Professional Documents
Culture Documents
The Autonomic Nervous System in The Head and Neck
Uploaded by
Ismail Bazly ZarirOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Autonomic Nervous System in The Head and Neck
Uploaded by
Ismail Bazly ZarirCopyright:
Available Formats
15-May-09
The autonomic nervous system in the head and neck
Organization of the nervous system
Anatomically, the nervous system is organized into:
The central nervous system (CNS), consisting of the brain and spinal cord. The peripheral nervous system (PNS), consisting of the cranial and spinal nerves.
Physiologically (functionally), the PNS is divided into:
The somatic nervous system. The autonomic nervous system. This system is further divided into sympathetic nervous system and parasympathetic nervous system.
The somatic nervous system
It mainly supplies skeletal muscles through its motor nerves and it also provides general and special sensations through its sensory nerves. The somatic nervous system is totally under voluntary (conscious) control.
Motor innervation (one function): skeletal muscle contraction. Sensory innervation (two functions): general and special sensations.
1. General sensations such as pain, thermal (hot and cold), pressure
and tactile (touch)!?.
2. Special sensations (only four), which are vision, smell, taste, and
hearing. Note Medically, tactile (touch) sense is considered as a general sense, not special. Dont forget that.
The autonomic nervous system
The autonomic nervous system supplies cardiac muscle, smooth muscles, and secretory glands (sweat, salivary, lacrimaletc), through itstwo divisions the sympathetic and the parasympathetic systems.It isunder involuntary control.
Motor innervation (two functions): either inhibit or excite the effector organs through the sympathetic or the parasympathetic nervous systems, but which one? The sympathetic and parasympathetic nervous systems dually innervate most visceral organs, and in normal situations both systems are partially active; this on going activity is called sympathetic or parasympathetictone or tonic activity. Under given circumstances, activity of one system can dominate the other.In emergency or stressful situations fight or flight response, the sympathetic system will dominates to prepare the body for strenuous physical activity. While in quiet, relaxed situations rest and digest, the parasympathetic system will takeover.
Sensory innervation (one function): sensory nerves terminate on the effector organs, by binding to internal receptors. These receptors are chemical (chemoreceptors); like the carotid body, which monitors oxygen level in blood, and mechanical (mechanoreceptors); like the carotid sinus, which monitors blood pressure.
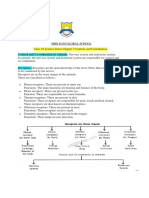
Somatic and autonomicnerves pathway
Somatic nerves pathway The cell bodies of almost all motor neurons are within the spinal cord. The only exception: the cell bodies of motor neurons supplying muscles in the head are in the brain stem. Now all the axons of motor neurons will leave from their origin in the CNS, and travel all the way to the effector organ, which is the skeletal muscle without any interruption (single neuron pathway). Usually the axons are myelinated.
Autonomic nerves pathway (preganglionic neuron, autonomic ganglion, postganglionic neuron)
Each autonomic nerve pathway extending from the CNS to an innervated organ is a two-neuron chain. The cell body is located in the CNS. Its axon, the preganglionic fiber, synapses with the second neuron, which lies within an autonomic ganglion. The axon of the second neuron, the postganglionic fiber, innervates the effector organ.
Preganglionic (also known as presynaptic or 1st order) neurons: originate from the CNS, all the way to the autonomic ganglia, where theysynapse with postganglionic neurons. They are usuallymyelinated.
Autonomic ganglion: aggregation of neuronal cell bodies and supporting cells like glial cells. Because the autonomic nervous system has two subdivisions, the ganglia could be sympathetic or parasympathetic. The sympathetic ganglia lie within the sympathetic trunk. While the parasympathetic ganglia are calledterminal ganglia (because they lie in or near the effector organs).
Postganglionic (also known as postsynaptic or 2nd order neurons: their cell bodies lie within the autonomic ganglia, all the way to the effector organ. They are usually unmyelinated.
Figure 1: motor nerves pathway of the somatic and autonomic nervous system.
Sympathetic motor nerves pathway Sympathetic nerve fibers (thoracolumbar) originate in the thoracic and lumbar regions of the spinal cord. Most sympathetic preganglionic fibers are very short; synapsing with cell bodies of postganglionic neurons within ganglia that lie in a sympathetic ganglion chain (the sympathetic trunk) located along either side of the spinal cord. Long postganglionic fibers originating in the ganglion chain end on the effector organs. Parasympathetic motor nerves pathway Parasympathetic preganglionic fibers (craniosacral) arise from the cranial (brain) and sacral areas of the CNS. These fibers are longer than sympathetic preganglionic fibersbecause they do not end until they reach terminal ganglia that lie in or near the effector organs. Very shortpostganglionic fibers end on the cells of an organ itself. The tables below will help you to sum up the main ideas for what was explained.
Table1: Comparison of the autonomic nervous system and the somatic nervous system
Feature
Site of origin Types of control Organs innervated Type of innervation
Autonomic nervous system
Brain or spinal cord Under involuntary control Cardiac muscle, smooth muscles and glands Most effector organs dually innervated by the two antagonistic branches of this system (sympathetic and parasympathetic) Dual functions: excitation and inhibition
Somatic nervous system
Spinal cord for most; those supplying muscles in head originate in the brain Under voluntary control Skeletal muscle Effector organs innervated only by motor neurons
Effects on Single function: stimulation effector of skeletal muscle organ contraction Sensory Single function: non Two functions: general and innervation conscious sensation only special Number of Two neuron chain pathway Single neuron neurons (preganglionic and from origin postganglionic) in CNS to effector organ Table 2:Distinguishing features of sympathetic nervous system and parasympathetic nervous system.
Feature
Origin of preganglionic fiber Origin of postganglionic fiber (location of ganglia) Length of fiber
Sympathetic nervous system
Thoracic and lumbar regions of spinal cord Sympathetic ganglion chain (near spinal cord) Short preganglionic fibers Long postganglionic fibers
5
Parasympathetic nervous system
Brain and sacral region of spinal cord Terminal ganglia (near or in effector organs) Long preganglionic fibers Short postganglionic fibers
myelination Dominance
Preganglionic fibers only Emergency fight or flight situations
Preganglionic fibers only Quiet rest and digest situations
Table 3:effects of autonomic nervous system on various organs
Organ
Heart Blood vessels (smooth muscles) Digestive tract Glands Sweat glands Salivary glands
Effect of sympathetic stimulation
Increase rate and force of contraction Constriction Decrease motility Stimulate secretion by most sweat gland Stimulate of small volume of thick saliva rich in mucus
Effect of parasympathetic stimulation
Decrease rate and force of contraction Dilation Increase motility Stimulate secretion by some sweat glands Stimulate of large volume of watery saliva rich in enzymes
Sympathetic ganglia in the head and neck
In the neck region, there are three cervical ganglia superior, middle and inferior, they are part of the sympathetic chain.The most important one is the superior one, because it carries most of the functions Location: attached posterior to the carotid sheath, within he carotid triangle. The superior ganglion usually fuses with the 1st thoracic ganglion; they form a large ganglion called the stellate ganglion.
Parasympathetic ganglion in the haed and neck
They are 4 in number:
1. Ciliary ganglion. 2. Ptergopalatine ganglion 3. Otic ganglion 4. Submandibular ganglion
Ciliary ganglion
It is located between the optic nerve (its lateral side) and lateral rectus muscle. It suspended in its position by communicating branch from nasociliary nerve (carries general sensations from the eyeball). Nasociliary nerve is a branch from the ophthalmic nerve. It receives its preganglionic parasympathetic fibers from oculomotor nerve (III), via the inferior branch (nerve to inferior oblique). The postganglionic parasympathetic fibers leave the ganglion in the short ciliarynerves (branches from nasociliary), which pass forward to the posterior aspect of the eyeball, they supply sphincter pupillae muscle and ciliary muscle. What is the function(s) of these muscles?
Sphincterpupillae muscle constricts the pupil. Ciliary muscle controls the shape of lens, by making them more convex to accommodate near vision.
Postganglionic sympathetic fibers pass from the superior cervical ganglion in the long ciliary nerves (branches from nasociliary) into the eyeball to supply dilator pupillae muscle, which dilates the pupil.
Horners syndrome
Damage to sympathetic innervation through superior cervical ganglion.
Symptoms 1. Ptosis: dropping of upper eyelid (WHY?) Once the superior cervical ganglion is damaged, the sympathetic innervation in the head region is lost. Levatorpalpebreasuperiorismuscle is responsible of raising the upper eyelid, this muscle has two parts; the superior part is made of skeletal muscle, supplied by oculomotor nerve (III), the inferior part is made of smooth muscle, supplied by sympathetic nerves. So the inferior part will be paralyzed and the muscle will not be able to hold the upper eyelid in its proper position.
2. Constriction of pupil: because dilator pupillea muscle is paralyzed
and the constrictor pupillea will takeover.
3. Anhydrosis: lack of sweating
4. Flushing of the face (WHY?) Due to parasympathetic dominance, which will vasodilate the blood vessels within the skin.
Ptergopalatine ganglion
Located in the Ptergopalatine fossa, suspended by maxillary nerve (V2) It receives its preganglionic parasympathetic fibers from greater petrosal nerve (branch from facial nerve). Postganglionic parasympathetic fibers leave in the maxillary nerve, they then run in the zygomaticotemporal nerve and the lacrimal nerve (branch from the ophthalmic nerve) to reach the lacrimal gland. They supply the gland with secretomotorinnervation. Postganglionic sympathetic fibers from superior cervical ganglia reach the ganglia via internal carotid artery, where they form the deep petrosalnerve. The deep petrosal nerve will join the greater petrosal nerve to form the nerve of the pterygoid canal (or vidian nerve), which will
enter the ganglion.
Otic ganglion
Located below foramen ovale, medial to mandibular nerve. It suspended by nerve to medial pterygoid. It receives its preganglionic parasympathetic fibers from glossopharyngeal nerve (IX), by its tympanic branch the tympanic nerve, which will form the tympanic plexuses in the tympanic cavity within the middle ear. The lesser petrosal nerve leaves the plexuses by passing anterior in the floor of middle cranial fossa, and then leaves through foramen ovale to reach the ganglion. Postganglionic parasympathetic fibers leave by joining the auriculotemporal nerve to the parotid gland and serve as secretomotor fibers.
Postganglionic sympathetic fibers from the superior cervical ganglion pass directly to the parotid gland.
Submandibular ganglion
Located lateral to hyoglossus muscle, suspended by lingual nerve. It receives its preganglionic parasympathetic fibers from facial nerve, through chorda tympani, then it join the lingual nerve within the infratemporal fossa at the lower border of lateral ptergoidmuscle. Postganglionic parasympathetic fibers are distributed directly to sublingual and Submandibular glands, because the ganglion is very close to the glands. They supply glands by secrertomotor fibers. Postganglionic sympatheticfrom superior cervical ganglion reach the glands, and they are vasomotor to the blood vessels of the glands (reduce the water content of saliva).
The end Done by: ME
Hiatham.H.M.Mendeny
10
11
You might also like
- Introduction To The Nervous System PDFDocument11 pagesIntroduction To The Nervous System PDFEmanuel DragomirescuNo ratings yet
- Medical Surgical Nursing PinoyDocument85 pagesMedical Surgical Nursing PinoyrosebaseNo ratings yet
- The Central Nervous System: BrainDocument12 pagesThe Central Nervous System: BrainsheinelleNo ratings yet
- Bechamp, Rife and Naessens (The Unhived Mind) PDFDocument4 pagesBechamp, Rife and Naessens (The Unhived Mind) PDFpaulxe100% (1)
- Natural Remedies For FibroidsDocument2 pagesNatural Remedies For Fibroidsafm2026No ratings yet
- EnamelDocument26 pagesEnamelIsmail Bazly ZarirNo ratings yet
- Nervous System: A Tutorial Study GuideFrom EverandNervous System: A Tutorial Study GuideRating: 5 out of 5 stars5/5 (1)
- CH 7 The Nervous SystemDocument4 pagesCH 7 The Nervous Systemapi-267543553No ratings yet
- Q3 - Nervous and Endocrine Systems - Science10 PDFDocument84 pagesQ3 - Nervous and Endocrine Systems - Science10 PDFGabriel Pasumbal100% (1)
- Assessment of The Ear, Nose and ThroatDocument40 pagesAssessment of The Ear, Nose and Throatsnickers_j100% (3)
- UNIT 4 (Nervous System)Document14 pagesUNIT 4 (Nervous System)Workinesh Kaynabo KambaloNo ratings yet
- Nervous SystemsDocument37 pagesNervous SystemsHannah CabritoNo ratings yet
- Nervous System of HumanDocument12 pagesNervous System of Humanibnulwaqt97% (33)
- The Nervous System-13 Dr. Hazim AL-RawiDocument16 pagesThe Nervous System-13 Dr. Hazim AL-RawiDrAli Al-FendiNo ratings yet
- Wild Animals Reading Writing WorksheetDocument2 pagesWild Animals Reading Writing WorksheetRRKATANo ratings yet
- Case Report - PromDocument16 pagesCase Report - PromFauziyyahrNo ratings yet
- The Autonomic Nervous SystemDocument20 pagesThe Autonomic Nervous SystemPaige Buchanan100% (1)
- Lecture 15 - Autonomic Nervous SystemDocument26 pagesLecture 15 - Autonomic Nervous SystemFlavius AnghelNo ratings yet
- Organization of The Nervous System (Student)Document4 pagesOrganization of The Nervous System (Student)raquel_kNo ratings yet
- Introduction To The Nervous SystemDocument8 pagesIntroduction To The Nervous SystemVal F. VilarNo ratings yet
- AnatomyDocument84 pagesAnatomyKumar M V ScNo ratings yet
- PNA100 Chapter 11 ReviewDocument5 pagesPNA100 Chapter 11 ReviewaamenaNo ratings yet
- Z (H) IV Chordata SHDocument3 pagesZ (H) IV Chordata SHalshareefsaadalshareefNo ratings yet
- V. Anatomy & PhysiologyDocument5 pagesV. Anatomy & PhysiologyAbigael Patricia GutierrezNo ratings yet
- Autonomic Nervous SystemDocument13 pagesAutonomic Nervous SystemSreejesh Rk100% (1)
- SSO Ok-EditDocument60 pagesSSO Ok-EditNahla FaridaNo ratings yet
- Lecture 5.doc AnsDocument8 pagesLecture 5.doc AnsElijah KamaniNo ratings yet
- Unit 1 LecNotesDocument49 pagesUnit 1 LecNotesAnn NguyenNo ratings yet
- Nervous System: by Dr. K. Sumangala BhatDocument37 pagesNervous System: by Dr. K. Sumangala BhatanushkaNo ratings yet
- CHP 7 Class 10Document13 pagesCHP 7 Class 10sourabh nuwalNo ratings yet
- Human Anatomy and Physiology With Pathophysiology: Explain The Functions of The Nervous SystemDocument16 pagesHuman Anatomy and Physiology With Pathophysiology: Explain The Functions of The Nervous SystemJay-ar BarquerosNo ratings yet
- Autonomic Nervous System: Dept of Anatomy Afmc PUNE-40Document47 pagesAutonomic Nervous System: Dept of Anatomy Afmc PUNE-40Naresh KshirsagarNo ratings yet
- Automatic Nervous System: Autonomic DrugsDocument52 pagesAutomatic Nervous System: Autonomic DrugslalitrajindoliaNo ratings yet
- Autonomic Nervous System-NoteDocument13 pagesAutonomic Nervous System-NoteprosperosamegieNo ratings yet
- Control and CoordinationDocument11 pagesControl and CoordinationADITYA MISHRANo ratings yet
- Central Nervous SystemDocument11 pagesCentral Nervous SystemAshleyNo ratings yet
- Endocrine SystemDocument11 pagesEndocrine SystemAnanya MishraNo ratings yet
- Nervous SystemDocument5 pagesNervous SystemJhunelynNo ratings yet
- Integration and Coordination - SG3Document180 pagesIntegration and Coordination - SG3Marcos AlbaridaNo ratings yet
- Introduction To The Pharmacology of CNS Acting DrugsDocument62 pagesIntroduction To The Pharmacology of CNS Acting Drugsshuklasanskar2003No ratings yet
- Review of Peripheral Nervous System: Dr. Syed Atif AbbasDocument31 pagesReview of Peripheral Nervous System: Dr. Syed Atif AbbasAfif HalimNo ratings yet
- 7 Nervous SystemDocument37 pages7 Nervous SystemAthar Habib ShahaniNo ratings yet
- Nervous SystemDocument6 pagesNervous SystemCerene denzinNo ratings yet
- Module 13: Nervous System OrganizationDocument11 pagesModule 13: Nervous System OrganizationNaMoNo ratings yet
- 2autonomic Nervous SystemDocument28 pages2autonomic Nervous SystemSolomon H.No ratings yet
- BCH 431. TISSUE BiochemistryDocument24 pagesBCH 431. TISSUE BiochemistryOkoro Janeth chisomNo ratings yet
- BSC 100 Midterm Questions For Oral ExamDocument20 pagesBSC 100 Midterm Questions For Oral ExamNovochino CastilloNo ratings yet
- Samar Deb Easy and Interesting ADocument846 pagesSamar Deb Easy and Interesting ACharlieNo ratings yet
- Describe The Organization of The Nervous System Including The Central Nervous System and The Peripheral Nervous SystemDocument7 pagesDescribe The Organization of The Nervous System Including The Central Nervous System and The Peripheral Nervous SystemGeoffreyNo ratings yet
- Nervous System of AnimalsDocument10 pagesNervous System of AnimalsbigbangNo ratings yet
- I. Objectives A. General ObjectivesDocument32 pagesI. Objectives A. General ObjectivesLeana Ella Rivera YemaNo ratings yet
- Drugs Affecting The CNADocument5 pagesDrugs Affecting The CNAWendy VasquezNo ratings yet
- SCIENCEDocument3 pagesSCIENCENel BorniaNo ratings yet
- Nervous System ReviewerDocument4 pagesNervous System ReviewerSophia CaisipNo ratings yet
- Kepy 01 09 37 EtextDocument9 pagesKepy 01 09 37 Etextmradul guptaNo ratings yet
- BiologyDocument6 pagesBiologyExtreme gaming buddyNo ratings yet
- Nervous System FunctionsDocument10 pagesNervous System FunctionsJovi Leo PunoNo ratings yet
- Nervous System, Neuronal Communication and Organization of BrainDocument17 pagesNervous System, Neuronal Communication and Organization of BrainPriyamvada VermaNo ratings yet
- Nervous SystemDocument10 pagesNervous SystemAlicia ValverdeNo ratings yet
- Chapter 7 Control and CoordinationDocument8 pagesChapter 7 Control and CoordinationS. KishoreNo ratings yet
- Psychology Week 3 NotesDocument9 pagesPsychology Week 3 Notes01234No ratings yet
- ادوية lec4Document11 pagesادوية lec4mmkfefeNo ratings yet
- The Receiving Mechanism: Sense Organs Are Sensitive Nerve Endings Located in Certain Body Parts. They Are Receptors ofDocument5 pagesThe Receiving Mechanism: Sense Organs Are Sensitive Nerve Endings Located in Certain Body Parts. They Are Receptors ofArlene Cerdeña SalcedaNo ratings yet
- Human BrainDocument17 pagesHuman BrainAkbota KuanishkyzyNo ratings yet
- Intro To Psych PrelimDocument113 pagesIntro To Psych PrelimAlexandra San PedroNo ratings yet
- Peripheral Nervous System: Division of The PNS and TheDocument3 pagesPeripheral Nervous System: Division of The PNS and Theawele lauraNo ratings yet
- Autacoids & RSDocument14 pagesAutacoids & RSIsmail Bazly ZarirNo ratings yet
- Lec #10 Introduction To CNS Pharmacology: 1. Voltage-GatedDocument13 pagesLec #10 Introduction To CNS Pharmacology: 1. Voltage-GatedAya ShahrouriNo ratings yet
- Arak2012 Summer.cDocument3 pagesArak2012 Summer.cIsmail Bazly ZarirNo ratings yet
- Lavender: Lavendula Augustifolia MillDocument18 pagesLavender: Lavendula Augustifolia MillIsmail Bazly ZarirNo ratings yet
- Botanical Description:: The Plant Has Small Pale-Blue Flowers That Bloom in Late Winter and Early SpringDocument13 pagesBotanical Description:: The Plant Has Small Pale-Blue Flowers That Bloom in Late Winter and Early SpringIsmail Bazly ZarirNo ratings yet
- Gundelia 2012cDocument8 pagesGundelia 2012cIsmail Bazly ZarirNo ratings yet
- N.favisim 2012cDocument9 pagesN.favisim 2012cIsmail Bazly ZarirNo ratings yet
- The Castor Bean Ricinus Communis: Common Names: Castor Bean, Castor Oil Plant, Wonder TreeDocument28 pagesThe Castor Bean Ricinus Communis: Common Names: Castor Bean, Castor Oil Plant, Wonder TreeIsmail Bazly ZarirNo ratings yet
- Media Biochemical TestsDocument36 pagesMedia Biochemical TestsIsmail Bazly ZarirNo ratings yet
- Neck Lump HistoryDocument4 pagesNeck Lump HistoryAlmomnbllah Ahmed100% (1)
- Pertanyaan Yang Harus DijawabDocument6 pagesPertanyaan Yang Harus DijawabMuhammad RhezaNo ratings yet
- Duck Rearing and ManagemntDocument49 pagesDuck Rearing and Managemntkaranpraba1901No ratings yet
- Test Bank For Ekg Plain and Simple 3rd Edition EllisDocument8 pagesTest Bank For Ekg Plain and Simple 3rd Edition Elliscanebrutalfniy66No ratings yet
- Prescription Pattern of Antibiotics Used in The Management of Respiratory Tract Infections in Paediatric PopulationDocument5 pagesPrescription Pattern of Antibiotics Used in The Management of Respiratory Tract Infections in Paediatric PopulationBaru Chandrasekhar RaoNo ratings yet
- Abigail BDocument3 pagesAbigail BbjhilarioNo ratings yet
- HIV-Associated Opportunistic Infections of The CNSDocument13 pagesHIV-Associated Opportunistic Infections of The CNSmauroignacioNo ratings yet
- Countercurrent Multiplier and ADHDocument5 pagesCountercurrent Multiplier and ADHAurora TamNo ratings yet
- Hemichordata and Invertebrate ChordatesDocument31 pagesHemichordata and Invertebrate ChordatesayonNo ratings yet
- Narrative TextDocument7 pagesNarrative TextNorma AyunitaNo ratings yet
- A Clinical ExemplarDocument5 pagesA Clinical Exemplarapi-302128044100% (1)
- Ordinary Wolves - A Novel by Seth KantnerDocument7 pagesOrdinary Wolves - A Novel by Seth KantnerMilkweed Editions50% (2)
- Agricultural Performance Survey of 2021 Wet Season in NigeriaDocument361 pagesAgricultural Performance Survey of 2021 Wet Season in NigeriaEnemona ShellengNo ratings yet
- Whooping Cough LectureDocument37 pagesWhooping Cough LecturePriyanshu MNo ratings yet
- GuppyDocument2 pagesGuppymartynunez12345No ratings yet
- Maham's Pre-Midterm Path NotesDocument190 pagesMaham's Pre-Midterm Path NotesVishal100% (1)
- Duchenne Muscular Dystrophy: A Cerebellar Disorder?: Shana E. Cyrulnik, Veronica J. HintonDocument11 pagesDuchenne Muscular Dystrophy: A Cerebellar Disorder?: Shana E. Cyrulnik, Veronica J. HintonFajri MuhammadNo ratings yet
- Preventive and Social MedicineDocument14 pagesPreventive and Social MedicineSuresh GuduruNo ratings yet
- KumeDocument28 pagesKumeGrace Clemenia-GrefaldiaNo ratings yet
- Week9&10 LEC Clinical Parasitology NEMATODESDocument18 pagesWeek9&10 LEC Clinical Parasitology NEMATODESSamuel ReyesNo ratings yet
- Cestodes 2020Document10 pagesCestodes 2020CDNo ratings yet
- Ace Reasoning New AddaDocument359 pagesAce Reasoning New Addajuinarka24112002No ratings yet
- Sakool ProfileDocument3 pagesSakool ProfileksakoolNo ratings yet
- Lungs and Lung Disease QuestionsDocument16 pagesLungs and Lung Disease QuestionsrkblsistemNo ratings yet
- DictTheSwatowDialect FieldeDocument648 pagesDictTheSwatowDialect FieldeKH QuahNo ratings yet