fastest and why. There are five classes of plasma proteins which are albumin, 1-globulin, 2-globulin, -globulin and -globulin. Albumin moves fastest due its low molecular weight. 2. What happens when there is a very low level of albumin in blood? Hypoalbuminemia causes a decrease in oncotic pressure which can lead to water retention and subsequent swelling in the body. It also can lead to symptoms that affect the muscles of the body such as muscle weakness, muscles fatigue or muscle cramping. In addition, individual who has been diagnosed with hypoalbuminemia might experience low appetite. Ascites; an excess fluid that collects in the space between the abdominal wall and the abdominal organs might also be present. Pleural effusion is also common in patient with hypoalbuminemia. It is defined as the accumulation of fluid in the space that surrounds the lungs.
3. Name two clinical conditions that lead to Hyperalbuminemia and Hypoalbuminemia. Hyperalbuminemia is generally not observed. Hypoalbunimeia is associated with malnutrition and malabsorption syndrom,
4. What are the other ways by which serum proteins can be separated? The other ways are and high-voltage electrophoresis (ion-exchange, immunodiffusion, reverse phase
immunoelectrophoresis, chromatography)
chromatography
5. Name two stains that binds to proteins. Coomassie Brilliant Blue and silver.
6. What is the pH of buffer? What is the reason for choosing this pH? The buffer pH is 8.3. The isoelectric point of most proteins is between pH 4.0 and 7.5. In pH 8 to 9, proteins will take on a negative charge and migrate to the anode. Most protein electrophoresis is performed at pH 8.3 so that the proteins become anions and migrate to the positively charged electrode (anode).
7. Name the clinical conditions that lead to the abnormal serum pattern of lane 3 and 4. Lane 3: hypercholesterolemia, iron deficiency anemia and multiple myeloma Lane 4: rheumatoid arthrisis, systemic lupus erythomatosus, cirrhosis, chronic liver disease and multiple myeloma REFERENCES 1. Ramik Sood. Textbook of Medical Laboratory Technology. New Delhi: Jaypee. 2006 2. Waqar Azim, Saad Azim, Khalid Ahmed et Al. Diagnostic Significance Of Serum Protein Electrophoresis" Biomedica Vol. 20 (2004), 40-44. 11 March 2012 < www.thebiomedicapk.com/articles/2.pdf> 3. Gel Electrophoresis of Protein AES Application Focus, 11 March 2012 <www.aesociety.org/areas/pdfs/Garfin_1DE_WebArticle9-07.pdf> 4. Albumin 11 March 2012 <http://www.rnceus.com/lf/lfalb.html> 5. Method for the determination of albumin in biological fluids European Patent Application (1988), 11 March 2012 <https://data.epo.org/publication-server/htmldocument?PN=EP0287745%20EP%200287745&iDocId=3864605> 6. Total Protein Assay Biochemistry 353. 11 March 2012 <http://www.science.smith.edu/departments/Biochem/Biochem_353/Bradford.html> 7. Protein, Total, Clinical Significance The Clinical Chemistry. 11 March 2012. <http://www.chronolab.com/point-ofcare/index.php?option=com_content&view=article&id=361&Itemid=58> 8. Total Protein and A/G ration Lab Tests Online (2011), 12 March 2012. <http://labtestsonline.org/understanding/analytes/tp/tab/test> 9. Hypoalbuminemia Chemocare.com, 12 March 2012. <http://www.chemocare.com/managing/hypoalbuminemia-low-albumin.asp> 10. Clinical Application of Serum Protein Determinations, Laboratory Medicine and Pathophysiology (2001), 12 March 2012. <http://home.comcast.net/~theWebDoc/Lectures/Winter/Proteins/indexpr.htm> 11. Guidelines on Standard Operating Procedures for Clinical Chemistry, World Health Organization (2000), 10 March 2012. <http://whqlibdoc.who.int/searo/2000/SEA_HLM_328.pdf>
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Rna Extraction by Trizol, Dnasei Treatment and RT-PCRDocument2 pagesRna Extraction by Trizol, Dnasei Treatment and RT-PCRMaisarah Ab SamadNo ratings yet
- BIOSTATISTICSDocument8 pagesBIOSTATISTICSMaisarah Ab SamadNo ratings yet
- Reproductive CloningDocument8 pagesReproductive CloningMaisarah Ab SamadNo ratings yet
- Esei EthicsDocument5 pagesEsei EthicsMaisarah Ab SamadNo ratings yet
- Normal Cell Physiology, Cell Growth & Cell MetabolismDocument12 pagesNormal Cell Physiology, Cell Growth & Cell MetabolismMaisarah Ab SamadNo ratings yet
- Praktikal 1Document14 pagesPraktikal 1Maisarah Ab SamadNo ratings yet
- List of Drugs Pharmacology 2Document13 pagesList of Drugs Pharmacology 2Maisarah Ab SamadNo ratings yet
- Constructing a Genomic DNA LibraryDocument10 pagesConstructing a Genomic DNA LibraryMaisarah Ab SamadNo ratings yet
- GTB 204 Molecular Tech Technic OSPE 2002/2003Document3 pagesGTB 204 Molecular Tech Technic OSPE 2002/2003Maisarah Ab SamadNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Interpreting Piping and Instrumentation DiagramsDocument41 pagesInterpreting Piping and Instrumentation DiagramsFredric Tun100% (2)
- Discuss The Challenges For Firms To Operate in The Hard-Boiled Confectionery Market in India?Document4 pagesDiscuss The Challenges For Firms To Operate in The Hard-Boiled Confectionery Market in India?harryNo ratings yet
- Final Decision W - Cover Letter, 7-14-22Document19 pagesFinal Decision W - Cover Letter, 7-14-22Helen BennettNo ratings yet
- The Art of Now: Six Steps To Living in The MomentDocument5 pagesThe Art of Now: Six Steps To Living in The MomentGiovanni AlloccaNo ratings yet
- Theoretical and Actual CombustionDocument14 pagesTheoretical and Actual CombustionErma Sulistyo R100% (1)
- Certificate Testing ResultsDocument1 pageCertificate Testing ResultsNisarg PandyaNo ratings yet
- Laser Surface Treatment ProcessesDocument63 pagesLaser Surface Treatment ProcessesDIPAK VINAYAK SHIRBHATENo ratings yet
- Material and Energy Balance: PN Husna Binti ZulkiflyDocument108 pagesMaterial and Energy Balance: PN Husna Binti ZulkiflyFiras 01No ratings yet
- Air Arms S400 EXPDocument3 pagesAir Arms S400 EXPapi-3695814No ratings yet
- Virchow TriadDocument6 pagesVirchow Triadarif 2006No ratings yet
- 1989 GMC Light Duty Truck Fuel and Emissions Including Driveability PDFDocument274 pages1989 GMC Light Duty Truck Fuel and Emissions Including Driveability PDFRobert Klitzing100% (1)
- Library Dissertation in Community DentistryDocument9 pagesLibrary Dissertation in Community DentistryPayForPaperCanada100% (1)
- Sto - Cristo Proper Integrated School 1 Grading Grade 9 Science Table of SpecializationDocument2 pagesSto - Cristo Proper Integrated School 1 Grading Grade 9 Science Table of Specializationinah jessica valerianoNo ratings yet
- Internship ReportDocument18 pagesInternship ReportRathan Kumar SMNo ratings yet
- Awakening The MindDocument21 pagesAwakening The MindhhhumNo ratings yet
- Henry Stevens - Hitler's Flying Saucers - A Guide To German Flying Discs of The Second World War New Edition (2013, Adventures Unlimited Press) - Libgen - lc-116-120Document5 pagesHenry Stevens - Hitler's Flying Saucers - A Guide To German Flying Discs of The Second World War New Edition (2013, Adventures Unlimited Press) - Libgen - lc-116-120sejoh34456No ratings yet
- NDE Procedure - Radiographic TestingDocument43 pagesNDE Procedure - Radiographic TestingJeganeswaranNo ratings yet
- AI Model Sentiment AnalysisDocument6 pagesAI Model Sentiment AnalysisNeeraja RanjithNo ratings yet
- 2019 Course CatalogDocument31 pages2019 Course CatalogDeepen SharmaNo ratings yet
- PC3 The Sea PeopleDocument100 pagesPC3 The Sea PeoplePJ100% (4)
- Cost Analysis and Financial Projections for Gerbera Cultivation ProjectDocument26 pagesCost Analysis and Financial Projections for Gerbera Cultivation ProjectshroffhardikNo ratings yet
- Compare Blocks - ResultsDocument19 pagesCompare Blocks - ResultsBramantika Aji PriambodoNo ratings yet
- Who will buy electric vehicles Segmenting the young Indian buyers using cluster analysisDocument12 pagesWho will buy electric vehicles Segmenting the young Indian buyers using cluster analysisbhasker sharmaNo ratings yet
- Conjoint Analysis Basic PrincipleDocument16 pagesConjoint Analysis Basic PrinciplePAglu JohnNo ratings yet
- Juan Martin Garcia System Dynamics ExercisesDocument294 pagesJuan Martin Garcia System Dynamics ExercisesxumucleNo ratings yet
- Garlic Benefits - Can Garlic Lower Your Cholesterol?Document4 pagesGarlic Benefits - Can Garlic Lower Your Cholesterol?Jipson VargheseNo ratings yet
- g4 - Stress Analysis of Operating Gas Pipeline Installed by HorizontalDocument144 pagesg4 - Stress Analysis of Operating Gas Pipeline Installed by HorizontalDevin DickenNo ratings yet
- Aircraft Design Project 2Document80 pagesAircraft Design Project 2Technology Informer90% (21)
- Life of A Landfill PumpDocument50 pagesLife of A Landfill PumpumidNo ratings yet
- T9001 T9002 T9003 T9004: Tecn# Originator Title Aging Status of TecnDocument2 pagesT9001 T9002 T9003 T9004: Tecn# Originator Title Aging Status of TecnThanalachmy GopiNo ratings yet