Professional Documents
Culture Documents
DK's KD
Uploaded by
Wiston IlaganOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DK's KD
Uploaded by
Wiston IlaganCopyright:
Available Formats
by:
Wiston E. Ilagan
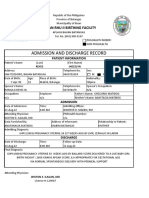
This is a case of D.K, 5 months old,
male, Filipino, Roman Catholic,
presently residing at 336 Quilo-Quilo
North P. Garcia, Batangas, who was
admitted due to fever of 21 days.
21 days PTA
Initially presented with fever (38 39 C) for 2 days
Paracetamol (10 mkdose),
Temporary relief of fever.
19 days PTA
Fever escalated (40 C)
Not relieved by Paracetamol.
Prompt consult at NL Villa Memorial Medical Center in
Lipa City Batangas.
Urinary Tract Infection based on urinalysis.
started with Ceftriaxone IV (123 mkdose)
17 days PTA
Defervescence
Ceftriaxone IV was shifted to Cefexime (6 mkday)
Discharged
In the afternoon of the same day, there was
reoccurrence of fever.
14 days PTA
Readmitted
Febrile (39.5 ), remittent
Cefixime discontinued
Shifted to Azithromycin
Irritable
ESR ( 48 mmol/hr) and CRP were requested
which showed increased values.
Given Hydrocortisone (5mkdose),
Diphenhydramine (1mkdose) and Ampicillin-
Sulbactam (100 mkday)
13 DAYS PTA
( + ) dry fissured lips, strawberry tongue , redness of the
bilateral eye and brawny edema of hands and feet
More irritable that he cant sleep.
Febrile (39 C).
Started on aspirin 80 mkD
11 days PTA
Given IVIG 2 g/kg.
Apparently well and disappearance of signs and
symptoms of KD
Deferevescence were noted, 48 hours after
administration.
Still on Azithromycin and developed loose stools.
Subsequently sent home on Aspirin tablet (80 mkday)
and Azithromycin.
9 days PTA
Initially asymptomatic but developed fever (39C)
in the afternoon
3 episodes of loose stools upon discharge
which
Prompted re-admission.
Referred to Pedia Intensivist
Looked up for alternative focus of infection.
Blood, urine and stool C/S was done that all
eventually turned negative .
8 days PTA
Started on piperacillin-tazobactam 89 mkd.
Referred to a pediatric cardiologist.
7 days PTA
2D echo was done: Dilated right coronary artery and left
coronary at 0.3 cm proximal and distal, minimal pericardial
effusion
Febrile (39 C).
Desquamating lesion on chest, abdomen and
extremities.
Erythematous rashes in the groin and buttocks area.
Started on methylprednisolone 255 IV
Aspirin was increased to 170 mg/tab 1 tab every 6
hours.
Stool and blood culture and sensitivity showed no
growth.
6 days PTA
IV methylprednisolone was shifted to oral
methylprednisolone 8 mg BID.
4 days PTA
Started on metronidazole.
Febrile (~38C).
3 days PTA
Febrile (39 C),
HAMA
discharged with home medications: Paracetamol
drops (10 mkdose), Metronidazole 125/ml,
Methylprednisolone 8 mg tab BID, and ASA 8
mg 1 tab tab OD.
2 days PTA
Febrile (38 C).
Paracetamol was given and was relieved.
1 day PTA
Afebrile, active, not irritable with decreasing signs
and symptoms of Kawasaki Disease.
His parents decided to bring him to Manila for
further evaluation.
Few hours PTA .
Upon examination in the clinic, febrile (38.4 C)
Admission
No previous hospitalizations or surgeries.
No known allergies to food or medications.
Born to a 30-year old G2P1.
Denied any illnesses or exposure to smoking/alcohol
intake/radiation during her pregnancy.
Term via normal spontaneous delivery
With no fetomaternal complications.
P
a
t
e
r
n
a
l
Hypertension
Diabetes
mellitus
Lung
carcinoma
M
a
t
e
r
n
a
l
Hypertension
Diabetes
mellitus
Breast
carcinoma
Social smile at 1 month.
Good head control; laughs loudly; and reaches for
objects
Follows moving objects with eyes and takes bottle in
mouth = 4 months
Breastfeeding until age of 2 with formula of S-26,
1:1 dilution
Consuming approximately 4 cm
.
Lives in a well-lit, well-ventilated house with 3
other household members.
Water source for consumption is distilled water,
not boiled. Garbage is collected daily.
Active and cheerful child and smiles to everyone
BCG, Hepa B, 1 dose of 5-in-1 (HiB/DPT/IPV)
vaccine, and 1 dose of 6-in-1
(HiB/IPV/DPT/HepaB) vaccine
no weight loss General
No jaundice, no cyanosis Skin
No swelling, discharge, tenderness,
discharge epistaxis, discharge, mass
HEENT
No cough, colds, difficulty of
breathing
RESPIRATORY
No cyanosis Cardiovasular
no hematemesis, constipation,
hematochezia
Gsstrointestinal
No polyuria, hematuria, discharge, (+)
erythematous rash in inguinal area
Genitourinary
No loss of consciousness, stiffening of
muscles, blank stare, drooling of saliva,
muscle twitching
Neurology
General
awake, alert, not in cardiorespiratory distress
Height: 70 cm Weight: 7.5 kg Length/Ht for age = O
Weight for Age = + 1
Vital Signs
Temperature = 36 C RR = 36 cpm HR = 142 bpm
Skin
(+) brownish desquamation on the chest and trunk
HEENT
normocephalic, pink palpebral conjunctiva, anicteric sclera, non
sunken eyeball, no nasal discharge, (+) erythematous, dry lips and
buccal mucosa, nonhyperemic posterior pharyngeal wall, tonsils not
enlarged, (+) right palpable cervical lymphadenopathies = 1 cm
Chest/Lungs
symmetrical chest expansion, no retractions, clear and equal breath
sounds, no wheezes/crackles
Cardiovascular
normal rate and regular rhythm, no murmurs
Abdomen
globular, no visible pulsations, normoactive bowel
sounds, soft, nontender
Genitourinary
(+) perineal erythema
Extremities
(+) erythematous palms and soles, no cyanosis,
(+) edema dorsa of the hands and foot, pulses full
and equal
KAWASAKI DISEASE
S/P
INTRAVENOUS
IMMUNOGLOBULIN
May 15 (Day 1)
Temp = 36 C RR= 32 cpm HR =
118 bpm
Vital signs
decrease desquamating lesion on
chest and abdomen
Skin:
moist mucosa, improving oral
mucosa (+) CLAD
HEENT
Equal expansion, clear breath
sounds
Lungs
Adynamic precordium, regular rate,
normal rhythm, no murmur
Heart
Perineal erythema, (+) lesions Genitourinary
Slightly edema of hands and feet,
Full equal pulses
Extremities
May 15, 2012
Day 1 afebrile
3-4 episodes of pasty loose stools
Improved activity
Good suck
less irritable
2D echo was done with the follewing
results:
Advised for second round of IVIG
Discontinue Methylprednisolone
Start Dyprimadole 25 mg / tablet,
prepare 6.25 mg papertab twice a
day
Give second dose of IVIG (2g/kg) 6
vials
May 16, 2012 (Day 2)
Temp = 36.3 C RR= 30 cpm HR
= 120 bpm
Vital signs
decrease desquamating lesion on
chest and abdomen
Skin:
Moist lips, improving Oral mucosa,
(+) CLAD
HEENT
Equal expansion, clear breath
sounds
Lungs
Adynamic precordium, regular rate,
normal rhythm, no murmur
Heart
Flabby, not distended, soft, non
tenderNormoactive bowel sounds,
Abdomen
Decreased perineal erythema Genitourinary
Full equal pulses, Extremities
May 16, 2012
Day 2 afebrile
good suck
not irritable
Decided to transfer to other
hospital for IVIG
Take home medications:
Aspirin 100 mg / tablet # 10
(prepare 150 mg papertablet
and give 1 papertablet every
6);
Dipyridamole 25 mg /tablet #
12 (prepare 6-25 mg paper
tablet two doses a day)
5 month old
(+)Bilateral bulbar conjunctival injection, nonpurulent
(resolved)
(+) Changes in the mucosa, dry fissured lips,
strawberry tongue (resolving)
(+) Changes of the peripheral extremities, such as
edema and/or erythema of the hands or feet and
periungual desquamation (resolving)
(+) Rash, primarily truncal; polymorphous but
nonvesicular (resolving)
(+) Cervical adenopathy, lymphadenopathy (1 cm),
uniateral right
35.5
36
36.5
37
37.5
38
38.5
39
39.5
40
40.5
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21
Series 1
May 6 48 (<10
mmol/hr)
May 9 51 (<10
mmol/hr)
May 11 81 (<10
mmol/hr)
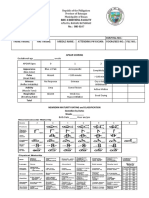
Parameters MAY 6 MAY 9 MAY 11 MAY 14 NORMAL
VALUES
WBC 19.8 23.8 22.3 5.6 5,000-10,000
Henoglobin 9 9.8 9.6 10 12-15
Hematocrit 28 30 30 30 37-45
Segmenters 54 47 50 53 55-65
Lymphocytes 32 36 31 43 26-35
Monocytes 8 17 14 --- 2-6
Eisonophiles 6 6 5 --- 2-4
Platelet 457,00
0
768,00
0
772,00
0
916,000 150,000-400,000
UNIT
Cu. Mm.
g/dl
Vol %
%
%
%
%
Cu. Mm.
Parameters MAY 12 MAY 14
Color Light yellow Yellow
Turbidity Clear Clear
Glucose Negative Negative
Protein Negative Negative
pH 6.0 6.0
Specific Gravity 1.020 1.020
WBC 0-1 0-1
RBC 0-1 0-1
Casts None seen None seen
Parameters Result (May 5)
Color yellowish brown
Consistency Semi-formed
WBC 0-1
RBC 0-1
Baxteria Few
Parasites None
May 6
Blood C/S: no growth after 24 hours of
incubation
May 8
Blood C/S: no growth after 2 days
May 7
There is haziness of the inner lung markings
Impression: Consider Bronhitis. No
consolidation identified.
Normal abdominal sites
Apex on the left
Dilated right coronary artery and left coronary at
0.3 cm proximal and distal
Normal chamber sizes
Minimal pericardial effusion
Good left ventricular systolic function
Left sided aortic arch
Intact interarterial / interventricular septae
Normal cardiac valves and cardiac dimensions
Dilated Left and Right Coronary artery. Left coronary
artery approximately 2.5 to 3.4 mm. The right coronary
artery measures approximately 2.3 to 2.9 mm
There is saccular aneurysm at proximal coronary
artery measuring 3.8 4.3 mm
Good left ventricular systolic function
Small pericardial effusion
No thrombus / vegetation seen
Color flow Doppler study reveal tricuspid regurgitation
and pulmonic regurgitation
Steven-Johnson Syndrome
Age = 5 mos, Prolonged
fever, conjunctivitis,
keratitis, target lesions,
erythema of oral
mucosa,
pseudomembrane
formation
normal extremities, (-)
CLADS, exudative
conjunctivitis, vesiculr
rash with crusting.
associated with Herpes
Virus infection, athralgia
Streptococcal Scarlet fever
Fever = variable usually
10 days; strawberry
tongue, flaky
desquamation,
sandpaper rash, (+) CL,
irritable
Normal eyes, pharyngitis,
positive throat culture for
Group A strep
Rapid clinical response to
appropriate antibiotic
therapy
Measles
High fever, rash , non-
exudative conjunctivitis,
lymphadenopathy,
desquamation severe
cases.
Solitary enlarged
lymphadenopathy, fever
= 5 days only, Koplik
spots and morbiliform
rash
Predisposing factors:
Age-5 mosr old, Sex-Male, Race-Asian
Precipitating Factors:
Unknown yet linked with unknown etiologic agent and environmental factors
Entry of
KD AGENT
Autoimmune Response
Release of Chemical
Mediators
Vasodilation and Cellular
Permeabilty
Attraction of Phagocytes
and WBC
Entry of antigen on
lymphatic capillaries
S/S:
Redness, Swelling, Heat
Phagocytosis by neutrophils and
macrophages (antigens are localized
and inflammation happens
Increase pressure due to
inflammation and entry
of antibodies
Entry of pathogens in the systemic circulation
Regulation of toxins in the body
Release of pyrogen
Stimulation of the hypothalamus
Increase or alteration of thermoregulation
Increase in body temperature
Hyperthermia
Swelling of tissues
Disruption of skin surfaces
Skin desquamation and Rash
Impaired skin integrity
Systemic blood vessels involvement (inflammation of
small & medium size vessels)
If treated:
IVIG
GOOD PROGNOSIS
Refractory symptoms
Give another round of IVIG
If not treated:
Complications developed
Pericarditis
Myocarditis
Cardiomegaly
Myocardial infarction
Heart failure
Ruptured coronary
aneurysym
DEATH
Formerly known as mucocutaneous
lymph node syndrome or infantile
polyarteritis nodosa
Acute febrile vasculitis of childhood
First described by Dr. Tomisaku
Kawasaki in Japan in 1967
Occurs worldwide with Asians at
higher risk
Leading cause of acquired heart
disease in children
Acute, multisystem, self-limited vasculitis
Small-medium vessels: panvasculitis
Age1: 0.5-5 years (90% of cases)
Peak 9-24 months
Male: female = 1.3-1.7:1
Incidence2-4: (per 100,000/yr of < 5 yrs old)
360 for Japanese
95 for Chinese
77 for Hawaiians
56 for Filipino
7 for Caucasians
Recurrence: 1.3-3%
Fever > 5 days + 4/5 criteria of
Bilateral conjunctival injection
Changes in lips and oral cavity
Cervical lymphadenopathy
Polymorphous exanthem
Changes in extremities
Exclusion of other diseases
15-20% of KD1
Age: <1 yr
ESR > 40 mm/hr
CRP > 3 mg/dL
> 3/6 Supplemental Criteria2
Alb < 3 g/dL
Elevate ALT
Anemia for age
Plt after 7d > 450,000/mm3
WBC > 15,000/mm3
UA > 10 WBC/HPF
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Bemonc Admiitting RecordDocument1 pageBemonc Admiitting RecordWiston IlaganNo ratings yet
- Bemonc Admiitting RecordDocument1 pageBemonc Admiitting RecordWiston IlaganNo ratings yet
- Apgar ScoringDocument1 pageApgar ScoringWiston IlaganNo ratings yet
- Provisions - InsuranceDocument26 pagesProvisions - InsuranceWiston IlaganNo ratings yet
- AS and BSDocument1 pageAS and BSWiston IlaganNo ratings yet
- A A A TitleDocument2 pagesA A A TitleWiston IlaganNo ratings yet
- INSURANCE Chapters 1 - 7 by AngelDocument169 pagesINSURANCE Chapters 1 - 7 by AngelWiston IlaganNo ratings yet
- Family Planning DohDocument441 pagesFamily Planning DohWiston Ilagan100% (11)
- 4th Long Exam GyneDocument1 page4th Long Exam GyneWiston IlaganNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- StsDocument10 pagesStsSamonte, KimNo ratings yet
- Indian Institute OF Management, BangaloreDocument20 pagesIndian Institute OF Management, BangaloreGagandeep SinghNo ratings yet
- Addition and Subtraction of PolynomialsDocument8 pagesAddition and Subtraction of PolynomialsPearl AdamosNo ratings yet
- Marijuana Grow Basics - Jorge CervantesDocument389 pagesMarijuana Grow Basics - Jorge CervantesHugo Herrera100% (1)
- A Systematic Scoping Review of Sustainable Tourism Indicators in Relation To The Sustainable Development GoalsDocument22 pagesA Systematic Scoping Review of Sustainable Tourism Indicators in Relation To The Sustainable Development GoalsNathy Slq AstudilloNo ratings yet
- Product Catalog 2016Document84 pagesProduct Catalog 2016Sauro GordiniNo ratings yet
- HP OpenVMS Alpha Version 8.3 and HP OpenVMS Version 8.3-1H1 For IntegrityDocument65 pagesHP OpenVMS Alpha Version 8.3 and HP OpenVMS Version 8.3-1H1 For IntegrityAlexandru BotnariNo ratings yet
- HP 5973 Quick ReferenceDocument28 pagesHP 5973 Quick ReferenceDavid ruizNo ratings yet
- CHB 2Document15 pagesCHB 2Dr. Guruprasad Yashwant GadgilNo ratings yet
- Lab ReportDocument5 pagesLab ReportHugsNo ratings yet
- Center of Gravity and Shear Center of Thin-Walled Open-Section Composite BeamsDocument6 pagesCenter of Gravity and Shear Center of Thin-Walled Open-Section Composite Beamsredz00100% (1)
- AIATS 2021 (OYMCF) Test 01 Offline - Code A - SolutionsDocument34 pagesAIATS 2021 (OYMCF) Test 01 Offline - Code A - Solutionsbhavyakavya mehta100% (1)
- 3.2 Probability DistributionDocument38 pages3.2 Probability Distributionyouservezeropurpose113No ratings yet
- Zhihua Yao - Dignaga and The 4 Types of Perception (JIP 04)Document24 pagesZhihua Yao - Dignaga and The 4 Types of Perception (JIP 04)Carlos Caicedo-Russi100% (1)
- Electrophoresis and Fractionation of Wheat GlutenDocument14 pagesElectrophoresis and Fractionation of Wheat GlutensecucaNo ratings yet
- Understand Azure Event HubsDocument12 pagesUnderstand Azure Event HubselisaNo ratings yet
- National Products Classification Code For Services in IndiaDocument92 pagesNational Products Classification Code For Services in Indiakalanemi0% (2)
- Ipo Exam Revised SyllabusDocument1 pageIpo Exam Revised Syllabusজ্যোতিৰ্ময় বসুমতাৰীNo ratings yet
- VNC Function Operation InstructionDocument11 pagesVNC Function Operation InstructionArnaldo OliveiraNo ratings yet
- Euro4 vehicle diesel engines 199 - 397 kW (270 - 540 hpDocument6 pagesEuro4 vehicle diesel engines 199 - 397 kW (270 - 540 hpBranislava Savic63% (16)
- Flexible AC Transmission SystemsDocument51 pagesFlexible AC Transmission SystemsPriyanka VedulaNo ratings yet
- Riedijk - Architecture As A CraftDocument223 pagesRiedijk - Architecture As A CraftHannah WesselsNo ratings yet
- CV Abdalla Ali Hashish-Nursing Specialist.Document3 pagesCV Abdalla Ali Hashish-Nursing Specialist.Abdalla Ali HashishNo ratings yet
- Understanding Culture, Society and PoliticsDocument62 pagesUnderstanding Culture, Society and PoliticsTeds TV89% (84)
- Android Attendance Management SystemDocument54 pagesAndroid Attendance Management Systemskpetks75% (12)
- Aquafine Optivenn Series Data SheetDocument8 pagesAquafine Optivenn Series Data SheetKenz ZhouNo ratings yet
- EG-45-105 Material Information Sheet (Textura) V2Document4 pagesEG-45-105 Material Information Sheet (Textura) V2GPRNo ratings yet
- AC7114-2 Rev N Delta 1Document34 pagesAC7114-2 Rev N Delta 1Vijay YadavNo ratings yet
- Policies and Regulations On EV Charging in India PPT KrishnaDocument9 pagesPolicies and Regulations On EV Charging in India PPT KrishnaSonal ChoudharyNo ratings yet